Doctors love the fast pain relief that Ketorolac Tromethamine is known for, but they also know that a single prescription can become a nightmare if the drug is given to the wrong patient. This guide breaks down every situation where you should say “no” to ketorolac, explains why those red flags matter, and offers practical steps to keep patients safe.
What exactly is Ketorolac Tromethamine?
Ketorolac tromethamine is a potent non‑steroidal anti‑inflammatory drug (NSAID) that blocks the enzyme cyclooxygenase (COX) and stops the production of prostaglandins - the chemicals that drive pain, fever, and inflammation. It’s usually given as an injection or oral tablet for short‑term management of moderate to severe acute pain, especially after surgery. Because it works faster and stronger than ibuprofen or naproxen, it’s often called the “IV ibuprofen” in hospital wards.
How does it work - and why does that create risks?
By inhibiting COX‑1 and COX‑2, ketorolac reduces prostaglandin levels throughout the body. While less prostaglandin means less pain, it also means:
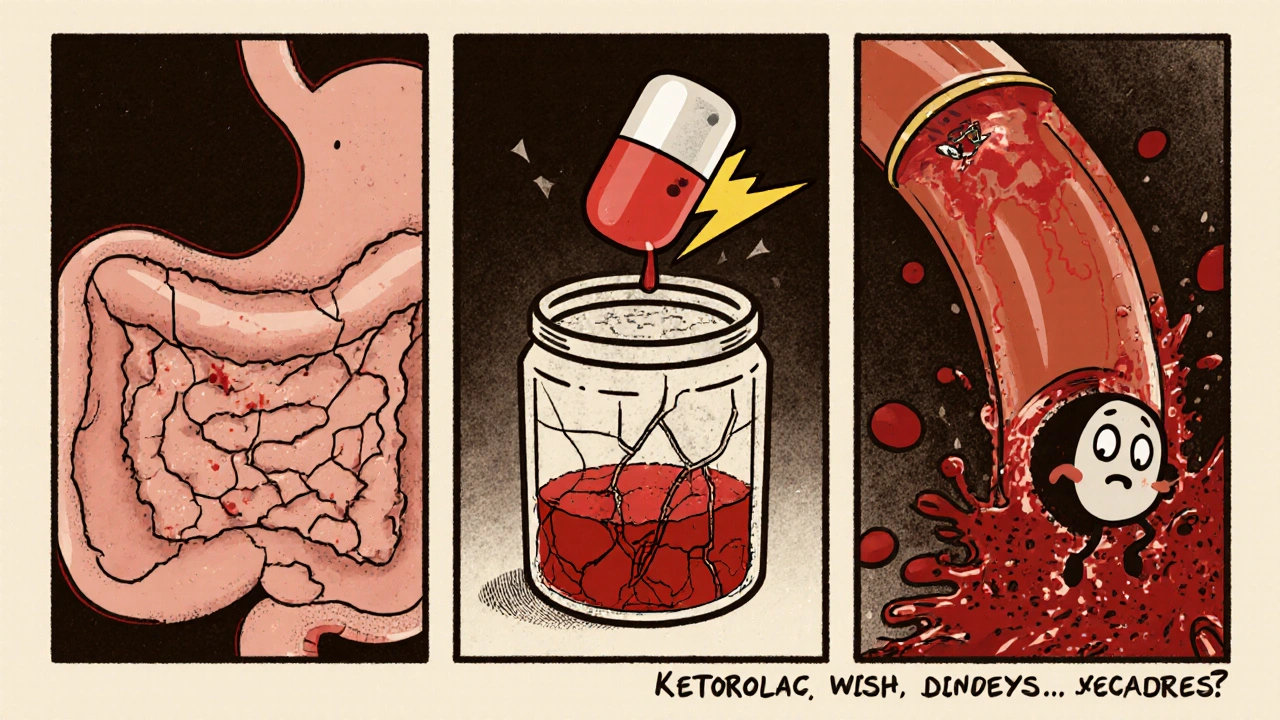
- Reduced protection of the stomach lining, raising the chance of ulcers and bleeding.
