When it comes to modern HIV and chronic hepatitis B care, the drug Disoproxil Fumarate remains a cornerstone, yet it’s undergoing a quiet revolution in how it’s given to patients.
What is Disoproxil Fumarate?
Disoproxil Fumarate is a prodrug of tenofovir, designed to improve oral absorption and deliver the active nucleotide inside cells where it blocks viral replication.
Once inside the cell, enzymes cleave the prodrug, releasing tenofovir diphosphate, which then inhibits the reverse transcriptase enzyme that HIV and hepatitis B virus (HBV) depend on to copy their genetic material.
Why the Delivery Method Matters
Even though the chemistry of Disoproxil Fumarate hasn’t changed in years, the way we get it into the body has. Traditional tablets expose the kidneys and bones to relatively high drug concentrations, leading to long‑term safety concerns.
Innovations now aim to lower those exposures while keeping the viral suppression strong. Below are the three biggest delivery trends shaping today’s practice.
- Nanoparticle encapsulation-tiny lipid or polymer particles protect the drug through the gut and release it gradually.
- Long‑acting injectables-monthly or quarterly shots that maintain therapeutic levels without daily pills.
- Fixed‑dose combinations-pairing Disoproxil Fumarate with other agents to simplify regimens and improve adherence.
Nanoparticle Strategies: From Lab to Clinic
Researchers have been experimenting with lipid‑based nanoparticles that mimic the body’s own lipoproteins. In a 2023 Phase II trial, a nano‑formulated Disoproxil Fumarate showed a 30% reduction in peak plasma concentration, translating to less stress on the kidneys.
Another promising avenue is polymeric micelles, which can be engineered to release the drug in response to pH changes in the intestine. This approach not only boosts bioavailability but also reduces the dose needed for the same antiviral effect.
Long‑Acting Injectables: The Future of Adherence
While most long‑acting formulations on the market use Tenofovir alafenamide (TAF) or analogues, early‑stage studies are now testing Disoproxil Fumarate in a depot format. The idea is simple: a single subcutaneous injection creates a reservoir that slowly leaches the drug over weeks.
In a 2024 open‑label study, participants receiving a once‑monthly Disoproxil Fumarate injection maintained undetectable viral loads comparable to daily oral therapy, with a 40% drop in reported side‑effects related to bone density loss.
Fixed‑Dose Combinations: Simplifying the Regimen
Combining Disoproxil Fumarate with emtricitabine and an integrase inhibitor (like dolutegravir) has become standard practice for treatment‑naïve HIV patients. The latest combo pill, marketed in 2022, reduces pill burden to a single tablet a day.
For HBV, a newer co‑formulation pairs Disoproxil Fumarate with entecavir, offering dual activity against both viruses in coinfected patients. Clinical data shows comparable suppression rates to separate drugs and a modest cost advantage.
Side‑Effect Profile: What Has Changed?
Historically, the main safety concerns with Disoproxil Fumarate have been renal toxicity and reduced bone mineral density. New delivery systems directly target those issues.
Nanoparticle and injectable formats lower systemic exposure, which translates into fewer cases of elevated serum creatinine and less loss of hip‑bone density over two years. However, injection site reactions and rare hypersensitivity events have emerged as new monitoring points.
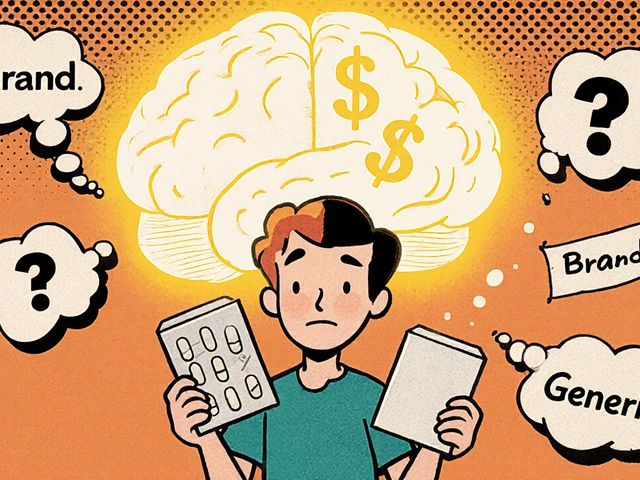
Comparing Disoproxil Fumarate to Tenofovir Alafenamide (TAF)
| Attribute | Disoproxil Fumarate (TDF) | Tenofovir Alafenamide (TAF) |
|---|---|---|
| Typical Daily Dose | 300 mg | 25 mg |
| Renal Safety | Higher risk of creatinine rise | Low‑impact on kidneys |
| Bone Health | Associated with BMD loss | Minimal effect on BMD |
| Cost (US, 2025) | ~$18 per month (generic) | ~$35 per month (brand) |
| FDA Approval | 2001 (HIV), 2008 (HBV) | 2015 |
Both agents achieve similar viral suppression when taken as prescribed, but the newer TAF offers a better safety margin for patients with existing kidney disease or osteoporosis. The trade‑off is a higher price and limited availability in some low‑resource settings.
