When a generic drug company submits an Abbreviated New Drug Application (ANDA) to the FDA, they’re not just asking for permission to sell a cheaper version of a brand-name drug. They’re asking the FDA to confirm that their product is therapeutically equivalent-same active ingredient, same strength, same dosage form, and same performance in the body. But more than half of these applications don’t pass the first review. Instead, they get a deficiency letter.
A deficiency letter isn’t a rejection. It’s a detailed checklist of what’s missing, wrong, or unproven. And for companies trying to bring affordable medicines to market, these letters can delay approval by over a year-and cost millions. The FDA doesn’t issue these letters lightly. They’re the result of rigorous scientific review across chemistry, manufacturing, bioequivalence, and toxicology.
What’s Most Often Missing in Generic Drug Applications?
Over 70% of major deficiencies in ANDAs are quality-related. That means the problem isn’t usually about whether the drug works-it’s about whether the FDA can be sure it will work the same way every time, batch after batch.
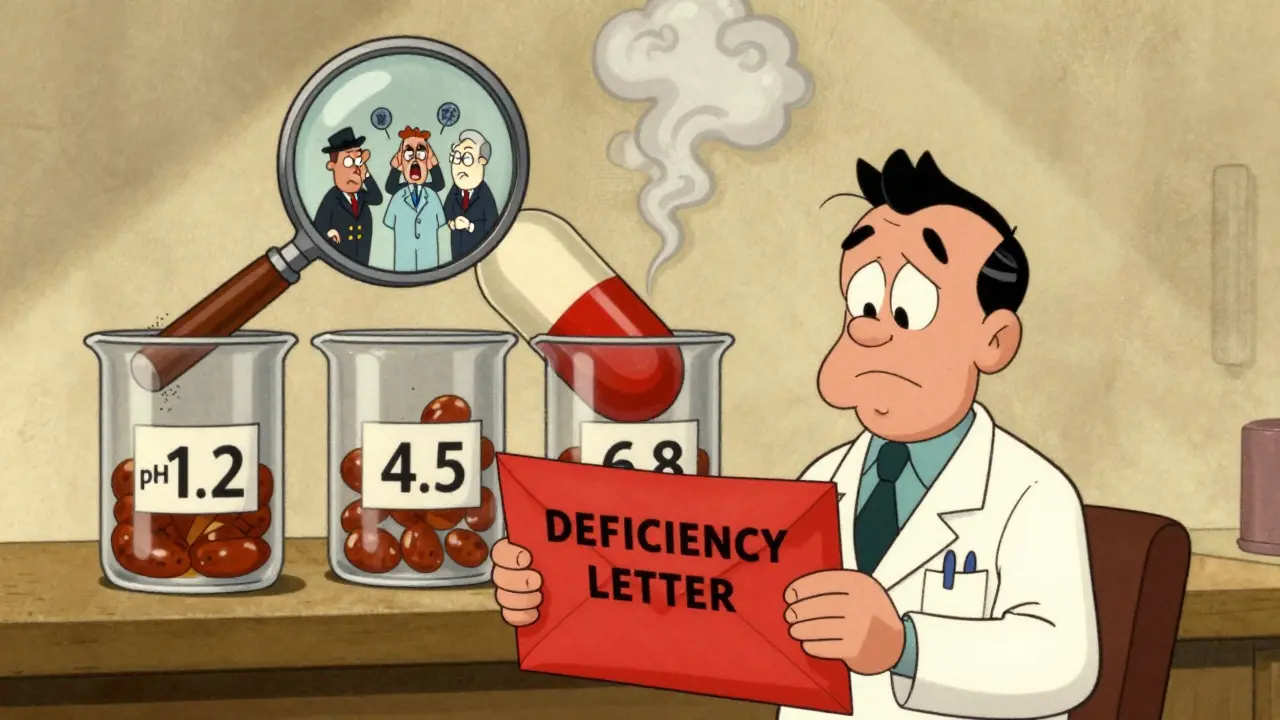
The biggest category? Dissolution issues. In FY2023, 23.3% of all deficiency letters cited problems with dissolution testing. This isn’t just about how fast the pill breaks down. It’s about whether the test method can tell the difference between a good batch and a bad one. Many companies use outdated equipment or test at only one pH level. The FDA expects dissolution methods to reflect real-life conditions-testing across pH 1.2, 4.5, and 6.8, using the right apparatus (usually Apparatus 2 for immediate-release tablets). If your method can’t distinguish between a product that performs well and one that doesn’t, it’s a deficiency.
