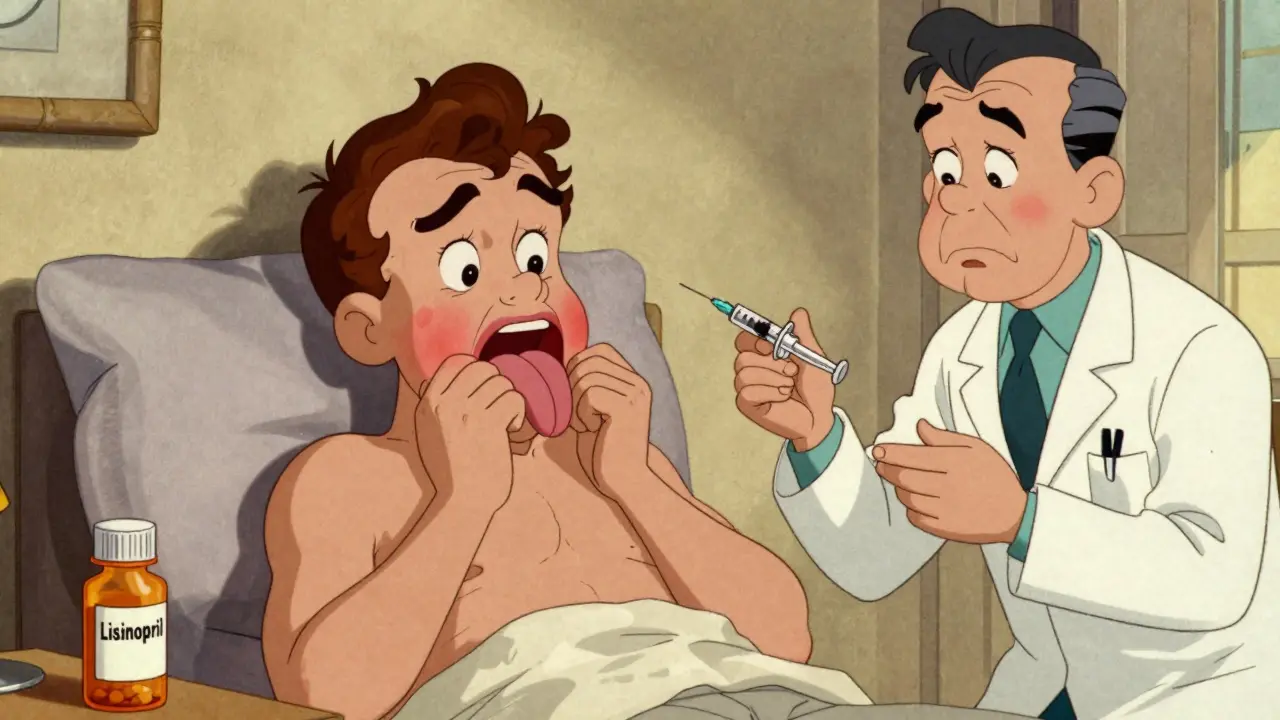
Swelling in your lips, tongue, or throat after starting a new blood pressure pill isn’t just inconvenient-it can kill you. And most doctors don’t recognize it right away. This isn’t an allergic reaction. It’s ACE inhibitor angioedema, a silent, dangerous side effect of one of the most common drug classes in the world. If you or someone you know is on lisinopril, enalapril, ramipril, or any other ACE inhibitor, you need to know the signs, why standard treatments won’t work, and what actually does.
What Exactly Is ACE Inhibitor Angioedema?
ACE inhibitors are prescribed to over 65 million Americans every year for high blood pressure, heart failure, and kidney disease. They work by blocking an enzyme that normally breaks down a substance called bradykinin. When that enzyme is blocked, bradykinin builds up. Too much of it leaks fluid into tissues, causing sudden, deep swelling-especially in the face, lips, tongue, throat, and sometimes the intestines.
This isn’t hives. It’s not itchy. It doesn’t come with a rash. That’s why so many people get misdiagnosed. Emergency rooms treat it like an allergy-epinephrine, antihistamines, steroids. None of it helps. Bradykinin doesn’t respond to those drugs. It’s a different pathway entirely. And if you keep taking the ACE inhibitor, the swelling doesn’t just come back-it gets worse.
