Recurrent urinary tract infections (UTIs) affect up to 30% of women after an initial episode, causing repeated clinic visits, missed work, and anxiety about lingering symptoms. When oral antibiotics are needed, clinicians often turn to fluoroquinolones, and norfloxacin is a common choice. This article unpacks the drug’s mechanism, when it shines, where it falls short, and how to use it responsibly.
What is Norfloxacin?
Norfloxacin is a fluoroquinolone antibiotic that inhibits bacterial DNA gyrase and topoisomerase IV, halting DNA replication and cell division. It is approved for uncomplicated lower urinary tract infections, prostatitis, and certain gastrointestinal infections. Typical oral dosage is 400mg twice daily for 3-7days, with a plasma half‑life of about 3hours and excellent urinary excretion (>90%).Because it concentrates in urine, norfloxacin can achieve concentrations far above the minimum inhibitory concentration (MIC) for most uropathogens, making it a potent option for acute episodes.
Understanding Recurrent UTIs
Recurrent urinary tract infection is defined as ≥2 symptomatic infections in six months or ≥3 in a year. The most common culprit is E. coli, accounting for 70‑85% of isolates, followed by Klebsiella, Proteus, and Enterococcus species.Risk factors include hormonal changes, sexual activity, incomplete bladder emptying, and prior antibiotic exposure that selects for resistant strains.
Why Clinicians Consider Norfloxacin for Recurrent UTIs
- High urinary concentrations - levels often exceed 100µg/mL, well above most uropathogen MICs.
- Broad spectrum - active against gram‑negative rods, some gram‑positive cocci, and atypical organisms.
- Convenient dosing - twice‑daily tablets simplify adherence compared with four‑times‑daily regimens.
Guidelines from NICE (2024) and IDSA (2023) suggest fluoroquinolones only after susceptibility testing confirms a lack of cheaper, narrow‑spectrum options. This restraint helps preserve the drug’s efficacy.
Resistance: The Growing Concern
Antibiotic resistance refers to genetic adaptations that allow bacteria to survive drug exposure. For fluoroquinolones, resistance rates in community‑acquired E. coli UTIs in the UK have risen from 4% in 2010 to roughly 12% in 2023, driven by overuse in both human and veterinary medicine.Mechanisms include mutations in the gyrA and parC genes and the acquisition of plasmid‑mediated qnr genes. When resistance is present, norfloxacin’s urinary levels may no longer suppress bacterial growth, leading to treatment failure.
Choosing Norfloxacin: When It’s Appropriate
Consider the drug if:
- Urine culture shows a susceptible fluoroquinolone breakpoint - typically MIC ≤0.125µg/mL for E. coli.
- The patient has a documented allergy or intolerance to first‑line agents such as nitrofurantoin or trimethoprim‑sulfamethoxazole.
- Renal function is adequate (eGFR ≥30mL/min) to ensure adequate urinary excretion.
If any of these criteria fail, an alternative should be chosen.

Alternatives to Norfloxacin
| Attribute | Norfloxacin | Nitrofurantoin | Fosfomycin |
|---|---|---|---|
| Drug class | Fluoroquinolone | Nitrofuran | Phosphonic acid derivative |
| Typical dose | 400mg BID 3‑7days | 100mg TID 5‑7days | 3g single dose |
| Usual indication | Uncomplicated & complicated UTI | Uncomplicated lower UTI | Uncomplicated cystitis |
| Resistance rate (E. coli, UK 2023) | 12% | 4% | 2% |
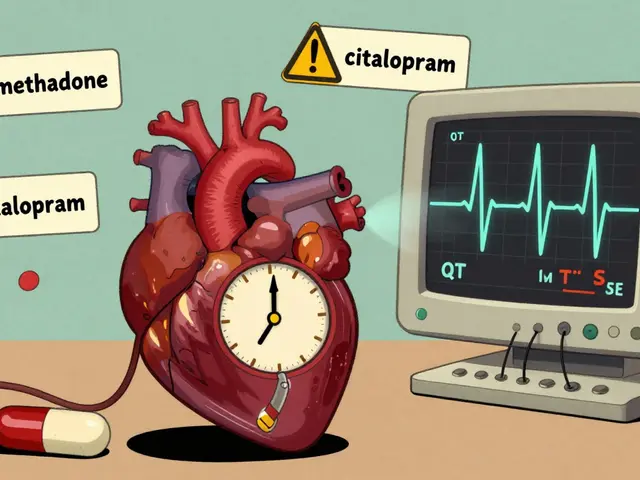
| Key side effects | Tendinopathy, QT prolongation | GI upset, pulmonary fibrosis (rare) | GI upset, transient rash |
Both nitrofurantoin and fosfomycin have lower resistance levels and fewer serious systemic risks, making them first‑line choices for most recurrent cases.