Next up: analytical method validation. At 16.5%, this is the second most common issue. It sounds technical, but it’s simple: Did you prove your test actually measures what it claims to measure? Many applicants submit data showing their HPLC method detects an impurity-but they never tested for accuracy, precision, or specificity across the full range of concentrations. The FDA needs to see that the method is fit for purpose. No assumptions. No shortcuts.
Drug Substance Problems: The Hidden Trap
One of the most surprising causes of delays? Problems in the Drug Master File (DMF). Over 80% of drug substance deficiencies trace back to issues in the DMF submitted by the raw material supplier. The generic company thinks they’ve done their part-until the FDA reviews the DMF and finds missing data on impurities, particle size distribution, or polymorph control.
For example, if your active ingredient has a known impurity that’s a potential mutagen, you need (Q)SAR data or actual toxicology studies to prove it’s safe. The FDA’s M7 guidance isn’t optional. Yet, 20% of deficiency letters point to unqualified impurities with no safety justification. And if you’re making a peptide drug? You’re not just checking purity. You need circular dichroism, FTIR, and size-exclusion chromatography to prove your molecule’s 3D structure matches the reference drug. Without that, you don’t have sameness.
DS sameness-drug substance sameness-is a major hurdle. Nearly 19% of deficiency letters cite this. It’s not enough to say your API is the same chemical. You have to prove it behaves the same way. Physical properties like crystal form, particle size, and surface area matter. If your supplier changes the manufacturing process without telling you-or you didn’t test for it-you’ll get flagged.
Drug Product Deficiencies: More Than Just a Pill
Now let’s talk about the final product. Modified-release tablets, topical creams, and injectables are where things get complicated. These aren’t simple pills you can copy with a mold. They require precise control over how the drug releases over time.
For modified-release products, 40-65% more applications get deficiency letters than for standard immediate-release tablets. Why? Because multiple systems have to work together: the coating, the matrix, the release mechanism. If your dissolution profile doesn’t match the reference drug across all pH levels and time points, you’ll get a deficiency. And if you didn’t test at the right time intervals-say, only at 1, 4, and 8 hours, but the reference drug releases over 12-you’re not showing bioequivalence.
Elemental impurities are another growing pain. In 13% of submissions, the control strategy for heavy metals like arsenic, cadmium, or lead is incomplete. The ICH Q3D guidelines are clear: you need to assess risk based on your manufacturing process and materials. But many applicants just check a box without showing how they control it. The FDA doesn’t want a list of tests-they want a science-based risk assessment.
Why Do Some Companies Keep Getting the Same Letters?
It’s not always about technical skill. It’s about culture.
Companies with fewer than 10 approved ANDAs have deficiency rates 22% higher than those with 50 or more. Why? Experience. They’ve learned what the FDA looks for. They know that a vague statement like “the method is validated” won’t cut it. They submit full validation reports with acceptance criteria, linearity curves, and robustness testing.
And then there’s the communication gap. A 2023 survey of 127 generic companies found that 78% said unclear FDA feedback led to repeated deficiencies. One company spent 18 months fixing the same dissolution issue because the reviewer’s comments were too vague. They finally got clarity after requesting a pre-ANDA meeting-and the next submission passed on the first try.
Pre-submission meetings aren’t optional for complex products. The FDA’s own data shows companies that use them have 32% fewer deficiencies. These meetings give you a chance to ask: “Is this test acceptable?” or “Does this impurity profile need more data?” Before you spend $2 million on a submission that’s doomed to fail.
What’s Changing at the FDA?
