OIC Symptom Tracker & Assessment Tool
Opioid-Induced Constipation Assessment
This tool calculates your Bowel Function Index (BFI) score based on your symptoms. A score above 30 indicates significant constipation requiring treatment adjustment.
Why Opioid-Induced Constipation Is More Than Just a Minor Annoyance
If you’re taking opioids for chronic pain, constipation isn’t something you just have to live with-it’s a common, predictable, and often untreated side effect. Around 40 to 60% of people on long-term opioid therapy develop opioid-induced constipation (OIC), and for many, it starts within days of beginning treatment. Unlike other side effects like drowsiness or nausea, which may fade over time, OIC sticks around as long as you’re on opioids. That’s because opioids don’t just block pain signals in the brain-they also slow down your entire digestive system by binding to receptors in your gut.
This isn’t about being "not regular." It’s about your bowels literally shutting down. Opioids reduce muscle contractions in the intestines, increase water absorption from stool, and tighten the anal sphincter, making it harder to pass anything. Patients often describe it as straining for minutes without success, feeling like they haven’t fully emptied their bowels, or having hard, pellet-like stools. Left untreated, OIC can lead to nausea, bloating, loss of appetite, and even dangerous bowel obstructions or fecal impaction.
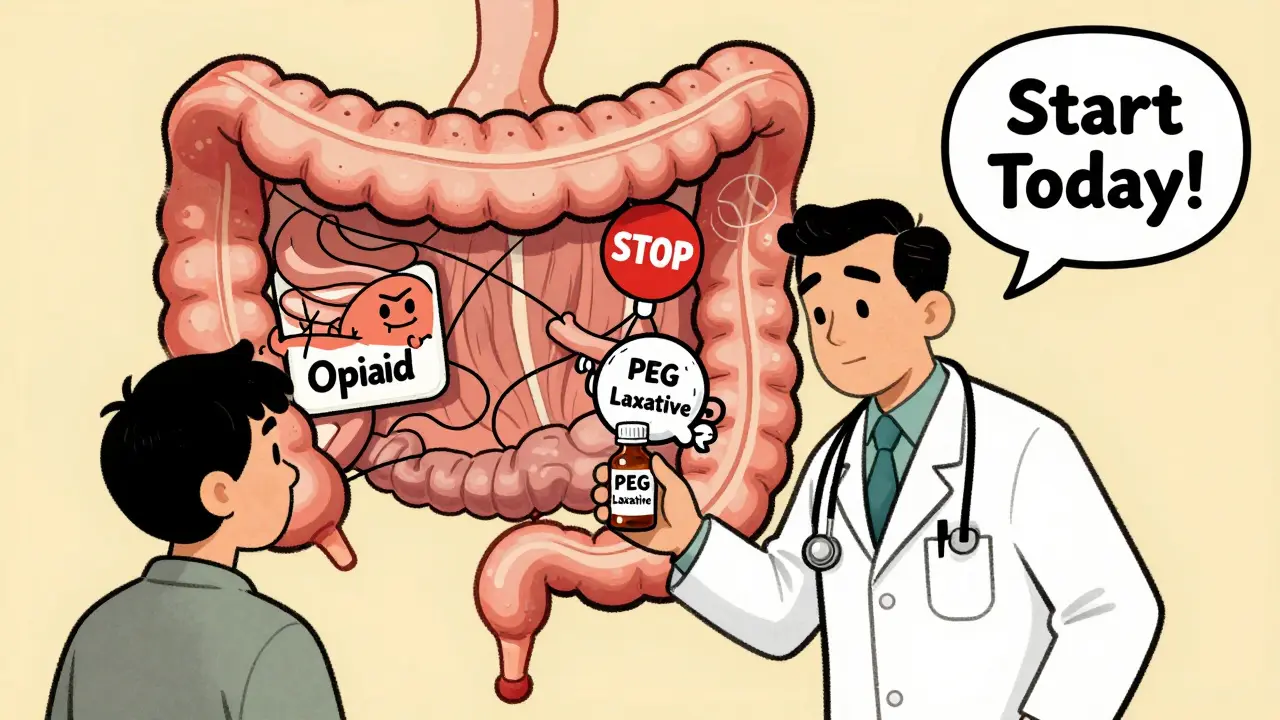
Prevention Starts on Day One
The biggest mistake doctors and patients make? Waiting until constipation shows up before doing anything. By then, it’s already taken root. Experts agree: if you’re starting opioids, you should start a laxative at the same time. This proactive approach can prevent 60 to 70% of severe cases.