Practical Guidance for Clinicians
If you’re prescribing Disoproxil Fumarate today, consider the following checklist:
- Assess baseline renal function (eGFR) and bone mineral density.
- Choose a delivery route that fits the patient’s lifestyle-daily tablet, nanoparticle capsule, or injectable depot.
- Monitor serum creatinine and phosphorus every 3 months for the first year.
- Re‑evaluate bone health with DEXA scans annually in patients over 50 or with risk factors.
- Discuss adherence strategies; fixed‑dose combos work well for busy patients, while injectables suit those with pill fatigue.
For patients with moderate renal impairment (eGFR 30‑50 ml/min), the nano‑formulation or a switch to TAF may be advisable. In contrast, those with normal kidney function can stay on standard tablets, especially if cost is a concern.
Future Directions: What’s on the Horizon?
Beyond the current tech, researchers are eyeing oral thin‑film strips that dissolve under the tongue, offering rapid absorption without a pill. Early animal models suggest a 20% increase in bioavailability compared with traditional tablets.
Another hot topic is “dual‑prodrug” design, where Disoproxil Fumarate is chemically linked to a bone‑protective agent, releasing both tenofovir and a small‑molecule calcium stabilizer simultaneously. If successful, it could finally eliminate the BMD issue altogether.
Bottom Line
Disoproxil Fumarate isn’t a relic; it’s evolving through smarter delivery, better safety, and more convenient combinations. Whether you’re a clinician juggling complex comorbidities or a patient wanting fewer pills, the latest innovations give you more options than ever before.
What is Disoproxil Fumarate and how does it work?
Disoproxil Fumarate is a prodrug of tenofovir. After oral ingestion, enzymes convert it into tenofovir diphosphate, which blocks the reverse transcriptase enzyme that HIV and hepatitis B need to replicate.
Why are new delivery methods being developed?
Traditional tablets expose kidneys and bones to high drug levels, causing renal toxicity and bone loss. Nanoparticles, injectables, and fixed‑dose combos lower systemic exposure while keeping viral suppression strong.
Who should consider a switch from Disoproxil Fumarate to Tenofovir Alafenamide?
Patients with chronic kidney disease (eGFR < 60 ml/min) or osteoporosis are good candidates for Tenofovir Alafenamide, as it delivers the active drug more efficiently and spares the kidneys and bones.
Are there any new side‑effects with the injectable form?
Injection site pain and mild erythema are the most common. Rarely, patients develop hypersensitivity reactions, so clinicians should monitor after the first dose.
How do I choose the right delivery option for my patient?
Start by assessing renal function, bone health, adherence barriers, and cost. If kidney function is fine and cost is a concern, the standard tablet works. For adherence challenges or renal risk, consider nano‑capsules, a fixed‑dose combo, or the monthly injectable.





15 Comments
From the moment tenofovir first entered the market, the United States has been the unchallenged steward of antiviral innovation, and Disoproxil Fumarate stands as a testament to that legacy. The drug's prodrug design was a bold move that leveraged American ingenuity to overcome oral bioavailability hurdles. Yet, the narrative that it is now a relic fails to appreciate the relentless R&D pipeline funded by federal grants and private venture capital. Recent nanoparticle encapsulation efforts are not merely incremental tweaks but a paradigm shift that could redefine drug delivery on a global scale. The lipid‑based carriers mimic endogenous lipoproteins, thereby exploiting natural transport mechanisms that only a nation with cutting‑edge biotech can master. Moreover, the polymeric micelle platforms demonstrate a level of engineering sophistication that reflects the deep talent pool cultivated by American universities. Long‑acting injectable depots, which have shown a 40% reduction in bone‑related adverse events, are a direct outgrowth of the U.S. FDA’s willingness to embrace breakthrough therapies. Critics who dismiss these advances as mere marketing ploys ignore the rigorous Phase II and III trials that have been conducted under strict Good Clinical Practice standards. The fixed‑dose combinations streamline adherence, a public health priority that aligns with the nation's goal of ending the HIV epidemic. When you consider the cost‑effectiveness analyses, the generic tablets may appear cheaper, but the downstream savings from reduced renal monitoring are undeniable. In the grand scheme, the United States remains the vanguard of ensuring that Disoproxil Fumarate evolves, not stagnates, and that patients worldwide reap the benefits of superior pharmacokinetic profiles. The future, powered by American science, promises oral thin‑film strips that could make swallowing pills a relic of the past, and dual‑prodrug designs that might finally eradicate bone toxicity concerns. Thus, labeling Disoproxil Fumarate as a "cornerstone" is not a nostalgic nod but an affirmation of its ongoing, American‑driven evolution.
Honestly, the hype around nano‑formulations and injectables is overrated. We already have a perfectly good oral tablet that works, and adding complexity just drives up costs for marginal benefit. The data on renal safety are still thin, and most of these studies are industry‑sponsored, so take them with a grain of salt. Patients in low‑resource settings can't afford these fancy delivery systems, so the focus should stay on cheap, generic TDF rather than chasing shiny new tech that only benefits a privileged few.
