Every year, over 23,000 people end up in the emergency room because a supplement they took messed with their prescription medication. That’s not a rare accident. It’s happening to people just like you-someone taking a multivitamin, fish oil, or St. John’s wort because they think natural means safe. But that’s not true. And if you’re on any kind of regular medication, you need to know how to check if your supplement is safe.
Why Supplements Can Be Dangerous with Medications
Supplements aren’t tested the same way as prescription drugs. Under the 1994 Dietary Supplement Health and Education Act, companies don’t have to prove their products are safe before selling them. That means a bottle labeled “immune support” or “natural energy booster” could contain ingredients that interfere with your blood pressure pills, antidepressants, or even birth control. The biggest problem? Drug metabolism. Your liver uses enzymes-especially the CYP3A4 and CYP2C9 systems-to break down medications. Some supplements can block or speed up these enzymes. For example, St. John’s wort speeds up CYP3A4, which means drugs like cyclosporine (used after organ transplants) get cleared from your body too fast. Studies show this can reduce cyclosporine levels by up to 50%, putting transplant patients at risk of rejection. Other interactions work differently. Calcium, magnesium, and iron all compete for the same absorption spots in your gut. Taking them together can mean none of them work well. Warfarin, a blood thinner, is especially dangerous. Vitamin E at 400 IU or higher can raise your INR by 15-20%, increasing bleeding risk. Ginkgo biloba does the same thing, and combined with Eliquis or Plavix, it’s led to hospitalizations for internal bleeding.High-Risk Supplements You Should Avoid
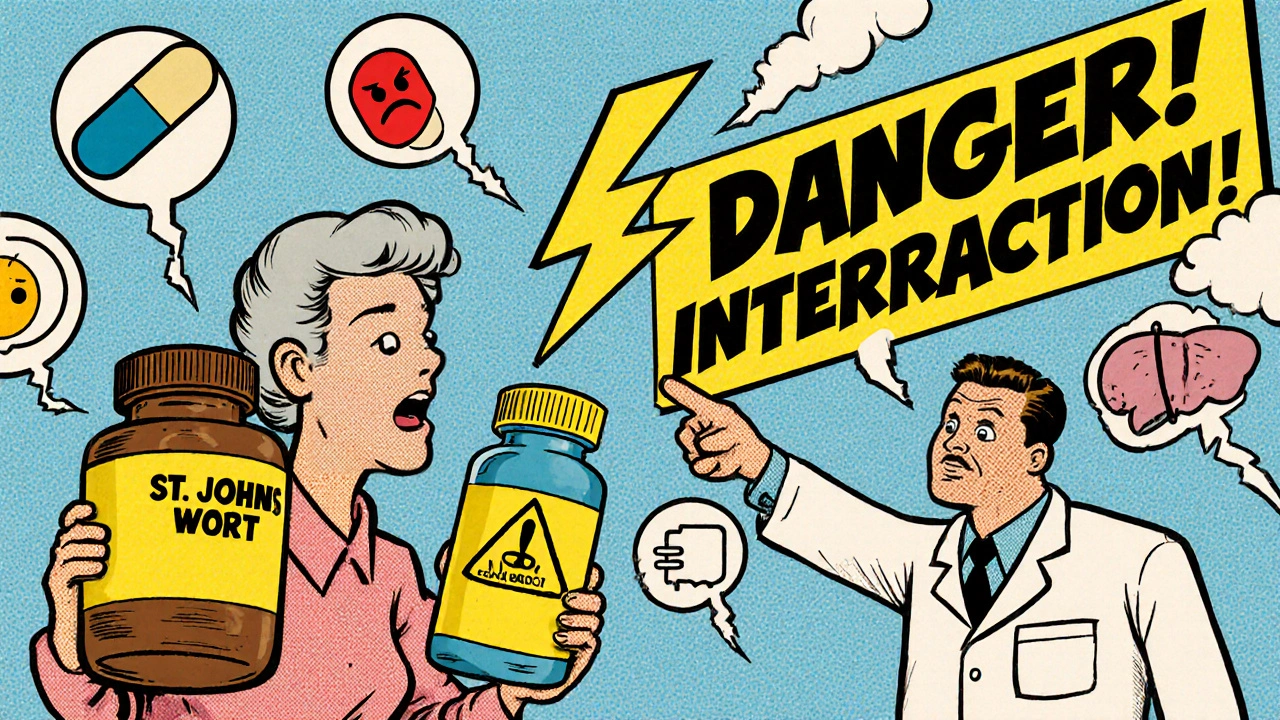
Not all supplements are created equal. Some are low-risk. Others? They’re ticking time bombs when mixed with common meds.- St. John’s wort: This one interacts with over 57 prescription drugs. It reduces the effectiveness of birth control, HIV medications, antidepressants (SSRIs), and heart drugs like digoxin. It’s also linked to serotonin syndrome-a potentially deadly condition caused by too much serotonin in the brain.