It’s not about being overly cautious-it’s about understanding the science. Opioids change how your gut works from the moment you take them. So your bowel routine needs backup from the beginning. The best first-line defense? Osmotic laxatives like polyethylene glycol (PEG), which pull water into the colon to soften stool, and stimulant laxatives like senna or bisacodyl, which gently nudge the muscles to move.
Don’t rely on stool softeners like docusate alone-they’re too weak for OIC. And don’t wait for symptoms to get bad before increasing the dose. Many people take half the recommended amount because they’re afraid of side effects. But with PEG, you can adjust the dose safely. Start with one sachet daily, and if you’re not having a bowel movement every 2 to 3 days, increase it. Your goal isn’t daily poops-it’s consistent, easy passage without straining.
When Laxatives Aren’t Enough: The Role of PAMORAs
For many, even the right laxatives aren’t enough. Studies show 68% of patients on opioids report inadequate relief from standard over-the-counter options. That’s where peripherally acting μ-opioid receptor antagonists (PAMORAs) come in. These are prescription drugs designed specifically to undo the gut-slowing effects of opioids-without touching the pain relief in your brain.
How? PAMORAs like methylnaltrexone (Relistor®), naldemedine (Movantik®), and naloxegol block opioid receptors only in the gut. Because they can’t cross the blood-brain barrier easily, your pain control stays intact. In clinical trials, these drugs have been shown to speed up bowel transit, improve stool consistency, and reduce straining within hours.
There are three main PAMORAs in use:
- Methylnaltrexone (Relistor®): Given as a subcutaneous injection, it works in about 30 minutes. It’s often used in palliative care and for patients who need fast relief. A once-weekly version was approved in 2023, making it easier to manage.
- Naldemedine (Movantik®): Taken as a daily pill, it’s especially recommended for cancer patients by the American Society of Clinical Oncology (ASCO) in 2024. It doesn’t just treat constipation-it may also reduce opioid-induced nausea and vomiting.
- Naloxegol: Another oral option, taken daily, with similar effectiveness to naldemedine.
One Reddit user wrote: "Relistor injections work within 30 minutes when nothing else does." That’s not an outlier-it’s the reality for many who’ve struggled for months.
What About Lubiprostone?
Lubiprostone (Amitiza®) is another option, but it works differently. Instead of blocking opioid receptors, it activates chloride channels in the bowel lining, drawing fluid into the colon to stimulate movement. It’s FDA-approved for women with chronic idiopathic constipation, but studies show it works just as well in men. The catch? Up to 32% of users report nausea, and 11% get diarrhea. It’s not usually a first choice for OIC, but for patients who can’t tolerate PAMORAs or can’t afford them, it’s a viable alternative.
Cost, Access, and the Hidden Barriers
Here’s the hard truth: even the best treatments are useless if you can’t get them. PAMORAs cost between $500 and $900 a month without insurance. Many insurance plans require prior authorization or force patients to try cheaper laxatives first-step therapy-before approving them. A 2024 KFF analysis found that 41% of Medicare Part D plans and 28% of commercial plans impose these hurdles.
And it gets worse: 57% of patients stop using PAMORAs within six months-not because they don’t work, but because of cost or inconsistent results. Some people get great relief. Others notice only slight improvement. There’s no way to predict who will respond best, which makes trial and error frustrating.
Pharmacists are often the unsung heroes here. Studies show that when pharmacists proactively suggest laxatives at the time of opioid prescription, patients are 43% more likely to start them. Ask your pharmacist. Don’t wait for your doctor to bring it up.
When to Be Worried: The Risk of Perforation
PAMORAs are powerful, but they’re not risk-free. The FDA requires all of them to carry a black box warning for gastrointestinal perforation. This is rare-but serious. It’s most likely in people with a history of bowel obstruction, recent abdominal surgery, Crohn’s disease, diverticulitis, or other conditions that weaken the intestinal wall.
