Medication Side Effect Checker
Check Your Medication Impact
Select your pain medication to see sexual function side effects
Select a medication to see details
Living with chronic pain is a daily battle that reaches far beyond the obvious aches. When the body is constantly sending distress signals, the mind often shifts its focus away from intimacy, leading to low libido and changes in sexual performance. This article breaks down why pain hijacks desire, what biological and emotional pathways are involved, and how you can reclaim a satisfying sex life while still managing the pain.
Why Chronic Pain Shrinks Desire
At its core, chronic pain is a persistent activation of the nervous system. The brain’s pain‑processing centers-especially the thalamus and anterior cingulate cortex-stay on high alert, diverting resources that would otherwise support pleasure and arousal. When the body is in a constant state of "fight or flight," the hormone cascade favors cortisol and adrenaline over sex hormones like testosterone and estrogen, dampening sexual drive.
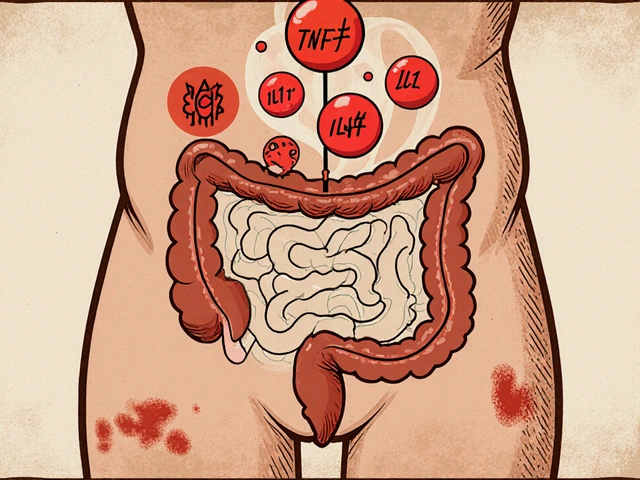
Biological Pathways Linking Pain and Libido
Three main physiological routes explain the connection:
- Neurotransmitter imbalance: Pain increases the release of substanceP and glutamate, which can suppress dopamine - the brain’s reward messenger essential for sexual excitement.
- Hormonal shifts: Elevated cortisol lowers testosterone and estradiol levels, directly reducing libido. In men, a drop of even 10nmol/L can mean a noticeable loss of drive.
- Reduced blood flow: Chronic inflammation constricts peripheral vessels, making erectile response or vaginal lubrication slower and less reliable.
These changes don’t happen overnight. Studies from the University of Oxford (2023) showed that patients with fibromyalgia experienced a 30% average decline in testosterone after six months of uncontrolled pain.
Psychological Factors That Compound the Issue
When pain dominates daily life, mood suffers. Depression a common co‑occurring condition marked by persistent sadness and loss of interest often follows, and it carries its own libido‑killing effect. Anxiety about pain flare‑ups can trigger performance anxiety, creating a feedback loop where fear of pain during sex leads to avoidance, which then fuels relationship tension.
Medications: Double‑Edged Swords
Many pain‑relief drugs have side‑effects that hit sexual function hard. Below is a quick comparison of the three most prescribed classes.
| Medication Class | Typical Use | Common Sexual Side‑Effect | Mechanism |
|---|---|---|---|
| Opioids | Severe acute or chronic pain | Reduced libido, erectile dysfunction | Suppresses hypothalamic‑pituitary‑gonadal axis |
| Antidepressants (SSRIs) | Co‑existing depression or neuropathic pain | Delayed orgasm, decreased arousal | Increases serotonin, which inhibits dopamine pathways |
| NSAIDs (e.g., ibuprofen) | Mild‑to‑moderate inflammatory pain | Generally minimal; occasional fatigue | Reduces prostaglandins without hormonal interference |
Because opioids are notorious for lowering testosterone, many clinicians recommend physiotherapy a hands‑on treatment that improves movement and reduces pain through targeted exercises or non‑opioid alternatives when possible.
Non‑Pharmacological Strategies to Boost Sexual Health
Addressing the root pain while nurturing intimacy can revive desire. Here are evidence‑backed approaches:
- Mind‑Body Therapy: Cognitive‑behavioral therapy (CBT) a structured talk therapy that reshapes thoughts about pain and sexuality reduces catastrophizing and improves sexual confidence.
