Antibiotic Decision Guide
Select Your Situation
Answer these questions to find the best antibiotic option for your case.
Recommended Antibiotics
When a doctor needs to clear up a bacterial infection, choosing the right antibiotic can feel like a guessing game. Cephalexin is a first‑generation cephalosporin that stops bacteria from building their cell walls, making it a go‑to for skin, bone, and urinary‑tract infections. But it isn’t the only option on the shelf. Below you’ll see how Cephalexin stacks up against other popular drugs, when each shines, and what pitfalls to watch out for.
How Cephalexin Works
Cephalexin belongs to the beta‑lactam family, sharing a core chemical ring with penicillins but with a slightly different side chain that gives it a broader reach against Gram‑positive bacteria. By binding to penicillin‑binding proteins, it cripples the bacterial cell wall and leads to rapid cell death. Because it’s absorbed well when taken orally, it’s often prescribed for outpatient treatment.
When Doctors Prefer Cephalexin
- Uncomplicated skin infections such as cellulitis or impetigo.
- Bone infections (osteomyelitis) caused by susceptible organisms.
- Lower‑risk urinary‑tract infections (UTIs) in adults.
- Dental infections where a broad Gram‑positive coverage is needed.
It’s generally safe for most adults and children over six months, but it should be avoided if you have a documented severe allergy to any cephalosporin or penicillin.
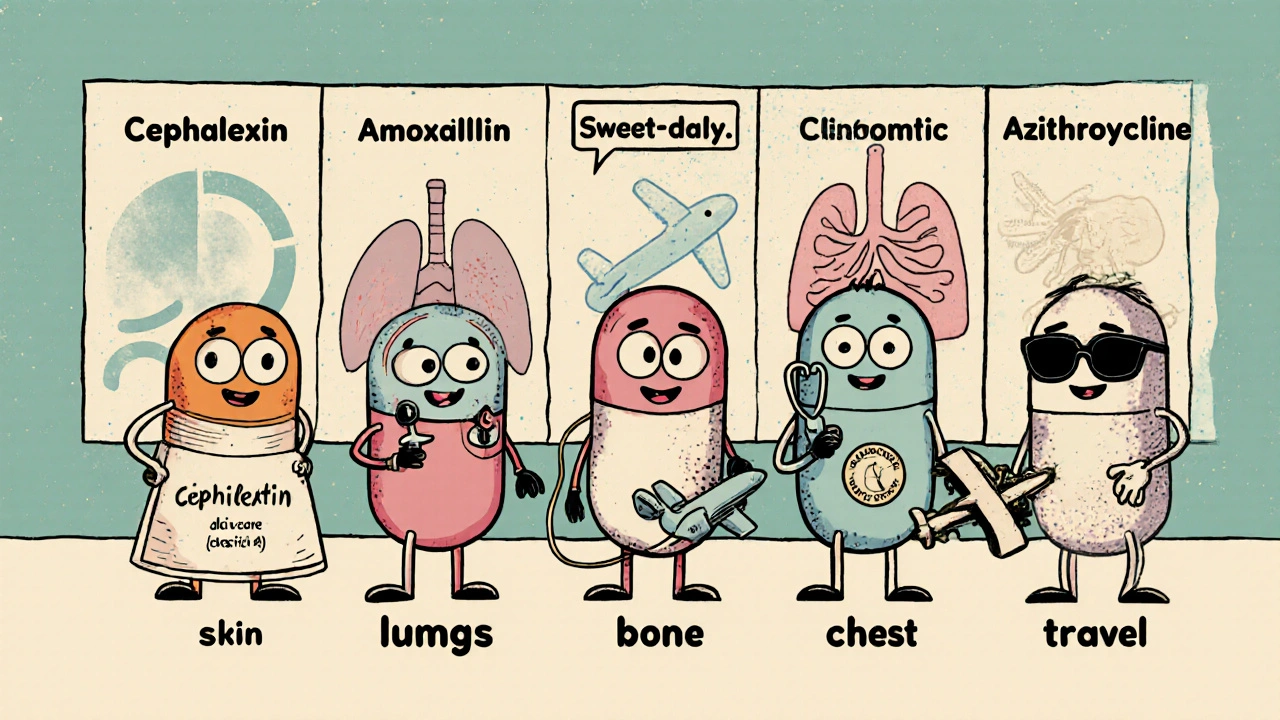
Common Alternatives and Their Sweet Spots
Four antibiotics frequently appear as substitutes for Cephalexin. Each brings a unique spectrum, dosing schedule, and safety profile.