Who’s at Risk-and When Can It Happen?
It’s not random. African Americans are 2 to 4 times more likely to develop this reaction. Women are affected more often than men. And it doesn’t care how long you’ve been on the drug. Half of cases show up within the first week. Another 30% show up in the first year. But 20%? They appear after five, ten, even fifteen years of taking the same pill without issue.
One patient in a medical case study developed swelling after 10 years on lisinopril. Another had episodes for four months after stopping it. That’s not a fluke. It’s documented. And if you’re on a diabetes drug like sitagliptin or saxagliptin (DPP-4 inhibitors) at the same time as an ACE inhibitor, your risk jumps 4 to 5 times higher.
Why Standard Allergy Treatments Fail
Epinephrine tightens blood vessels. Antihistamines block histamine. Steroids calm immune responses. All of these work for allergic reactions-hives, anaphylaxis, food allergies. But ACE inhibitor angioedema? It’s driven by bradykinin, not histamine. Giving someone epinephrine for this is like using a fire extinguisher on a leaking pipe. The water keeps coming because the valve’s still open.
Studies from the International Consensus on Hereditary and Acquired Angioedema, the EMCrit podcast, and the MSD Manual all agree: antihistamines, steroids, and epinephrine have no proven benefit here. Continuing them delays real treatment. And in a case where the tongue is swelling shut, every minute counts.
What Actually Works
The only guaranteed fix? Stop the ACE inhibitor-immediately and permanently. No exceptions. No "maybe we can try a lower dose." Once you’ve had one episode, you’re at risk for worse ones. And they can come back even after you’ve stopped the drug, sometimes for months.
For severe cases with airway threat, the gold standard is icatibant (brand name FIRAZYR). It blocks the bradykinin receptor. Symptoms often improve within 2 to 4 hours. It’s not cheap-around $9,000 per dose in the U.S.-but it’s life-saving. Other options include ecallantide (a kallikrein inhibitor) or C1-inhibitor concentrate, both used for hereditary angioedema but sometimes repurposed here.
Fresh frozen plasma has been used off-label because it contains functional ACE enzyme that can break down bradykinin. But evidence is limited to case reports. It’s not a first-line treatment. Airway protection comes first. If breathing is at risk, intubation or even a tracheostomy may be necessary.
What to Take Instead
Once you’ve had ACE inhibitor angioedema, you can never take another ACE inhibitor again. Ever. But you still need to control your blood pressure. The go-to replacement is an ARB-angiotensin II receptor blocker. Drugs like losartan, valsartan, or irbesartan work similarly but don’t interfere with bradykinin breakdown the same way.
But here’s the catch: 10 to 15% of people who had angioedema on an ACE inhibitor will get it again on an ARB. That’s why doctors now monitor closely after switching. If swelling returns on an ARB, the next step is usually a calcium channel blocker or a diuretic. Some patients end up on a combination of two or three different blood pressure meds to get control without triggering swelling.

Why So Many Cases Go Undiagnosed
A 2022 survey by the American College of Emergency Physicians found that only 55% of ER doctors correctly identified ACE inhibitor angioedema on the first visit. Patients often go to the ER three or more times before getting the right diagnosis. One Reddit user shared: "I had swelling for four months after stopping lisinopril. ER doctors didn’t believe it was related because I’d been on it for seven years."
That’s the problem. People assume if you’ve been on a drug for years, it can’t be the cause. But the science says otherwise. The risk doesn’t disappear with time-it just hides.
And even after diagnosis, only 42% of patients get proper counseling about permanently avoiding ACE inhibitors. That means thousands of people are being prescribed these drugs again-sometimes by different doctors, sometimes after a hospital discharge with no clear note in their chart.
What You Should Do Now
If you’re on an ACE inhibitor and notice any of these symptoms:
- Sudden swelling of lips, tongue, or throat
- Difficulty swallowing or speaking
- Feeling like your airway is closing
- No rash, no itching, no hives
Stop the medication. Go to the ER. Tell them: "I think this is ACE inhibitor angioedema. I’m on [name of drug]." Don’t wait for them to figure it out. Bring a list of your meds. Ask if they’ve heard of bradykinin-mediated angioedema.
