Probiotic Timing Calculator
How to Use This Calculator
This tool helps you determine the best time to take probiotics alongside antibiotics based on your specific schedule. The goal is to maximize probiotic effectiveness while minimizing interference with antibiotic action.
Recommended: Take probiotics 2 hours before or after your antibiotic dose. The most common effective timing is 2 hours after antibiotic intake.
Your Antibiotic Schedule
Your Probiotic Schedule
Optimal Timing Results
Best Strains for Antibiotics
Use Lactobacillus rhamnosus GG or Saccharomyces boulardii for maximum effectiveness against antibiotic-associated diarrhea.
These strains have the strongest clinical evidence and are less likely to be affected by antibiotics.
Duration Recommendation
Continue probiotics for at least 1-2 weeks after finishing antibiotics. For broad-spectrum antibiotics, extend to 3-4 weeks.
Storage Reminder
Keep probiotics refrigerated (unless label specifies otherwise) to maintain potency. Refrigerated probiotics retain 85-90% of live bacteria after 30 days.
When you're on antibiotics, your gut knows it. You might feel bloated, get diarrhea, or just feel off-not because the infection is getting worse, but because the medicine is wiping out good bacteria along with the bad. It’s like a bulldozer rolling through a neighborhood: the criminals are gone, but so are the teachers, the grocers, the doctors. That’s where probiotics come in. But here’s the catch: when you take them matters more than you think.
Why Antibiotics Mess With Your Gut
Antibiotics don’t pick and choose. They hit everything. That’s how they work-they kill bacteria, period. But your gut is home to trillions of bacteria, many of which help digest food, make vitamins, and keep your immune system in check. When antibiotics wipe them out, your microbiome doesn’t just bounce back. Studies show it can take up to two years to fully recover, if it ever does. And during that time, you’re more likely to get diarrhea, yeast infections, or even feel more anxious or tired. That’s not just coincidence-it’s your gut signaling distress.Probiotics: Helpers or Hindrances?
The idea of taking probiotics while on antibiotics sounds smart. Add back the good bugs, right? But science isn’t so simple. Some studies say probiotics help. Others say they delay recovery. One 2018 study in Nature Microbiology found people who took probiotics after antibiotics took 132 days longer to get their original gut bacteria back compared to those who didn’t take anything. That’s almost four months of slower healing. Yet another study in 2024, led by D. John and published in Frontiers in Microbiomes, showed something different: people who took probiotics while on antibiotics had fewer antibiotic resistance genes in their gut. That’s important. Antibiotic resistance isn’t just a hospital problem-it’s happening inside your body. Probiotics might be helping stop that spread. So are they good or bad? The answer: it depends. On the strain. On the timing. On your health.Which Probiotic Strains Actually Work?
Not all probiotics are created equal. Out of hundreds of commercial products, only a handful have solid proof they help with antibiotic-related diarrhea. The two most studied are:- Lactobacillus rhamnosus GG - Proven to reduce antibiotic-associated diarrhea by 26% more than multi-strain blends in a 2022 Cochrane review.
- Saccharomyces boulardii - A yeast, not a bacterium, so antibiotics don’t kill it. Shown to cut diarrhea risk by nearly half in multiple trials.
When to Take Them: The 2-Hour Rule
Timing isn’t just about convenience-it’s about survival. Antibiotics can kill probiotic bacteria if they meet in your stomach or intestines too soon. The fix? Space them out. Harvard Medical School and the American Gastroenterological Association both recommend taking probiotics at least 2 hours before or after your antibiotic dose. Why? It gives the antibiotic time to do its job and move through your system before the probiotic arrives. Here’s what real people do:- Take probiotic at breakfast, antibiotic at lunch → 6-hour gap
- Take probiotic at bedtime, antibiotic in the morning → 12-hour gap
- Take probiotic 2 hours after antibiotic → most common in user polls
How Long Should You Keep Taking Them?