- Ginkgo biloba: Safe for most people, but dangerous with blood thinners. Studies show it increases bleeding risk by 2.3 times when taken with warfarin.
- Vitamin E (400 IU+): Raises INR levels in people on warfarin. Even if you’re not on blood thinners, high doses can interfere with chemotherapy drugs.
- Garlic, ginger, and fish oil: These all have mild blood-thinning effects. Surgeons require patients to stop them 7-10 days before surgery. Skipping this step can lead to uncontrolled bleeding.
- Goldenseal: Blocks liver enzymes the same way St. John’s wort does, but less predictably. It can raise levels of drugs like metformin and statins, increasing side effects.
Low-Risk Supplements (But Still Check)
Some supplements rarely cause issues. That doesn’t mean they’re risk-free-it just means the chances are much lower.- Milk thistle: Only 3 documented interactions in the last 10 years, mostly with drugs processed by CYP2C9.
- Cranberry: Often blamed for warfarin interactions, but recent studies show it’s unlikely to cause problems at normal doses.
- Black cohosh, American ginseng, saw palmetto, valerian: These have minimal evidence of interaction with common medications.
How to Check for Interactions: A Simple 3-Step System
You don’t need to be a pharmacist to protect yourself. Just follow this:- Make a full list. Write down every prescription, over-the-counter drug, and supplement you take-including doses and how often. Don’t forget things like herbal teas, CBD oil, or probiotics. Many people forget these.
- Bring it to your next appointment. Use the “brown bag method.” Put everything in a bag and take it to your doctor or pharmacist. A Johns Hopkins study found this reduces medication errors by 37%. Pharmacists at Walgreens and CVS now screen for interactions during every consultation. In 2021, they caught dangerous combos in 18% of cases.
- Check the label. Look for three things: active ingredients, amount per serving, and any warning statements. If it says “May interact with blood thinners” or “Avoid with antidepressants,” take it seriously. If there’s no warning, that doesn’t mean it’s safe-it just means the manufacturer isn’t required to say anything.
What to Do If You’re Already Taking a Risky Combo
If you’ve been taking St. John’s wort with your antidepressant, or ginkgo with Eliquis, don’t panic. But don’t ignore it either. Stop the supplement immediately. Call your doctor or pharmacist. Don’t wait for your next appointment. If you’re on warfarin and started taking vitamin E, get an INR test right away. If you’re on birth control and take St. John’s wort, use backup contraception until you talk to your provider. A 2023 survey found 68% of supplement users never tell their doctor. That’s the real danger-not the supplement itself, but the silence around it.




14 Comments
Man, I never thought about how fish oil could mess with my blood pressure meds. I’ve been taking it for years thinking it was just ‘heart healthy.’ Guess I’m bringing my whole supplement drawer to my next appointment. Thanks for the wake-up call.
You’re lucky you’re not dead yet. People like you think ‘natural’ means ‘no consequences.’ St. John’s wort with antidepressants? That’s not a mistake-that’s a death wish. Get your head out of the clouds.