- Pelvic Floor Rehabilitation: For both men and women, gently strengthening pelvic muscles can improve arousal response and alleviate discomfort during intercourse.
- Exercise: Low‑impact activities like swimming or yoga lower cortisol, increase endorphins, and can raise testosterone by up to 15% in sedentary males after 12 weeks.
- Sleep Hygiene: Chronic pain often disrupts sleep, and poor rest further depresses sex hormones. Aim for 7‑9hours of uninterrupted sleep; consider nighttime stretches or a warm bath to ease pain before bed.
- Nutrition: Anti‑inflammatory foods (omega‑3 rich fish, berries, leafy greens) can reduce systemic inflammation, indirectly supporting vascular health needed for arousal.
Talking About Pain and Sex With Your Partner
Open communication prevents misunderstandings. Start the conversation during a relaxed moment, not in the middle of a painful flare‑up. Use "I" statements-"I feel less desire when my back hurts"-instead of blaming language. Exploring new forms of intimacy (massage, cuddling, sensual reading) can keep the emotional connection alive while the body heals.

When to Seek Professional Help
If low libido persists for more than three months despite pain management, or if sexual activity causes additional pain, it’s time to involve a specialist. A multi‑disciplinary team-GP, pain specialist, and sex therapist-can tailor a plan that addresses both the physical and emotional dimensions.
Key red‑flags include:
- Sudden loss of interest in any sexual activity
- Pain that intensifies during intercourse
- Significant mood swings, anxiety, or depressive episodes
- Hormone‑related symptoms (e.g., hot flashes, decreased muscle mass)
Early intervention can prevent the cycle of pain → low libido → relationship strain → worsening pain.
Putting It All Together: A Practical Action Plan
- Track pain levels and sexual desire in a simple journal for two weeks.
- Discuss findings with your GP; ask about hormone tests if testosterone feels low.
- Consider tapering opioids under medical supervision and adding physiotherapy.
- Schedule a CBT session focused on pain‑related anxiety.
- Introduce one new intimacy activity each month to rebuild connection.
Following these steps creates a feedback loop where reduced pain improves mood, which in turn boosts libido, making both pain and sexual function easier to manage.
Frequently Asked Questions
Can chronic back pain make it impossible to have an erection?
Back pain can interfere with nerve signals and blood flow, which are essential for an erection. However, most men can improve erectile function by managing the pain, staying active, and, if needed, discussing medication options with a urologist.
Do NSAIDs affect my sex drive?
NSAIDs have the least impact on hormones compared with opioids or antidepressants. Some people report mild fatigue, but they rarely cause a noticeable drop in libido.
Is it safe to use a vacuum erection device while I have chronic pelvic pain?
Generally yes, but consult your pain specialist first. The device creates a suction that could aggravate sensitive pelvic tissues if the pain is severe.
How long does it take for hormone levels to recover after reducing opioid use?
Most patients see measurable testosterone rises within 4‑6weeks of tapering, but full recovery can take up to six months depending on age and duration of opioid therapy.
Can mindfulness meditation help with pain‑related low libido?
Yes. Mindfulness reduces cortisol, improves body awareness, and often restores a sense of pleasure. A daily 10‑minute practice has been linked to a 12% increase in sexual desire in chronic pain cohorts.