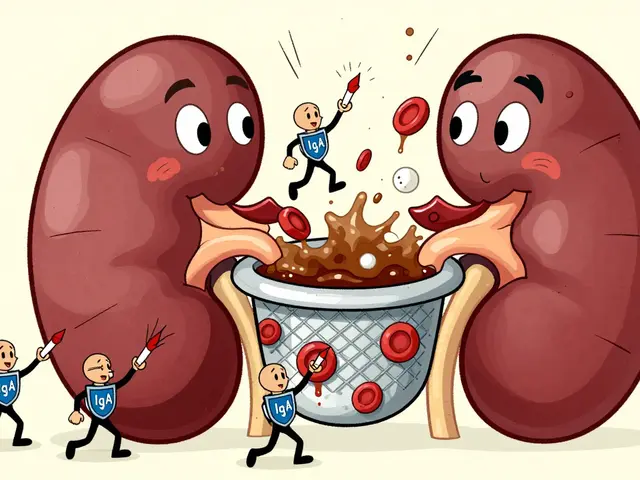
- Lowered blood flow to the kidneys, which can spark acute kidney injury, especially when fluid balance is already shaky.
- Interference with platelet aggregation, increasing bleeding time during surgery or after trauma.
Core Contraindications - The Non‑Negotiable List
The following conditions are absolute contraindications for ketorolac. If any are present, the drug must be avoided entirely:
- Severe renal impairment (creatinine clearance < 30 mL/min) or patients on dialysis.
- Active peptic ulcer disease or a history of gastrointestinal bleeding within the past month.
- Uncontrolled hypertension or known cardiovascular disease that puts the patient at high thrombotic risk.
- Pregnancy after the 20th week (third trimester) and the peripartum period.
- Breastfeeding mothers - ketorolac can pass into milk and affect the infant’s renal function.
- Known hypersensitivity to ketorolac, other NSAIDs, or any component of the formulation.
- Concomitant use of anticoagulants (e.g., warfarin, direct oral anticoagulants) or other drugs that raise bleeding risk.
Why each contraindication matters - a deeper dive
1. Kidney Trouble
The kidneys rely on prostaglandins to keep blood vessels dilated, especially when perfusion is low (think dehydration, heart failure, or sepsis). Ketorolac’s COX inhibition can cause a sudden drop in glomerular filtration rate, leading to acute tubular necrosis. Studies from 2023 show a 4‑fold increase in AKI when ketorolac is given to patients with baseline creatinine clearance under 40 mL/min.
2. Gastro‑intestinal Bleeding
Prostaglandins also maintain the gastric mucosal barrier by stimulating mucus and bicarbonate secretion. Removing that shield can quickly erode the lining, causing ulceration and potentially life‑threatening hemorrhage. A meta‑analysis of 12 trials (2022) reported a 2.2 % incidence of major GI bleed in ketorolac users versus 0.7 % for opioid‑only regimens.
3. Cardiovascular Concerns
While ketorolac isn’t as notorious as COX‑2 selective drugs for heart attacks, it still raises blood pressure and can promote thrombosis by tipping the balance between thromboxane and prostacyclin. Patients with unstable angina, recent myocardial infarction, or uncontrolled hypertension should never receive it.
4. Pregnancy and Breastfeeding
During the third trimester, fetal kidneys start to function, and prostaglandin inhibition can impair that development, leading to oligohydramnios and low birth weight. Post‑delivery, ketorolac passes into breast milk at concentrations that can reduce neonatal urine output. The FDA therefore classifies it as pregnancy category C for the first two trimesters and contraindicated after week 20.
5. Drug Interactions that Heighten Bleeding
Combining ketorolac with anticoagulants, antiplatelet agents (like aspirin or clopidogrel), or SSRIs dramatically increases gastrointestinal and surgical bleeding. The risk climbs from roughly 1 % to over 8 % when both are used together, according to a 2024 longitudinal cohort study in surgical patients.
Who is at higher risk - patient‑specific factors to watch
- Age over 65: kidney function naturally declines and polypharmacy raises interaction chances.