Amoxicillin is a penicillin‑type drug with excellent activity against many respiratory pathogens. It’s favored for ear infections, sinusitis, and certain strep infections.
Clindamycin shines when anaerobic bacteria or resistant Staphylococcus aureus (including MRSA) are suspected. It’s often chosen for deep skin abscesses or bone infections when beta‑lactams might fail.
Azithromycin is a macrolide with a long half‑life, allowing once‑daily dosing. It’s popular for atypical pneumonia, chlamydia, and certain sexually transmitted infections.
Doxycycline is a tetracycline derivative that covers a wide range of bacteria, including atypical organisms and some tick‑borne diseases. It’s the drug of choice for Lyme disease and certain acne treatments.
Side‑Effect Profiles Compared
| Antibiotic | Typical Indication | Primary Spectrum | Common Side Effects | Pregnancy Safety (US FDA Category) |
|---|---|---|---|---|
| Cephalexin | Skin, bone, uncomplicated UTI | Gram‑positive, some Gram‑negative | Diarrhea, nausea, mild rash | B (generally safe) |
| Amoxicillin | Respiratory, otitis media | Gram‑positive, some Gram‑negative | Diarrhea, allergic rash | B |
| Clindamycin | MRSA, anaerobic, deep tissue | Anaerobes, some Gram‑positive | Clostridioides difficile risk, metallic taste | B |
| Azithromycin | Atypical pneumonia, STI | Atypical, some Gram‑negative | GI upset, QT prolongation | B |
| Doxycycline | Lyme, acne, travel‑related infections | Broad (including atypicals) | Photosensitivity, esophageal irritation | D (use with caution) |
Choosing the Right Antibiotic: Decision Checklist
- Identify the suspected pathogen. If the infection is clearly Gram‑positive (e.g., uncomplicated cellulitis), Cephalexin or Amoxicillin are first‑line.
- Assess patient allergies. A history of penicillin allergy may push you toward a non‑beta‑lactam like Doxycycline.
- Consider site of infection. Deep bone or anaerobic infections often need Clindamycin.
- Check pregnancy status. Most beta‑lactams (Cephalexin, Amoxicillin) are safe; Doxycycline is usually avoided.
- Evaluate dosing convenience. Azithromycin’s once‑daily schedule can improve adherence for outpatient care.
Risks and Precautions
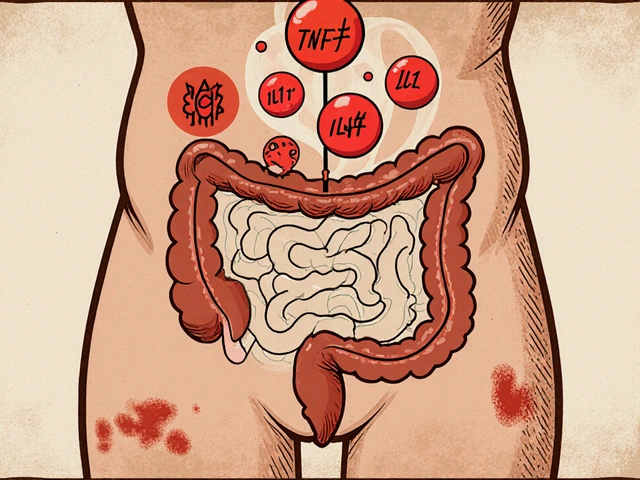
All antibiotics carry the risk of disturbing gut flora, which can lead to Clostridioides difficile infection. This is especially true for broad‑spectrum agents like Clindamycin. Using the narrowest effective drug helps keep this risk low.
