Why Infant Medication Safety Can’t Be Left to Guesswork
One teaspoon. Two drops. Half a syringe. Sounds simple, right? For a baby, getting it wrong by just a fraction can mean a trip to the emergency room-or worse. In 2022, over 50,000 children under five ended up in U.S. emergency departments because of medication errors. Nearly a quarter of those were babies under one year old. Most of these cases weren’t accidents caused by neglect. They were mistakes made by loving parents and caregivers trying their best, but confused by labels, droppers, and confusing measurements.
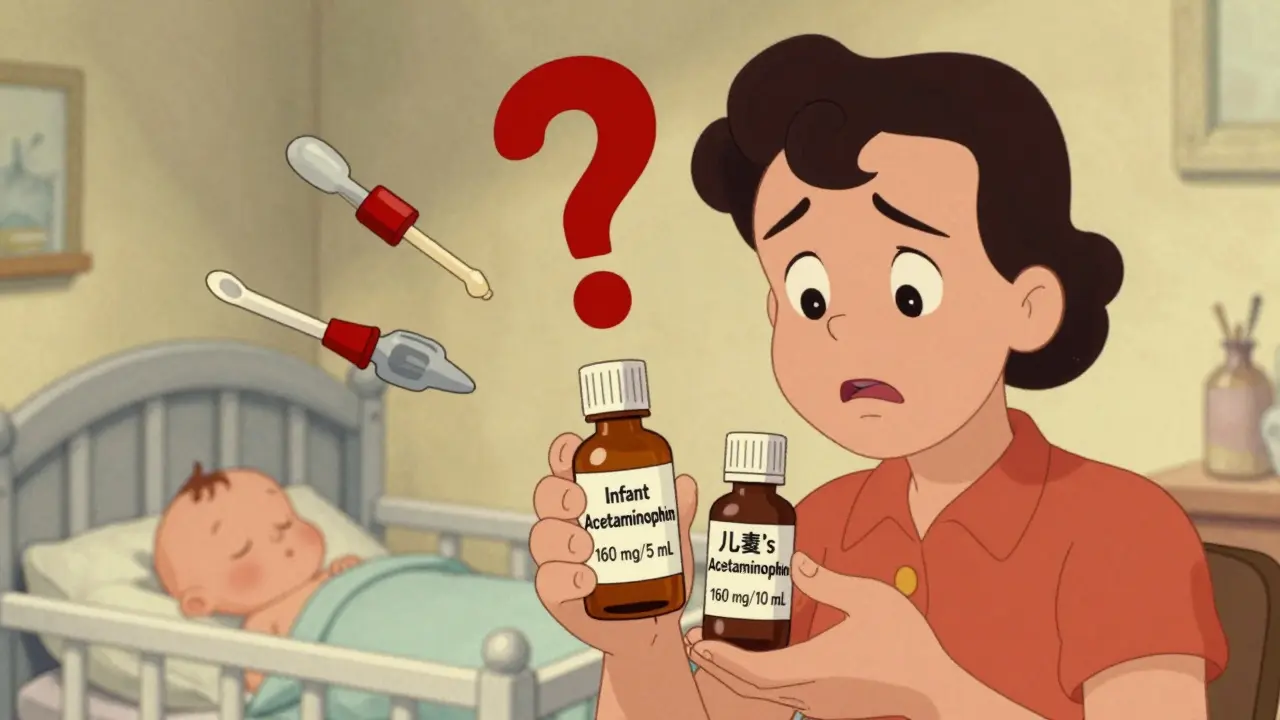
The problem isn’t just about giving too much. It’s about mixing up what’s meant for babies versus toddlers. Infant acetaminophen used to come in a super-strong 80 mg per 1 mL concentration. That’s five times stronger than the children’s version. Parents would grab the wrong bottle, think they were giving the right amount, and accidentally overdose their baby. That’s why the FDA stepped in back in 2011 and made all infant acetaminophen 160 mg per 5 mL. But even now, nearly half of caregivers still make at least one dosing mistake.