- Dehydration or recent volume loss (vomiting, diarrhea, diuretics).
- History of chronic NSAID use - tolerance may mask early kidney injury.
- Concurrent use of ACE inhibitors or ARBs, which also reduce renal perfusion.
- Obesity and diabetes - both accelerate atherosclerotic disease, making cardiovascular side‑effects more likely.
Safe Alternatives When Ketorolac Is Off‑Limits
If any of the red flags appear, consider these options:
- Acetaminophen (paracetamol) - good for mild‑to‑moderate pain, minimal renal impact.
- Low‑dose opioids - short courses for breakthrough pain, with careful monitoring for dependence.
- Regional anesthesia - nerve blocks or epidurals provide targeted relief without systemic effects.
- Selective COX‑2 inhibitors (e.g., celecoxib) - lower GI risk but still caution with heart disease.
Quick Checklist for Clinicians
- Confirm renal function (eGFR) before ordering ketorolac.
- Ask about recent GI bleeds, ulcers, or NSAID use.
- Screen for pregnancy - a simple urine test if status is unknown.
- Review anticoagulant and antiplatelet therapy.
- Limit total duration to ≤5 days (ideally ≤3 days for IV administration).
- Monitor blood pressure and urine output during treatment.
Summary Table of Contraindications
| Condition | Why it matters | Typical clinical sign |
|---|---|---|
| Severe renal impairment | Reduced prostaglandin‑mediated renal blood flow → AKI | eGFR < 30 mL/min, rising creatinine |
| Active GI ulcer or bleed | Loss of gastric mucus protection → ulceration/hemorrhage | Melena, hematemesis, abdominal pain |
| Uncontrolled hypertension / CV disease | NSAID‑induced sodium retention & thromboxane shift | BP >160/100 mmHg, recent MI, unstable angina |
| Third‑trimester pregnancy | Fetal renal development & prostaglandin inhibition | ≥20 weeks gestation, reduced fetal urine output |
| Breastfeeding | Drug passes into milk, may cause neonatal renal suppression | Infant oliguria, poor weight gain |
| Concurrent anticoagulants | Synergistic effect on platelet function → bleeding | Prolonged PT/INR, unexpected bruising |
| Known NSAID hypersensitivity | IgE‑mediated or non‑IgE reactions can be severe | Urticaria, angioedema, anaphylaxis |
Practical Tips for Managing Pain Without Ketorolac
When you’ve ruled out ketorolac, start with a multimodal approach. Combining acetaminophen with a low‑dose opioid often reaches the same pain scores but with fewer side‑effects. Add a short course of a muscle relaxant if spasms contribute to the discomfort. Physical therapy, ice packs, and elevation can also shave off a few points on the pain scale without a pill.
Common Pitfalls to Avoid
- Prescribing ketorolac beyond five days - risks accumulate sharply after that point.
- Assuming normal renal function based on age alone - always check eGFR.
- Mixing ketorolac with aspirin for “dual pain control” - the bleeding risk skyrockets.
- Skipping pregnancy testing in women of child‑bearing age - a single missed pill can lead to a dangerous exposure.
Frequently Asked Questions
Can I give ketorolac to a patient on ibuprofen?
No. Adding ketorolac to any other NSAID compounds the risk of kidney injury and GI bleeding. If pain isn’t controlled with ibuprofen, switch to ketorolac after a wash‑out period, not stack them.
Is a single IV dose of ketorolac safe for an elderly patient with mild hypertension?
A single 15‑mg IV dose can be acceptable if blood pressure is well‑controlled and renal function is normal (eGFR >60 mL/min). Monitor blood pressure for a few hours afterwards.
What’s the difference between a contraindication and a precaution?
A contraindication means the drug should never be used because the risk outweighs any benefit. A precaution means you can use the drug, but only with extra monitoring or dose adjustments.
Can ketorolac be given to a patient with a history of asthma?
Asthma isn’t a blanket contraindication, but severe hypersensitivity to NSAIDs can trigger bronchospasm. Ask about prior NSAID reactions; if unsure, avoid ketorolac.