If you’ve had this happen before, wear a medical alert bracelet. Write "ACEi Angioedema-NO ACE Inhibitors" on it. Make sure your primary care doctor and pharmacist have it documented in your file. Not "allergy." Not "sensitivity." Exact wording matters.
The Future: Screening and Prevention
Researchers are close to identifying genetic markers that predict who’s at highest risk. A 2023 study found a specific variation in the XPNPEP2 gene-responsible for making a key bradykinin-breakdown enzyme-tripling the risk of this reaction. That means someday, before you’re even prescribed an ACE inhibitor, you might get a simple blood test to check your genetic risk.
The European Medicines Agency already recommends extra caution for patients of African descent. In the U.S., experts predict genetic screening for high-risk groups will become routine within five years. Until then, the best protection is awareness. If you’re Black, female, diabetic, or have been on an ACE inhibitor for more than a year, pay attention. Swelling isn’t always an allergy. Sometimes, it’s your body screaming that the drug is wrong for you.
Can ACE inhibitor angioedema happen after years of taking the drug safely?
Yes. While half of cases occur within the first week, up to 20% of people develop swelling after five, ten, or even fifteen years of uninterrupted use. There’s no safe duration-anyone on an ACE inhibitor can experience it at any time.
Do antihistamines or epinephrine help with ACE inhibitor angioedema?
No. These treatments work for allergic reactions caused by histamine, but ACE inhibitor angioedema is caused by bradykinin buildup. Giving epinephrine or antihistamines delays effective treatment and provides no benefit. They should not be used as first-line therapy.
Is it safe to switch to an ARB after having ACE inhibitor angioedema?
ARBs are the most common alternative, but they carry a 10-15% risk of triggering angioedema again. Close monitoring is required. If swelling returns on an ARB, other blood pressure medications like calcium channel blockers or diuretics should be used instead.
How long does swelling last after stopping an ACE inhibitor?
Acute swelling usually resolves within 24 to 48 hours after stopping the drug. But mild episodes can continue for weeks or even months. Some patients report intermittent swelling for up to four months after discontinuation, even with no further exposure to the medication.
Should I get genetic testing for ACE inhibitor angioedema risk?
Not yet as a routine test. But if you’re of African descent, female, or have had unexplained swelling on an ACE inhibitor, ask your doctor about the XPNPEP2 gene variant. Research shows it triples risk, and testing may become standard within the next few years.




12 Comments
So let me get this straight - you’re telling me my grandpa’s been on lisinopril for 12 years, no issues, then one Tuesday his lips swell up like he swallowed a marshmallow and the ER docs just shrug? And the only thing that actually works costs more than my car payment? This isn’t medicine, it’s Russian roulette with a prescription pad.
Ugh. Another ‘educational’ post from someone who clearly never had to explain to their mother why she can’t take her ‘little blue pill’ anymore. Of course African Americans are more at risk - your biochemistry is different, darling. But no one wants to say it out loud because ‘racism.’ Meanwhile, I’m sitting here with my DPP-4 inhibitor and ACE combo, wondering if I’m just a walking time bomb with a South African accent.
I’ve seen this in my village back home - elderly folks on blood pressure meds, swelling like balloons, no one knows why. Doctors blame stress. Family blames karma. No one checks the script. This isn’t just American medicine failing. It’s global silence. I’m sharing this with my aunt in Mumbai. She’s on ramipril. She needs to know.
Stop the ACE inhibitor. Go to the ER. Say the words. Document it. Wear the bracelet. These are not suggestions. They are non-negotiable actions. If you’re reading this and you’re on an ACE inhibitor - act now. Your life depends on it.
The bradykinin cascade is a beautiful, terrifying example of physiological unintended consequences. The renin-angiotensin system evolved to regulate fluid balance, blood pressure, and vascular tone - but pharmacologically inhibiting ACE creates a domino effect where bradykinin, a peptide meant to be transiently active, becomes a runaway signaling molecule. It’s not an allergy - it’s a metabolic trap. And the fact that we still treat it like anaphylaxis speaks to how deeply entrenched dogma overrides mechanistic understanding in clinical practice. We’re treating symptoms, not systems.