18 Comments
Totally get how painful this stuff can be its easy to lose drive when every day feels like a battle keep pushing you got this
Reading through this was like flipping through the most vivid kaleidoscope of science and soul it paints a picture so bright you can almost feel the hormone waves crashing like surf on a restless shore the brain is basically a factory of fire and ice when chronic pain takes the helm it shuts down the pleasure department and the engine of desire gets rusted over by cortisol and adrenaline like an old rusted bike left out in the rain the neurotransmitter imbalance is a sneaky thief it kidnaps dopamine the very spark of excitement and then swaps it for a dull thrum of substance P and glutamate the hormonal shifts turn testosterone into a whisper and estrogen into a sigh the body’s own orchestra loses its rhythm the blood vessels that normally dance in sync with arousal become sluggish warped by inflammation and tension your mind, body and spirit all get caught in this endless feedback loop of distress and doubt but there is hope there is a roadmap out of this dark tunnel the article lays out practical steps like mind‑body therapy that can rewire those pathways like a master carpenter reworking a sagging beam the pelvic floor exercises act like tiny engineers rebuilding the foundation of intimacy the gentle rhythm of yoga and swimming can lift cortisol levels like a balloon shedding weight it’s fascinating how a simple diet change with omega‑3 rich foods can calm the fire inside and let the blood flow like a river again the key takeaway is that you are not doomed you can reclaim desire by tackling pain at its roots by listening to your body and your partner and by staying curious about the tools that science offers keep the flame alive and let the pain be a teacher not a tyrant
Great rundown of the mechanisms I especially appreciate the bullet points on neurotransmitters and hormones. It’s useful to see the connection between cortisol spikes and testosterone drops. The table of medication side effects was spot on and easy to read. I think adding a quick tip about checking hormone panels could help folks track progress. Overall solid info that balances science with practical advice.
This article reads like a watered‑down propaganda piece from the wellness elite. It pretends to be neutral while pushing a neoliberal agenda of self‑optimisation through yoga and “mind‑body” buzzwords. The focus on personal responsibility ignores systemic issues like access to proper pain management and the pharmaceutical industry's grip. If you’re looking for real change, start demanding better healthcare policies instead of just doing pelvic floor exercises. The vibe is overly saccharine and dismissive of genuine suffering.
Honestly, I think the whole “medication side‑effect checker” is a cover‑up. Big pharma knows they’re suppressing libido to keep us dependent on their drugs. They sprinkle in “exercise” and “mindfulness” to make us think we’re in control while the real power players pull strings behind the scenes. Don’t be fooled by the pretty charts. Look deeper and you’ll see the hidden agenda.
Well this is another lazy attempt to pat the reader on the back and call it a solution. The article throws around buzzwords like “non‑pharmacological strategies” without giving any real data beyond vague percentages. The claim that yoga can raise testosterone by 15% is tossed in like a miracle cure, yet the source is nowhere to be found. It feels like a marketing copy for a wellness startup rather than a serious medical guide. The emphasis on “talk therapy” as if it can magically fix hormonal imbalances is absurd. We need rigorous studies, not anecdotal hype.
I love how the piece breaks everything down into clear steps it makes the whole thing feel doable even when you’re dealing with constant pain it’s cool to see the reminder that tracking pain and desire can actually help you spot patterns and talk to your doctor about hormone tests it’s a solid roadmap for anyone feeling stuck
Quick tip: if you’re on opioids ask your doctor about a testosterone panel. It’s a simple blood test and can give you clear direction on whether hormone therapy might help.
Stay hopeful! Even small changes in sleep or a short walk can make a big difference in mood and desire. You’ve got this.
OMG the drama of chronic pain stealing your sex life is like a soap opera you deserve a happy ending and these tips are the plot twist we needed!
This analysis is riddled with half‑baked claims. The “up to 15% testosterone increase” from exercise is a statistical fluke not a reliable treatment. The article glosses over the fact that many patients can’t even commit to a regular workout routine due to pain. It’s a classic case of blaming the patient for systemic failures.
While I see where you’re coming from, it’s important to recognize that not everyone can jump into a rigorous exercise program. Small, consistent movements can still yield hormonal benefits without aggravating pain. Encouraging flexibility in the approach helps more people feel empowered rather than discouraged.
It is utterly unacceptable to dismiss the profound socioeconomic barriers that prevent many from accessing such “flexible” regimens. The discourse must shift from individual blame to structural reform if we are to see genuine improvement.
Good point about the need for tailored plans. Even a short 5‑minute stretch in the morning can be a game‑changer for some folks dealing with limited mobility.
I feel for anyone wrestling with this. The balance between pain management and intimacy is delicate, and taking it step by step, with compassion for yourself, can truly lighten the burden.
One has to wonder if the pharmaceutical companies are secretly happy about this “balance” narrative. It keeps us in a perpetual loop of dependency while they profit from the very side‑effects they claim to mitigate.
Remember, even tiny wins are victories. Celebrate each night you feel a bit more connected to your partner-those moments add up.
Take it one day at a time.
Write a comment