Renal impairment changes how Cephalexin is cleared; dose reductions are often needed for patients with a creatinine clearance below 30 mL/min. Likewise, hepatotoxicity is a rare but serious concern with Doxycycline and Azithromycin.
Quick Reference Cheat‑Sheet
- Cephalexin: Best for uncomplicated skin, bone, and urinary infections; safe in pregnancy.
- Amoxicillin: First‑line for most respiratory infections; also safe in pregnancy.
- Clindamycin: Choose for MRSA or anaerobic infections; watch for C. difficile.
- Azithromycin: Ideal for atypical pneumonia and STI; caution with heart‑rate issues.
- Doxycycline: Broad coverage for travel‑related bugs; avoid in pregnancy and when sun exposure is high.
Can I switch from Cephalexin to Amoxicillin if I develop a rash?
If the rash looks like a mild allergy, talk to your doctor first. They may switch you to Amoxicillin, but only if you have no penicillin allergy. Otherwise, a non‑beta‑lactam such as Doxycycline might be safer.
Is Cephalexin effective against MRSA?
Most community‑acquired MRSA strains are resistant to Cephalexin. In those cases, doctors prefer Clindamycin or a newer agent like Trimethoprim‑Sulfamethoxazole.
How long should I take Cephalexin for a skin infection?
Typical courses run 7‑10 days, but your doctor may adjust the length based on infection severity and response to treatment.
Can I use Cephalexin if I’m pregnant?
Yes. Cephalexin is classified as FDA Category B, meaning animal studies have not shown risk and there are no well‑controlled human studies that indicate danger.
What should I do if I miss a dose of Cephalexin?
Take the missed dose as soon as you remember, unless it’s almost time for the next dose. In that case, skip the missed one and continue your regular schedule-don’t double up.



9 Comments
The pharmacodynamic profile of cephalexin, while often lauded in primary care textbooks, is hardly the panacea some clinicians pretend it to be.
Its beta‑lactam ring confers activity primarily against gram‑positive cocci, yet the drug’s spectrum is embarrassingly narrow when faced with the modern menace of resistant organisms.
For uncomplicated cellulitis, the drug may indeed suffice, but the author of this article conveniently omits the fact that community‑acquired MRSA remains a considerable pitfall.
One must also consider the pharmacokinetic nuances: renal clearance dictates dose adjustment, a detail conspicuously absent from the summary.
While the safety chart boasts a category B pregnancy rating, the underlying studies are limited to animal models, a nuance that would interest any discerning prescriber.
Moreover, the table's side‑effect column fails to highlight the relatively high incidence of gastrointestinal upset in patients with pre‑existing dysbiosis.
Comparatively, amoxicillin offers a broader respiratory coverage without the penalty of clostridial overgrowth associated with broader agents.
Clindamycin, albeit infamous for C. difficile, remains indispensable for anaerobic deep‑tissue infections where cephalexin’s reach is insufficient.
Azithromycin’s once‑daily dosing is not merely a convenience but a factor that improves adherence, a point the author glosses over with euphemistic brevity.
Doxycycline, despite its category D label, provides invaluable coverage for atypical pathogens and tick‑borne illnesses, a therapeutic niche cephalexin never enters.
From an antimicrobial stewardship perspective, the recommendation to default to cephalexin without culture data borders on reckless.
In practice, deciphering the optimal agent requires a careful appraisal of the suspected pathogen, patient allergies, comorbidities, and local resistance patterns.
Thus, treating a presumed urinary tract infection with cephalexin in a renally impaired elderly patient is at best ill‑advised.
The article’s checklist is a commendable start, yet it lacks actionable guidance on when to deviate toward a narrow‑spectrum alternative.
In summary, while cephalexin is a valuable tool in the antimicrobial armamentarium, it should be wielded with the precision of a surgeon, not the indifference of a generalist.
Life’s little hurdles remind us that health decisions can be a philosophical adventure. Even when the antibiotic list feels endless, keeping a hopeful mindset helps us navigate the maze. Sure, the nuances can be overwhelming, but you’ll defintely find the right fit with a bit of patience. Remember, every treatment is a step toward recovery, not just a checklist item. Stay positive, and trust the process.