Don’t stop when the antibiotics run out. Your gut is still recovering. Most experts recommend continuing probiotics for at least 1 to 2 weeks after your last antibiotic pill. For broad-spectrum antibiotics (like clindamycin or ciprofloxacin), go longer-up to 4 weeks. The 2024 John study gave probiotics for 28 days after antibiotics ended. That’s a good benchmark. The goal isn’t just to prevent diarrhea-it’s to give your native bacteria time to repopulate without competition from foreign strains.Dosage: More Isn’t Always Better
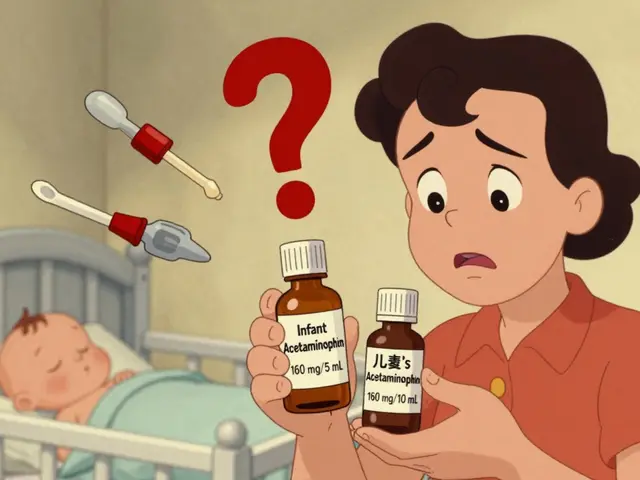
Probiotic labels can be confusing. You’ll see numbers like 5 billion, 20 billion, even 100 billion CFUs (colony-forming units). For most people, 10 to 20 billion CFUs per day is enough. If you’re older, immunocompromised, or have had severe antibiotic side effects before, 20 to 40 billion may help-but talk to your doctor first. Higher doses don’t mean better results. In fact, too many probiotics can cause bloating, gas, or even temporary diarrhea. That’s because some strains produce gas as they work. It’s not a bad sign-it’s just a side effect. Reduce the dose if it bothers you.Storage Matters More Than You Think
Probiotics are living organisms. They die if they get too hot or dry. The most effective strains-like Lactobacillus rhamnosus GG and Saccharomyces boulardii-need refrigeration. Shelf-stable versions might be convenient, but they lose potency faster. A 2023 study found refrigerated probiotics kept 85-90% of their live bacteria after 30 days. Shelf-stable? Only 65-70%. Check the label. If it says “refrigerate after opening,” do it. If it doesn’t say anything, assume it’s not designed to survive long-term at room temperature. Your gut will thank you.
What About Food Instead of Pills?
Yogurt, kefir, sauerkraut, kimchi, miso-these are natural sources of probiotics. But here’s the problem: they usually contain lower, inconsistent doses of bacteria. You’d need to eat a lot to match the 10-20 billion CFUs in a supplement. Plus, many commercial yogurts are loaded with sugar, which can feed bad bacteria. If you love fermented foods, keep eating them. But don’t rely on them alone during antibiotic treatment. Use them as a side dish, not your main defense.Who Should Avoid Probiotics?
Most people can take probiotics safely. But not everyone. If you have:- A weakened immune system (from cancer treatment, HIV, or organ transplant)
- Are critically ill or in the ICU
- Have a central line or catheter
What Do Doctors Really Think?
Here’s the messy truth: doctors don’t all agree. A 2023 survey by the American Gastroenterological Association found 73% of U.S. doctors recommend probiotics with antibiotics. But that’s not because they’re certain it works-it’s because patients ask for it, and the risk is low. The science is still evolving. The 2024 systematic review by Łukasik et al. concluded there’s no clear winner. Some studies show benefit. Others show no effect. A few even show harm. But one thing’s clear: for preventing diarrhea, Lactobacillus rhamnosus GG and Saccharomyces boulardii have the strongest track record.The Bottom Line
You’re not alone if you’re confused. The market is flooded with probiotics. The science is mixed. But here’s what you can do right now:- Choose Lactobacillus rhamnosus GG or Saccharomyces boulardii-no other strains have this level of proof.