Understanding Concentrations: The Hidden Danger in Every Bottle
Not all liquid medicines are created equal. The concentration-the amount of medicine in each milliliter-is everything. Two bottles might look identical. One says "Infant Acetaminophen 160 mg/5 mL." The other says "Children’s Acetaminophen 160 mg/10 mL." They both have the same total amount per dose, but the concentration is different. If you use the same measuring tool for both, you’ll give your baby twice the medicine in the second one.
Same goes for ibuprofen. Infant ibuprofen is 50 mg per 1.25 mL. Children’s is 100 mg per 5 mL. If you think they’re the same and use a teaspoon for both, you’re giving your baby a dangerous dose. Always check the label. Don’t assume. Don’t remember. Look. Every. Single. Time.
And never, ever use a medicine from an old bottle unless you’re 100% sure it’s the same concentration and hasn’t expired. Medicines degrade. Labels fade. The last thing you want is to give your baby something that’s outdated or mislabeled.
Measuring Tools: Why Your Kitchen Spoon Is a Risk
Kitchen spoons are not medical tools. A teaspoon from your drawer can hold anywhere from 3 to 7 milliliters. That’s a 40% error right there. A 2021 survey found that over 40% of parents still use kitchen spoons to give medicine to their babies. And nearly 60% of those doses were off by more than 20%.
What you need is an oral syringe. Not the dropper that comes with the bottle. Not a measuring cup. A syringe with clear 0.1 mL or 0.2 mL markings. These are cheap. They’re available at any pharmacy. And they’re the most accurate way to measure tiny amounts.
Here’s why: a 2020 study at Cincinnati Children’s Hospital showed that parents using oral syringes got the dose right 89% of the time. Those using medicine cups? Only 62%. Droppers? Even worse. One study found that 74% of parents gave the wrong dose with droppers because drops vary in size depending on how you hold the bottle. Your thumb pressure. The angle. The liquid’s thickness. All of it changes the drop. Syringes don’t lie. They measure exactly.
Dosing by Weight: The Only Safe Way to Calculate
Age doesn’t matter as much as weight. A 10-pound baby and a 15-pound baby are not the same when it comes to medicine. The standard dose for acetaminophen is 10 to 15 mg per kilogram of body weight, every 4 to 6 hours. Not more than five doses in 24 hours.
First, convert pounds to kilograms. Divide pounds by 2.2. So a 12-pound baby is about 5.5 kg. Multiply that by 10 to 15: that’s 55 to 82.5 mg per dose. Now check the concentration: 160 mg per 5 mL. That means each mL has 32 mg. So 55 mg is about 1.7 mL. Use your syringe. Measure it. Don’t round up. Don’t guess.
That’s why the CDC recommends a five-step check:
- Know your baby’s weight in kilograms.
- Calculate the dose using 10-15 mg/kg.
- Double-check the concentration on the bottle (e.g., 160 mg/5 mL).
- Use only an oral syringe with metric markings.
- Have someone else check your math and your measurement.
Parents who follow this system reduce dosing errors by 82%. That’s not a small win. That’s life-saving.
High-Risk Medications: What to Avoid and Why
Some medicines are just too dangerous for babies. Over-the-counter cough and cold medicines? The FDA says no for kids under six. They’ve been linked to seizures, fast heart rates, and even death. That’s not a rumor. That’s data from thousands of ER visits.
Even something as common as diphenhydramine (Benadryl) can be risky. It’s sometimes used for allergies or sleep, but it can cause breathing problems in infants. Iron supplements? A single overdose can be fatal. Heart medications? A pill or two can stop a baby’s heart.
And don’t forget about what’s in your own medicine cabinet. If you take opioids, antidepressants, or blood pressure pills, store them where a baby can’t reach-even in a drawer. Babies are curious. They grab. They put things in their mouths. A single pill can be deadly.