While the preceding optimism is commendable, it neglects the rigorous statistical evidence required for antibiotic selection. The pharmacological literature demands a granular analysis of minimum inhibitory concentrations, a facet conspicuously omitted here. Moreover, the author's reliance on anecdotal experience undermines the requisite methodological robustness. In sum, the discourse would benefit from a deeper evidentiary foundation.
It is essential to acknowledge both the merits and the constraints of cephalexin within the therapeutic spectrum. By fostering a balanced perspective, clinicians can harmonize efficacy with safety considerations. The discourse thus far provides a valuable scaffold, yet further deliberation on patient-specific variables would enhance its applicability. Ultimately, collaborative decision‑making remains the cornerstone of optimal antimicrobial stewardship.
Listen, the whole 'balanced perspective' spiel is just fluff. If you want real results, stop sugar‑coating and pick a drug that actually kills the bug, not some vague 'optimal' nonsense. Cephalexin is fine until it isn’t-then get over it.
Navigating the antibiotic landscape feels like parsing a dense pharmacology textbook after three cups of coffee, doesn’t it? The therapeutic index of cephalexin, while respectable, is eclipsed by the broader spectrum of beta‑lactam agents when polymicrobial flora are suspected. From a stewardship standpoint, the article’s emphasis on narrow‑spectrum usage is laudable, yet the practical realities of patient adherence often dictate a more pragmatic approach. Consider the once‑daily dosing of azithromycin: a pharmacokinetic advantage that translates directly into higher compliance rates. Moreover, the risk of clostridial overgrowth with clindamycin shouldn’t be dismissed as a marginal footnote; it represents a significant safety signal in the real world. While cephalexin’s safety profile is indeed favorable, clinicians must remain vigilant for renal dose adjustments in compromised populations. In essence, the decision matrix is a multidimensional calculus of efficacy, safety, and patient factors-a nuance that the summary only superficially touches upon. So, keep your eyes on the data, not just the drug name on the prescription pad.
Great points! Just remember to match the regimen to the patient's lifestyle, and it'll go a long way.
Honestly, when you start dissecting the myriad of antimicrobial agents available, the sheer breadth of options can feel overwhelming, especially if you’re juggling comorbidities, renal function, and the ever‑present specter of resistance.
Cephalexin, with its respectable gram‑positive coverage, certainly has its place, yet it is not a one‑size‑fits‑all solution, as some overly simplistic guides might suggest.
The pharmacokinetic profile-absorption, distribution, metabolism, and excretion-plays a pivotal role, particularly in patients with fluctuating creatinine clearance where dose adjustments become indispensable.
Moreover, the clinical decision‑making process should incorporate local antibiogram data; ignoring those trends is tantamount to practicing in a vacuum.
It is also worth noting that the drug’s safety in pregnancy, although categorized as B, is derived from limited human data, so prescribers must weigh the risk‑benefit ratio meticulously.
On the other hand, alternatives like doxycycline bring a broader spectrum but introduce concerns such as photosensitivity, which can be a deal‑breaker for patients with extensive sun exposure.
Likewise, azithromycin’s prolonged half‑life offers dosing convenience, yet the potential for QT prolongation cannot be brushed aside.
From a stewardship perspective, narrowing the spectrum to the most targeted agent is ideal, but only after confirming the pathogen via culture whenever feasible.
In practice, many clinicians resort to empirical therapy, and that is where clinical judgement and experience truly shine.
Ultimately, the art of prescribing antibiotics lies in balancing efficacy, safety, patient adherence, and the looming threat of resistance, all while navigating the labyrinthine guidelines that govern modern medicine.
The comparative table, while informative, suffers from a lack of quantitative MIC data, which undermines its utility for precise prescribing. Additionally, presenting pregnancy categories without explicit discussion of teratogenic studies leaves clinicians with an incomplete risk assessment. The omission of cost considerations is another glaring oversight, given that drug pricing heavily influences patient compliance. A more rigorous evaluation would also address the pharmacodynamic targets required for different infection sites. In its current form, the article provides a superficial overview rather than a deep dive.
Write a comment