- Take your probiotic 2 hours after your antibiotic dose.
- Take it daily for the entire antibiotic course and at least 1-2 weeks after.
- Keep it refrigerated unless the label says otherwise.
- Start with 10-20 billion CFUs. Increase only if needed and with medical advice.
- Stop if you get worse bloating, pain, or fever.
Can I take probiotics at the same time as antibiotics?
It’s not recommended. Antibiotics can kill the probiotic bacteria before they have a chance to work. To protect the probiotics, take them at least 2 hours before or after your antibiotic dose. The most common and effective timing is 2 hours after the antibiotic.
Which probiotic strain is best for antibiotic-associated diarrhea?
Lactobacillus rhamnosus GG and Saccharomyces boulardii have the strongest evidence for reducing antibiotic-associated diarrhea. Lactobacillus rhamnosus GG is especially effective, reducing diarrhea risk by 26% more than multi-strain products in clinical trials. Saccharomyces boulardii is a yeast, so antibiotics don’t affect it, making it a reliable choice during treatment.
How long should I take probiotics after finishing antibiotics?
Continue for at least 1 to 2 weeks after your last antibiotic dose. For broad-spectrum antibiotics like clindamycin or ciprofloxacin, extend it to 3 or 4 weeks. This gives your native gut bacteria time to recover without competition from the probiotic strains you’re taking.
Do I need to refrigerate my probiotics?
Yes-if the label says so, or if it contains Lactobacillus rhamnosus GG or Saccharomyces boulardii. Refrigerated probiotics retain 85-90% of their live bacteria after 30 days. Shelf-stable versions lose potency faster, often dropping below 70%. If you’re serious about effectiveness, keep them cold.
Can probiotics cause side effects?
Yes, but usually mild. Some people experience temporary bloating, gas, or loose stools when they start taking probiotics. This happens because the bacteria are active and producing gases. It usually fades within a few days. If symptoms are severe or last more than a week, stop and talk to your doctor.
Are probiotics safe for everyone?
Most healthy people can take probiotics safely. But if you’re immunocompromised-due to cancer treatment, HIV, organ transplant, or critical illness-you’re at risk for rare but serious infections from probiotic bacteria. Always consult your doctor before starting probiotics if you fall into one of these categories.





14 Comments
Just took my probiotic 2 hours after my antibiotic like the post said - no more bloating. My gut finally feels like it’s not staging a rebellion. 🙌
Let’s be clear: the 2018 Nature study is the only one that matters. Probiotics are a placebo dressed in microbiome jargon. The human gut doesn’t need ‘repopulation’ - it needs time and silence. You’re not fixing a broken engine by dumping in random oils.
And ‘Saccharomyces boulardii’? That’s a yeast. Not a probiotic. It’s a fungal hitchhiker that temporarily suppresses pathogens, not restores balance. This whole industry is built on conflating suppression with healing.
Stop buying into the ‘gut flora’ fairy tale. Your microbiome doesn’t need your help. It needs you to stop poisoning it with antibiotics in the first place.
bro i just chugged a probiotic gummy with my amoxicillin like a boss 🤪
my gut is vibin’
science? pfft. i trust my gut (literally)
They don’t want you to know this but probiotics are a Big Pharma scam to sell you pills while they keep selling you antibiotics.
Why do you think the FDA doesn’t regulate them? Because they’re not drugs - they’re distractions.
And refrigeration? That’s just so they can charge you more. Your kitchen counter is fine. The government just wants you dependent on their ‘science’.