This is one of those posts that should be mandatory reading before anyone buys a supplement. I used to think ginkgo was just ‘brain fuel’-turns out it’s basically a blood thinner with a fancy label. I’m switching to milk thistle now. Thanks for the clarity.
I work in a pharmacy, and I can’t tell you how many times I’ve seen people walk in with a bag full of supplements they got from a ‘wellness influencer’ on Instagram. One guy was taking goldenseal with his statin-and didn’t even know what statins were. The FDA’s new app is a start, but we still need better education. Pharmacists aren’t just pill dispensers-we’re your last line of defense. Ask us. Seriously. We’ve seen it all. And no, ‘it’s just herbal’ doesn’t cut it.
The epistemological fallacy inherent in the conflation of ‘natural’ with ‘safe’ is a persistent cultural pathology. One must interrogate the ontological status of pharmacological agency in botanical substances, particularly when their metabolic pathways intersect with synthetic pharmaceuticals. The regulatory lacuna under the 1994 DSHEA Act exemplifies a neoliberal abdication of public health stewardship.
Just wanted to add: if you’re on warfarin, don’t just avoid ginkgo and vitamin E-watch your kale intake too. Vitamin K flips your INR like a switch. And probiotics? Some strains can affect how your body metabolizes meds-especially antibiotics. I always tell patients: write down EVERYTHING-even the chamomile tea you drink before bed. And yes, CBD counts. I’ve seen it lower the effectiveness of seizure meds. Don’t guess. Check. And if you’re unsure? Call your pharmacist. They’re paid to answer these questions.
So now I'm supposed to stop taking turmeric because it might thin my blood? What's next? Are we gonna ban water because it might cause a stroke if you drink too much? This is fearmongering. I'm 65 and I've been taking supplements for 20 years and I'm still standing. Your doctor is just trying to sell you more pills
Bro, this is gold. In India, everyone just buys supplements from the local pharmacy without asking anything. I showed this to my uncle-he was taking ashwagandha with his thyroid med. He didn’t even know it could mess with his TSH levels. Now he’s asking his doctor. Small wins.
It’s not about fear. It’s about awareness. We’re taught to trust nature, but we’re never taught how nature interacts with modern medicine. That gap? That’s where people get hurt. I used to think St. John’s wort was just ‘natural Prozac.’ Now I know it’s more like a silent saboteur. Knowledge isn’t scary-it’s power.
I cried reading this. My mom had a bleed in her brain last year because she was taking ginkgo with Eliquis and didn’t tell anyone. She thought it was ‘just a memory pill.’ We’re lucky she made it. Please, if you’re reading this-tell your doctor. Even if it feels dumb. Even if you think they’ll judge you. They won’t. They’ve heard it all.
so like... if i take vitamin c with my abilify, am i gonna die? or is that just another fear tactic? also can i still drink green tea? idk anymore
Thank you for writing this. I’m a nurse, and I’ve seen too many patients come in with bleeding, liver issues, or organ rejection because they didn’t tell anyone about their supplements. It’s not about being paranoid-it’s about being smart. I give this article to every new patient who takes anything beyond a daily multivitamin. And yes, even ‘harmless’ things like melatonin can interfere with diabetes meds. You’re not alone in wondering-just don’t wonder alone.
Ugh. Another ‘don’t take anything’ post. I’ll take my fish oil and my ginkgo and my turmeric and keep living. I’m not some lab rat for Big Pharma.
Just saw your comment about turmeric. It’s not about dying-it’s about your INR creeping up slowly until your doctor’s like, ‘Why is your blood so thin?’ Turmeric can increase bleeding risk, especially with blood thinners. Green tea? Low risk unless you’re drinking a gallon a day. But if you’re on antipsychotics like Abilify? The caffeine might make you jittery, but the herbals? Not a big interaction. Still-tell your doctor. Always.
Write a comment