The FDA knows these delays hurt patients. That’s why they launched the First Cycle Generic Drug Approval Initiative in 2023. They’re now providing template responses for the 10 most common deficiencies-exact examples of what a good response looks like. For dissolution, they now show you the right pH levels, apparatus, and number of time points to test. For impurities, they give you the format for a Q3D risk assessment.
They’ve also created specialized review teams for complex products like peptides and modified-release formulations. In 2024, this reduced inconsistent feedback by 22%. No more one reviewer saying “add more data,” and another saying “it’s fine.”
By Q3 2026, the FDA plans to roll out AI-assisted pre-submission screening. It won’t approve your application-but it will flag common errors before you even hit submit. Think of it like a spellchecker for regulatory filings. Early tests show it can catch 35% of preventable mistakes.
How to Avoid a Deficiency Letter
If you’re submitting an ANDA, here’s what actually works:
- Match the reference drug exactly-not just the active ingredient, but the dissolution profile, particle size, and release mechanism. Use the FDA’s Reference Listed Drug Database.
- Validate your methods like your reputation depends on it-because it does. Include specificity, accuracy, precision, linearity, range, and robustness. Don’t skip the control samples.
- Test under real conditions-dissolution at pH 1.2, 4.5, and 6.8. Use Apparatus 2 for immediate-release, Apparatus 3 or 4 for modified-release.
- Don’t rely on your supplier’s DMF-review it yourself. If they haven’t provided full impurity data or polymorph control, ask for it before you submit.
- Request a pre-ANDA meeting-especially if you’re making a complex product. It’s free, and it saves months.
- Document everything-applications with detailed development reports have 27% fewer deficiencies. The FDA doesn’t want to guess. They want to see your thinking.
And if you’re a small company? Don’t try to do this alone. Partner with a regulatory consultant who’s submitted ANDAs before. One mistake in your dissolution method can cost you $1.2 million and over a year of delays.
What Happens After a Deficiency Letter?
When you get one, don’t panic. Don’t rush. Read it line by line. The FDA gives you specific requests: “Provide additional data on impurity X,” or “Justify the use of Apparatus 1.”
Most deficiencies can be fixed in 3-6 months if you respond with clear, complete data. But if you send back vague answers or incomplete studies, you’ll get another letter-and the clock resets. Teva’s regulatory team reported that unqualified impurity deficiencies alone can add 14-18 months to approval timelines because they require new toxicology studies.
The key is to treat the deficiency letter as a roadmap-not a roadblock. The FDA wants your drug to be approved. They just need proof it’s safe, effective, and consistent.
Final Thought: It’s Not About Cheaper-It’s About Reliable
The generic drug market is worth over $110 billion in the U.S. alone. But patients don’t care how much you saved on production. They care that the pill they take today works the same as the one they took yesterday.
The FDA’s job isn’t to slow you down. It’s to make sure that when a patient switches from a brand-name drug to a generic, they don’t get sick because the product isn’t equivalent.
Deficiency letters are frustrating. They’re expensive. But they’re also necessary. The companies that succeed aren’t the ones who submit fastest-they’re the ones who submit right.
What is a deficiency letter from the FDA for generic drugs?
A deficiency letter is a formal notice from the FDA that identifies specific issues in an Abbreviated New Drug Application (ANDA) that prevent approval. It lists missing data, flawed methods, or unproven claims that must be addressed before the application can move forward. It’s not a rejection, but a request for more information to prove therapeutic equivalence.
What are the most common reasons for FDA deficiency letters?
The top reasons are dissolution method and specification issues (23.3% of cases), analytical method validation failures (16.5%), unqualified impurities (20%), drug substance sameness problems (19%), and inadequate control strategies for elemental impurities (13%). Most of these are quality-related and stem from incomplete testing or failure to meet ICH and FDA guidance.
How long does it take to respond to a deficiency letter?
A well-prepared response can take 3 to 6 months. But if the deficiency requires new toxicology studies-like for unqualified mutagenic impurities-it can take 14 to 18 months. The key is responding with complete, high-quality data the first time. Re-submissions with incomplete answers lead to further delays.