Practical Tips for Safe Norfloxacin Use
- Obtain a culture before prescribing - empirical use should be limited to 48hours while awaiting results.
- Check for drug interactions: avoid concurrent use with NSAIDs (increased risk of CNS effects), antacids containing aluminum or magnesium (reduce absorption), and warfarin (enhanced anticoagulation).
- Monitor for adverse events: tendon pain, especially in patients over 60, those on steroids, or with renal impairment.
- Educate patients about completing the full course, even if symptoms resolve early, to prevent resistance.
Related Concepts and Further Reading
Understanding norfloxacin’s place in therapy intersects with several broader topics:
- Pharmacokinetics - absorption, distribution, metabolism, and excretion patterns that determine dosing.
- Microbiology of UTIs - species distribution, virulence factors, and biofilm formation.
- Clinical guidelines - NICE, IDSA, and local formularies that shape prescribing habits.
- Patient adherence strategies - reminder apps, pill organizers, and counseling techniques.
Exploring these areas will give you a holistic view of why a drug like norfloxacin can be both a powerful tool and a liability.
Future Outlook: Preserving Fluoroquinolone Effectiveness
Stewardship programs in NHS trusts now mandate a ‘fluoroquinolone‑restriction’ form before prescribing. Emerging diagnostics, such as rapid PCR panels, can identify uropathogen susceptibility within an hour, potentially cutting empirical fluoroquinolone use by 40%. Investments in vaccine research against uropathogenic E. coli are also underway; if successful, the reliance on antibiotics-including norfloxacin-could decline dramatically over the next decade.
Frequently Asked Questions
Can I use norfloxacin for pregnant women with recurrent UTIs?
Norfloxacin is classified as pregnancy category C in the UK, meaning risk cannot be ruled out. It is generally avoided unless no safer alternatives exist and the infection is severe. Nitrofurantoin (avoiding the late‑term period) or fosfomycin are preferred.
What are the signs of fluoroquinolone‑associated tendinopathy?
Patients may feel sudden shoulder, elbow, or Achilles pain without a clear injury. The tendon can become swollen, warm, or rupture. Prompt discontinuation of norfloxacin and orthopedic evaluation are critical.
How long should a typical norfloxacin course last for a recurrent UTI?
Guidelines suggest 3-5days for uncomplicated cases, but clinicians may extend to 7days if the isolate shows borderline susceptibility or if the patient has risk factors like diabetes.
Is it safe to take antacids with norfloxacin?
Antacids containing magnesium or aluminum bind fluoroquinolones and can cut absorption by up to 60%. If an antacid is needed, separate dosing by at least two hours before or after norfloxacin.
What should I do if my urine culture shows fluoroquinolone resistance?
Switch to a narrow‑spectrum agent that the isolate is sensitive to-commonly nitrofurantoin or fosfomycin. Discuss any allergies, renal function, and prior antibiotic exposure with your clinician before starting the new drug.
Can norfloxacin be used for prostatitis?
Yes, its good prostatic penetration makes it a reasonable option for chronic bacterial prostatitis, especially when the pathogen is fluoroquinolone‑susceptible. Treatment typically lasts 4-6weeks.