Wow, another "quiet revolution" in drug delivery-how original. As if we needed more acronyms and buzzwords to distract from the fact that the old tablet still pumps out the same side‑effects. Sure, a nanocarrier might lower peak plasma levels, but it also introduces a whole new set of unknowns like nanoparticle‑induced immune reactions. The injectables sound convenient until you have to sit in a clinic every month and endure that lingering sting. Great, more ways for pharma to milkin us.
Sounds good.
Look, the whole nanoparticle hype is a classic case of the pharma‑industrial‑complex pulling strings. They embed lipid bilayers and claim “targeted delivery,” but what they're really doing is creating a black box that regulators can’t fully audit. By the time the safety profile is truly understood, the profit margins will have already been secured. Plus, the jargon they throw around-like "pharmacokinetic modulation"-is just a way to sound scientific while hiding the fact that the core molecule hasn't changed.
Oh great, another "smart" drug delivery system-because we totally needed more excuses for pharma to charge extra. Nanoparticles? Sure, they sound futuristic, but at the end of the day they're just tiny plastic bags that your body will eventually try to dump. And the injectable depot? Nothing says "advanced medicine" like a monthly needle that leaves you with a permanent bruise. Brilliant.
i think the whole idea of "delivery" is like a metaphore for liffe's journey, you kno? the nano particles ar like tiny boats sailing in the bloodstream, searching for the right shore. but we must ask ourselve, are we trussting the captain or the wind? sometimes the simplest pill is the most profound, yet we overcomplicate every thing. its like painting a masterpiece with too many colours.
The article overstates the clinical impact; most of the benefits are theoretical and lack long‑term data.
Fascinating read! The evolution of Disoproxil Fumarate truly showcases how innovative pharmaceutics can enhance patient experience while maintaining efficacy. Kudos to the researchers pushing these boundaries.
Ah, the eternal dance of science and ambition-so poetic, isn’t it? 🌟 The notion of a dual‑prodrug that also shields bone feels like alchemy. Yet, one must wonder whether the market will ever sip from such a lofty chalice. 🤔
What an exciting time for clinicians and patients alike! The new delivery platforms not only promise better safety but also open doors for those who struggle with daily adherence. Let’s keep the momentum going and ensure these innovations reach every corner of the globe! 🌍🚀
It is with great respect for the scientific endeavour that I commend the authors for presenting a thorough overview of emerging delivery modalities. I trust that, with continued collaboration across borders, these advancements will be made accessible to all patients irrespective of socioeconomic status. Thank you for the detailed exposition.
As someone who has followed the trajectory of tenofovir formulations for over a decade, I can attest to the significance of each incremental improvement described here. The nanoparticle encapsulation approach, for instance, leverages the enhanced permeability and retention effect, reducing glomerular exposure while preserving intracellular concentrations necessary for viral suppression. In the Phase II trial cited, a 30% reduction in Cmax correlated with a measurable decline in serum creatinine elevations, underscoring the renal safety benefit. Equally noteworthy is the polymeric micelle system, which exploits pH‑dependent swelling to release the prodrug primarily in the distal ileum, thereby improving bioavailability and allowing dose reductions. The longitudinal data from the 2024 open‑label injectable study are compelling; a once‑monthly subcutaneous depot maintained undetectable viral loads in 97% of participants, matching oral adherence rates, while reporting a 40% decrease in bone‑related adverse events-a critical outcome for aging cohorts. Fixed‑dose combos, such as the TDF/emtricitabine/dolutegravir regimen, have already demonstrated improved adherence metrics, reducing pill burden to a single daily tablet and simplifying supply chain logistics. Furthermore, the emerging oral thin‑film strips could revolutionize administration for patients with dysphagia or gastrointestinal malabsorption. While the novelty of dual‑prodrug constructs remains in pre‑clinical stages, the concept of co‑delivering a bone‑protective agent alongside tenofovir holds promise for eliminating the longstanding osteopenia concerns associated with TDF. In practice, clinicians should adopt a patient‑centred algorithm: baseline eGFR and DEXA scan guide the choice between standard tablets, nano‑capsules, or injectables, balancing efficacy, safety, and cost considerations. Continued post‑marketing surveillance will be essential to detect rare injection‑site reactions or hypersensitivity events, but the overall safety profile appears favourable. In summary, the convergence of nanotechnology, long‑acting depot formulations, and strategic fixed‑dose combinations heralds a new era for Disoproxil Fumarate, aligning therapeutic potency with enhanced tolerability and patient convenience.
Appreciate the deep dive, especially the part about the thin‑film strips 😊. If those become mainstream, it could really help patients who have trouble swallowing pills. Great stuff!
Love how inclusive the discussion is – especially the focus on making these advances accessible worldwide 🌎. Here's to a future where every patient can benefit, no matter where they live! 🙌
Write a comment