If you start a PAMORA and suddenly get sharp, severe abdominal pain, fever, or vomiting, get medical help immediately. These aren’t normal side effects-they’re red flags. Your doctor should screen you for these risks before prescribing. If you’ve had recent surgery or inflammatory bowel disease, PAMORAs may not be safe for you.

Real-Life Management: What Works for Real People
Patients on chronic pain forums and support groups share what actually helps:
- Drinking 2 to 3 liters of water daily-hydration is non-negotiable.
- Adding fiber gradually-too much too fast can worsen bloating.
- Walking at least 20 minutes a day-movement stimulates bowel activity.
- Not ignoring the urge to go-even if you think it won’t work.
- Using a footstool when on the toilet to mimic a squatting position, which naturally aligns the rectum.
One patient on PatientsLikeMe wrote: "Naldemedine has allowed me to stay on my pain medication without constant bathroom struggles." That’s the goal: keeping pain under control without sacrificing quality of life.
How to Track Progress
Don’t guess whether your treatment is working. Use a simple tool called the Bowel Function Index (BFI). It’s a three-question survey that rates your constipation severity:
- How difficult was it to have a bowel movement?
- How complete was your bowel movement?
- How much did constipation interfere with your daily life?
Each question is scored from 0 to 10. Add them up. A score above 30 means you have significant constipation and need to adjust your treatment. Many doctors don’t use it-but you can print it online and bring it to your next appointment.
What’s Next for OIC Treatment?
Research is moving fast. By 2026, doctors may be able to predict your response to OIC treatments based on your genes. Clinical trials are testing combination pills that pair low-dose PAMORAs with traditional laxatives for better results. There’s also growing pressure on insurers to cover these drugs without unnecessary delays. The American Society of Gastroenterology estimates that poor OIC management costs the U.S. healthcare system $2.3 billion a year in avoidable ER visits and hospitalizations.
The message is clear: OIC is not a minor inconvenience. It’s a serious, treatable condition that affects millions. And it doesn’t have to be part of your daily life.
Is opioid-induced constipation permanent?
No, OIC is not permanent, but it lasts as long as you’re taking opioids. Unlike other side effects that fade over time, OIC doesn’t improve on its own. That’s why prevention and ongoing treatment are essential. Once you stop opioids, bowel function usually returns to normal within days to weeks.
Can I just use prune juice or fiber supplements instead of medication?
Prune juice and fiber help with general constipation, but they’re usually not enough for OIC. Opioids directly slow gut movement, which dietary changes alone can’t overcome. Fiber can even make bloating worse if you’re not drinking enough water. For OIC, you need targeted treatments like osmotic laxatives or PAMORAs.
Do PAMORAs reduce pain relief?
No. PAMORAs are designed to work only in the gut and don’t cross the blood-brain barrier in significant amounts. Studies confirm they don’t interfere with opioid pain control. If your pain gets worse after starting a PAMORA, it’s likely due to another issue-not the drug.
How soon should I start a laxative after beginning opioids?
Start the same day. Waiting until you’re constipated means you’re already behind. Research shows that starting laxatives at the same time as opioids prevents most severe cases. Don’t wait for symptoms. Be proactive.
Are there natural remedies that work for OIC?
Hydration, walking, and proper posture on the toilet help-but they’re not enough on their own. Opioids override natural bowel rhythms. Natural remedies can support treatment, but they won’t replace medications proven to work against OIC’s specific mechanism. Don’t rely on them as your only solution.
Can I take PAMORAs if I have kidney or liver problems?
Some PAMORAs need dose adjustments for kidney or liver disease. Naldemedine is metabolized by the liver, so it may need to be lowered if you have liver impairment. Methylnaltrexone is cleared by the kidneys, so dose changes may be needed if your kidney function is reduced. Always tell your doctor about all your medical conditions before starting any new medication.





2 Comments
I've been on long-term opioids for fibromyalgia and started PEG right away. It's been a game changer. No more hours on the toilet, no more bloating. Just regular, easy bowel movements. Don't wait until it's bad. Start day one.
Also, the footstool trick? Real. Makes a surprising difference.
This is the most practical guide I've seen on OIC. So many people think it's just 'not eating enough fiber' and it's not. Opioids wreck your gut function. Laxatives aren't optional.
Write a comment