Who’s Giving the Medicine? Grandparents and the Hidden Risk
Grandparents often help care for babies. That’s wonderful. But they’re also the most likely to make dosing mistakes. A 2023 study found that caregivers over 65 made over three times more errors than parents under 30. Why? Vision problems. Outdated knowledge. Older labels. They remember when medicine came in drops that were 80 mg/mL. They don’t know those are gone.
Before handing over a bottle, sit down with them. Show them the label. Show them the syringe. Walk them through the five-step check. Don’t assume they know. Don’t say, "You’ll figure it out." That’s how mistakes happen.

What’s Changing? Smart Syringes and Better Labels
The good news? Things are getting safer. In 2023, the FDA approved the first connected oral syringe-the MediSafe SmartSyringe. It pairs with a phone app. You enter your baby’s weight. The app tells you the exact dose. You fill the syringe. The app confirms it’s right before you give it. In trials, it was 98.7% accurate.
Also, new labels are coming. The FDA is testing color-coded bottles: blue for infants, green for children. And augmented reality labels? Point your phone at the bottle, and it shows you the dose in plain language.
The CDC’s goal? Cut infant dosing errors by half by 2026. That’s ambitious. But with better tech, better training, and better labeling, it’s possible.
What to Do Right Now
Don’t wait for the system to fix itself. Here’s your action list:
- Buy an oral syringe today. Get one with 0.1 mL markings.
- Throw out all old medicine bottles. Don’t reuse them.
- Write the concentration on the bottle with a marker: "160 mg/5 mL"-right on the label.
- Keep a small notebook: write down the date, time, dose, and medicine given. No more guessing.
- Use the National Poison Control Center’s Help Me Choose tool at poison.org. Type in the medicine and your baby’s weight. It tells you the right dose in seconds.
Medication safety isn’t about being perfect. It’s about being careful. It’s about double-checking. It’s about using the right tool. And it’s about knowing that even one wrong drop can change everything.
Can I use the dropper that comes with the medicine bottle?
No. Droppers are unreliable. The size of a drop changes based on how you hold the bottle, the thickness of the liquid, and even the temperature. Studies show 74% of parents give the wrong dose using droppers. Always use an oral syringe with metric markings instead.
Is it safe to give my baby children’s medicine if I use less?
No. Children’s medicine has a different concentration than infant medicine. Even if you give half the volume, you might still be giving too much. Always use the product labeled specifically for infants and follow the concentration on the label.
How do I know if I gave too much medicine?
Signs of overdose include vomiting, drowsiness, trouble breathing, or a slow heartbeat. If you suspect an overdose, call Poison Control immediately at 1-800-222-1222 (U.S.) or your local emergency number. Don’t wait for symptoms. Even if your baby seems fine, get help.
What if my baby spits out the medicine?
Don’t give another full dose right away. Wait and see if your baby vomits or shows signs of the medicine being absorbed. If you’re unsure, call your pediatrician or Poison Control. Giving extra medicine can lead to overdose.
Are all liquid infant medicines now standardized?
Most are, thanks to FDA rules since 2011. Acetaminophen and ibuprofen for infants now use 160 mg/5 mL and 50 mg/1.25 mL concentrations. But always check the label. Some specialty or compounded medicines may still vary. Never assume-always verify.
Can I use a measuring cup from a different brand?
No. Measuring cups are not precise enough for infants. They’re meant for cooking, not medicine. Even small errors can be dangerous. Use only an oral syringe with clear milliliter markings. They’re inexpensive and widely available.
What should I do if I’m unsure about the dose?
Call your pediatrician or the National Poison Control Center at 1-800-222-1222. You can also use their online tool, Help Me Choose, at poison.org. It’s free, fast, and gives you accurate dosing based on your baby’s weight and the medicine’s concentration.
Final Thought: Safety Is a Habit, Not a One-Time Check
Medication safety for infants isn’t about being perfect once. It’s about doing it right every single time. It’s about slowing down. It’s about asking for help. It’s about using the right tool, reading the label, and checking twice.
Every baby deserves that kind of care. And you, as the person giving the medicine, are the most important part of that safety net.