While the data on L. rhamnosus GG and S. boulardii is indeed the most robust, we must acknowledge the heterogeneity in study populations and dosing regimens. The 2024 John et al. paper introduces a critical nuance: the reduction in antibiotic resistance gene load may be a more clinically significant endpoint than diarrhea incidence alone.
Moreover, the 132-day recovery delay in the Nature study may reflect microbial community reassembly dynamics rather than harm - the probiotics may be acting as transient colonizers that facilitate host immune modulation, not permanent reintroduction.
Contextualizing these findings requires systems biology thinking, not reductionist ‘good bug/bad bug’ narratives.
you know what they dont tell you? probiotics are made in china and shipped across the ocean in hot containers… by the time it reaches you, its just sugar dust.
and the ‘2 hour rule’? that’s just a marketing gimmick so you buy more bottles.
just eat yogurt. real yogurt. not that sweet garbage.
Stop being lazy. If you’re taking antibiotics, you’re already compromising your health. Don’t treat probiotics like a magic pill you can swallow while scrolling TikTok.
Refrigerate them. Take them on an empty stomach. Wait two hours. Don’t buy the 100 billion CFU crap. Stick to the strains proven to work. And if you’re still getting diarrhea? See a doctor. Not a supplement aisle.
THIS. RIGHT HERE. I was in the hospital last year on clindamycin for a bad infection. Diarrhea was killing me. Took S. boulardii at 2 hours post-antibiotic - and I swear, I didn’t have one single accident for the whole 10 days.
My nurse said I was the only patient who didn’t need Depends. That’s not luck. That’s science.
DO NOT SKIP THIS. Your future self will thank you.
hi! i’m new to all this but i just started antibiotics and i was so scared of the stomach stuff. this post literally saved me. i bought the l. rhamnosus GG from the health store and i’m keeping it in the fridge like u said 😭
thank u for making it so easy to understand. i feel less alone now
i’ve been taking probiotics for years and honestly? i don’t know if they help. but they don’t hurt. and i like the idea of feeding my gut. 🌱
plus, i eat kimchi every day now. it’s kinda fun. like a little fermented adventure.
also - i refrigerate mine. my cat knocks them off the counter if i don’t. so now they live in the fridge. 🐱❄️
From India - we’ve been eating fermented foods for centuries. No pills needed. Curd, idli batter, kanji - these are natural probiotics. Why are we chasing Western supplements?
Also, most people here don’t even refrigerate. They store it cool, not cold. Works fine. Maybe the ‘refrigeration rule’ is overhyped for Western climates.
Listen. You’re not a lab rat. You’re a human. Your body knows what it’s doing. But if you’re gonna take probiotics - DO IT RIGHT.
Get L. rhamnosus GG. Take it 2 hours after your antibiotic. Keep it cold. Don’t stop after 3 days. And if you feel worse? Stop. No guilt.
This isn’t about being ‘healthy’ - it’s about not being miserable while your body fights a war you started with a prescription.
You got this.
The notion that we can ‘restore’ a microbiome with a pill is a fundamental misunderstanding of ecological systems. The gut is not a garden you can replant. It’s a dynamic, self-organizing network shaped by diet, stress, sleep, and environment.
Probiotics may transiently modulate immune signaling, but they do not ‘recolonize’ the gut in any meaningful way. The 2018 Nature study isn’t just a finding - it’s a warning against technological hubris.
We don’t need to fix what isn’t broken. We need to stop breaking it.
Let’s be real - if you’re taking antibiotics, you’re already part of the problem. Probiotics are just a Band-Aid on a bullet wound.
And don’t even get me started on ‘shelf-stable’ probiotics. That’s like selling frozen pizza as ‘fresh seafood.’
Also - S. boulardii is a yeast. Yeast. Not a bacterium. So why are we calling it a probiotic? It’s not even in the same taxonomic kingdom. This whole field is a semantic dumpster fire.
But hey - if it makes you feel better, go ahead. Just don’t call it science.
Write a comment