ICATIBANT isn’t just a drug - it’s a molecular key to a locked door. It’s like having a fire extinguisher for a chemical leak and finally finding the shutoff valve. The cost is obscene, yes - but so is the cost of misdiagnosis. We’ve turned a physiological quirk into a death sentence because we’re too lazy to learn the biochemistry behind the pill we hand out like candy.
And ARBs? They’re not safe alternatives - they’re probabilistic compromises. A 12% chance of recurrence? That’s not ‘low risk.’ That’s a loaded gun with a 1 in 8 trigger pull. We need better pharmacogenomic screening. We need to stop prescribing by algorithm and start prescribing by biology.
Until then, we’re just rearranging deck chairs on the Titanic - except the Titanic is your airway, and the water is bradykinin.
Of course this is happening. Big Pharma doesn’t want you to know this. They’ve been burying data on bradykinin-mediated angioedema for decades. Why? Because ACE inhibitors are billion-dollar drugs. And if patients knew they could develop life-threatening swelling after 15 years? They’d stop taking them. And then the profits would collapse. You think the FDA really wants this info out there? They’re paid by the same companies that make these pills. Wake up.
Wow. Another one of those ‘I read a medical blog and now I’m an expert’ posts. Let me guess - you’ve never actually seen a patient with this? You just copied and pasted from EMCrit and think you’re doing a public service? Newsflash: most people who get angioedema on ACE inhibitors are already high-risk - elderly, diabetic, Black women. You don’t need a 2000-word essay to tell them to stop the drug. You need better education for *doctors*. And you? You’re just virtue signaling.
I had this. Twice. First time, I thought I was having a stroke. Second time, I was in the ER for 14 hours while three different doctors told me it was ‘just allergies.’ One even said, ‘You’ve been on this for five years - it can’t be the pill.’ I screamed. I cried. I begged. Finally, a resident googled ‘ACE inhibitor angioedema delayed onset’ and saved my life. Now I have a medical alert bracelet. I wear it every day. I tell every new doctor. I post about it. Because if you don’t speak up, they’ll let you die quietly. And no one will care until it’s too late.
And yes - I’m still scared. Even now, five years later. I still wake up some nights with my tongue feeling heavy. I still check my lips in the mirror. I’m not over it. I never will be.
Wait… so if I’m a Black woman on lisinopril and I’ve been taking it for 8 years… and I’ve had weird lip swelling every winter since I started… and my doctor just called it ‘dry air’… and my mom died of choking on her tongue after a similar episode… this is ALL connected? And they never told us? This isn’t medical negligence. This is genocide. They’re killing us slowly with prescriptions. I’m calling my senator. I’m starting a petition. This is bigger than one drug. This is systemic murder disguised as healthcare.
Let’s talk about the elephant in the room: why do we still let white male doctors prescribe these drugs to Black women without a single genetic test? Why is this still considered ‘rare’ when the data says otherwise? This isn’t biology - it’s bias. We’ve been told for decades that Black people ‘tolerate’ meds better. That’s not true. We just die quietly. And now we’re supposed to be grateful when someone finally writes a post about it? We’ve been screaming. No one listened. Now you want a pat on the back for telling us what we already knew?
My sister got this after 11 years on enalapril. She’s fine now, but she had to get intubated. She didn’t know what to say to the ER staff. I wish I’d seen this post back then. I’m sharing it with every Black woman I know who’s on blood pressure meds. You’re not overreacting. You’re not paranoid. You’re just informed. Thank you.
Knowledge is power - but only if it reaches the right people. This post could save a life. Not because it’s fancy or scientific - but because it’s clear. No jargon. No fluff. Just facts. And that’s what matters. If you’re reading this, pass it on. Text it. Email it. Print it. Tape it to your fridge. Someone you love is on an ACE inhibitor right now. And they might not know. Don’t wait for them to swell. Tell them now.
Write a comment