Can pre-submission meetings with the FDA help avoid deficiency letters?
Yes. Companies that request pre-ANDA meetings have 32% fewer deficiency letters. These meetings allow applicants to clarify expectations on dissolution methods, impurity controls, or bioequivalence study design before spending millions on a submission. The FDA encourages them, especially for complex products like peptides or modified-release formulations.
Do complex generic drugs have higher deficiency rates?
Yes. Peptides, modified-release tablets, and topical dermatologicals have deficiency rates 40-65% higher than standard immediate-release small-molecule drugs. These products require advanced analytical techniques-like circular dichroism or multi-pH dissolution testing-and stricter control of physical properties. The FDA’s specialized review teams now handle these submissions to improve consistency.
Is there a way to reduce the chance of a deficiency letter?
Absolutely. Focus on three things: 1) Match the reference drug exactly in dissolution and physical properties, 2) Validate every analytical method with full data, and 3) Document your development process thoroughly. Companies that invest in Quality by Design (QbD) and pre-submission meetings see first-cycle approval rates jump from 52% to over 70%.



11 Comments
Wow, this is one of the most clarity-packed threads I’ve read all year. The dissolution stuff? Absolute gold. I’ve seen companies waste millions because they thought ‘close enough’ was good enough. The FDA’s not being petty-they’re protecting people’s lives. 🙌
It is imperative to underscore that the prevailing deficiency patterns are not indicative of regulatory overreach, but rather a reflection of insufficient methodological rigor in analytical validation protocols. The cited 16.5% deficiency rate for analytical method validation is, in fact, a conservative estimate; in my professional experience, non-compliance with ICH Q2(R1) criteria exceeds 40% in submissions from emerging markets.
Bro. I just submitted an ANDA last month and got a deficiency letter for dissolution. I thought I was being smart using Apparatus 1 because it was ‘easier’. 😅 Turns out I was being dumb. FDA’s template for pH 1.2/4.5/6.8? Saved my butt. Just fixed it and resubmitted. Fingers crossed! 🤞
THIS IS WHY WE CAN’T HAVE NICE THINGS. 🚨 The FDA is turning into a bureaucratic nightmare. I mean, come ON-now they want us to test at THREE pH levels?! And don’t get me started on the DMF trap. My supplier sent me a PDF that said ‘impurities controlled’ and I trusted them. Now I’m out $800K and six months. 😭
Thank you for writing this. I’m a pharmacist and I see generics every day. Patients rely on them. It’s scary when they don’t work the same. I’m so glad the FDA’s pushing for real consistency. And pre-meetings? Yes please. We need more of that. ❤️
Is there data on how many deficiency letters get resolved without any changes to the original submission? Like, do companies sometimes just rewrite their answers to sound better without actually fixing the issue?
This is such a good breakdown! 🎉 I work with a small generics startup and we used to think ‘just submit and hope’ was a strategy. Nope. After our first deficiency letter (dissolution, of course), we hired a consultant, did the pre-meeting, and now our approval rate is 100% on first try. The AI screening tool they’re rolling out? I’m already prepping for it. 🤖✨
Man I feel you on the DMF thing. My team got burned last year. Supplier said ‘everything’s fine’ then FDA comes back and says ‘where’s your polymorph data?’ We didn’t even know to ask. Now we have a checklist. Always check the DMF. Always. 🙏
Why does the FDA even exist? This is just control. They don’t want cheaper drugs. They want Big Pharma to keep making profits. You think they care about patients? Nah. They care about power. And now they’re using AI to spy on our submissions. 👁️🗨️
Deficiency letters are just a revenue stream for consultants. Everyone knows this. The FDA’s ‘templates’ are just rebranded boilerplate. Real innovation? They crush it. And ‘QbD’? Just buzzword bingo.
It’s not about being fast. It’s about being right. I’ve seen too many companies rush and end up costing patients more in the long run. The FDA’s process is painful, but it’s the only thing standing between a bad generic and someone’s health. Don’t cut corners. Ever.
Write a comment