Why is the duration limit for ketorolac shorter than for other NSAIDs?
Ketorolac is roughly five times more potent at COX inhibition, so the same dose hits the kidneys and stomach much harder. Limiting use to 3‑5 days curbs cumulative toxicity.
Bottom line: ketorolac tromethamine can knock out pain fast, but it’s a high‑stakes drug. Double‑check those contraindications, keep the treatment window tight, and have a backup plan ready. That way you protect the patient and still get the pain under control.



8 Comments
Wow, the ketorolac guide really pulls together a lot of critical info, and I love how it breaks down each red flag, because that makes it easier for busy clinicians to remember the key points, especially when juggling multiple patients, and the clear tables are a lifesaver, too. The explanation of prostaglandin inhibition, how it protects the stomach lining, and the cascade that leads to renal hypoperfusion, really helped me connect the dots, and I can now explain it to my residents without drowning them in jargon, which is a big win. I also appreciate the emphasis on checking eGFR before prescribing, because kidney function can sneakily decline with age, and catching that early prevents AKI, a complication we all dread. The section on pregnancy and lactation was spot on, highlighting the fetal renal development issue, and reminding us to always run a quick urine test if the gestation is unknown, something I’ll definitely adopt. The drug‑interaction table with anticoagulants is a must‑read, especially given the 8% bleeding risk that the guide cites, which is way higher than many think. I’m glad the guide also lists safer alternatives like acetaminophen and regional blocks, giving us a fallback when ketorolac is off‑limits, and that kind of pragmatic advice is gold. The checklist at the end feels like a perfect quick‑reference for rounding, and I’ve already printed it to stick on my workstation. Also, the reminder to limit therapy to ≤5 days, ideally ≤3 days IV, is a good safety net, because longer exposure ramps up the toxicity curve dramatically. Overall, the tone is supportive, the structure is logical, and the use of bullet points keeps the dense pharmacology digestible, which is exactly what we need in a busy hospital setting. I’m going to share this with my team tomorrow, and I think it will reduce a few near‑misses, especially around the elderly patients with hidden renal impairment. Thanks for pulling all this together, it’s clear a lot of research and clinical experience went into it, and the result is a truly useful tool for anyone prescribing NSAIDs. The mention of dehydration as a risk factor for AKI reminded me of a case last month when a patient’s vomiting led to a rapid rise in creatinine after a single dose, showing how vigilant we must be. Furthermore, the guide’s clear distinction between contraindications and precautions helps prevent over‑cautious avoidance of ketorolac when it could actually benefit a patient, striking a balanced approach. The use of real‑world statistics, like the 4‑fold AKI increase and 2.2% GI bleed rate, grounds the recommendations in evidence, which I find more convincing than vague warnings. I also liked the brief note on asthma, clarifying that it’s not an outright ban but a caution for those with known NSAID hypersensitivity, which clears up a common misconception. Lastly, the inclusion of a quick visual table for contraindications makes it easy to glance during a code, which can be a lifesaver in high‑pressure moments.
It's crucial to double‑check renal labs before hitting the order button, especially in patients over 65, because a hidden creatinine rise can turn a simple analgesic into a kidney hazard.
Hey team, this guide is like a bright compass in the fog of NSAID prescribing – it lights up the “no‑go” zones with vivid clarity and even throws in handy workarounds, so we can keep the pain relief train rolling without derailing patient safety.
Exactly, a quick glance at the checklist can save an entire day of troubleshooting later.
But sometimes the guidelines feel overly restrictive, limiting valuable options for patients who can tolerate short bursts of NSAIDs.
Man, I’ve seen docs throw ketorolac around like candy, and the fallout is brutal – GI bleeds, kidney crashes, and a mountain of paperwork, so shut that reckless habit down and stick to the protocol.
Ugh, the drama of a bleeding ulcer is not what anyone signed up for!
Totally feel you, those hidden bleeds can turn a routine post‑op night into a nightmare, so let’s all keep an eye on the risk factors and call out any red flags early.
Write a comment