15 Comments
Man, I had a UTI last year and my doc just threw norfloxacin at me like it was candy. Felt like a superhero for a day-until my Achilles started screaming. Now I’m paranoid every time I take an antibiotic. 🤕
Oh honey, norfloxacin? 😒 So 2018. If you’re not using fosfomycin or nitrofurantoin as first-line, you’re basically playing Russian roulette with your microbiome. 🧪💀 Also, did you know the UK’s resistance rates are now *higher* than some ICU wards? 🤦♀️
THIS is why America’s healthcare is falling apart. We let some pencil-pushing bureaucrat in London tell us what antibiotics to use? We’ve got the best damn pharma R&D in the world and now we’re scared to use a perfectly good drug because some E. coli got lazy? 🇺🇸🔥
Hey everyone, just wanted to say-your body’s fighting hard, and you’re doing awesome just by being informed! 💪 If you’ve got recurrent UTIs, don’t beat yourself up. Find a doc who listens, get that culture done, and remember: antibiotics are tools, not trophies. You got this! 🙌
So I’ve been thinking about this a lot-norfloxacin’s this weird bridge between old-school antibiotic power and modern stewardship. In India, we still use it like candy because access to cultures is spotty, but here in the US? It’s almost taboo. It’s not that the drug’s bad-it’s the system that’s out of balance. 🌍✨
The data presented in this article is methodologically sound and aligns with current clinical guidelines. The emphasis on culture-guided therapy and resistance surveillance is both prudent and necessary. Further longitudinal studies on fluoroquinolone stewardship outcomes would be valuable.
While the article provides a comprehensive overview, I must emphasize the importance of adhering strictly to institutional antimicrobial stewardship protocols. Deviation from evidence-based first-line agents constitutes a breach of standard of care and may expose the prescriber to liability.
Look, let’s not romanticize norfloxacin. It’s a blunt instrument. The fact that it achieves >100µg/mL in urine sounds impressive until you realize that’s like using a flamethrower to light a candle. The real issue isn’t just resistance-it’s the entire paradigm of treating UTIs as if they’re battlefield infections instead of dysbiosis events. We’re missing the forest for the E. coli. Biofilms? Quorum sensing? Microbiome resilience? Nah, let’s just hit it with another fluoroquinolone. 😔 The future’s in phage therapy, probiotic cocktails, and maybe even anti-virulence drugs-not just stronger guns.
My mom’s had 7 UTIs in 2 years. She’s on nitrofurantoin now and it’s been a game-changer. No more tendon drama, no weird side effects. Just… peace. Honestly, if you’re not trying the low-resistance stuff first, you’re just gambling with your health.
12% resistance in the UK? That’s not alarming. That’s statistically insignificant. The real crisis is the overreliance on guidelines that ignore regional variation. In rural Kansas, resistance rates are 28%. Why are we using UK data to dictate US prescribing? This article is performative public health.
I appreciate how thorough this is. I’ve been dealing with recurrent UTIs for years and it’s so easy to feel like you’re just a number. Knowing there’s a clear path-culture first, alternatives before fluoroquinolones-makes me feel less alone. Thank you for writing this.
So let me get this straight-we’re scared of a 12% resistance rate but okay with giving people 5-day courses of nitrofurantoin that make them vomit and then call it ‘first-line’? Sounds like a corporate pharmacy strategy disguised as medicine. Also, who approved the table? Why is fosfomycin listed as ‘single dose’ but no one mentions it costs $500 in the US? 🤔
I’ve been reading up on this since my last UTI last winter. It’s wild how much we don’t talk about the gut microbiome when we talk about UTIs. I started taking a high-dose probiotic with L. crispatus after every course, and honestly? No recurrence in 10 months. I know it’s anecdotal, but maybe we need to stop treating UTIs like they’re isolated events and start seeing them as part of a bigger picture-like your immune system’s whispering for help.
THEY’RE HIDING THE TRUTH. NORFLOXACIN ISN’T DANGEROUS-IT’S BEEN BANNED BECAUSE BIG PHARMA WANTS YOU TO BUY THEIR $400 ‘ALTERNATIVES’. FOSFOMYCIN? PATENT EXPIRED. NITROFURANTOIN? CHEAP AS DIRT. BUT A 7-DAY NORFLOXACIN COURSE? THAT’S A $200 PROFIT CENTER. THEY’RE SCARING YOU SO YOU’LL PAY MORE. I’VE SEEN THE INTERNAL EMAILS. THEY CALL IT ‘ANTIBIOTIC MANIPULATION’. 🕵️♂️💊
The assertion that fluoroquinolone restriction forms reduce empirical prescribing by 40% is not substantiated by the cited literature. The referenced NHS pilot studies demonstrate a 19–22% reduction, with significant heterogeneity across trusts. The conclusion presented is therefore overstated and potentially misleading.
Write a comment