For decades, Medicare couldn’t negotiate drug prices. Private insurers could, but Medicare-covering over 65 million Americans-was legally blocked from doing the same. That changed in 2022 with the Inflation Reduction Act. Now, for the first time, the federal government is directly negotiating lower prices for the most expensive single-source drugs. And starting January 1, 2026, those discounts will hit your pharmacy counter.
What’s Actually Being Negotiated?
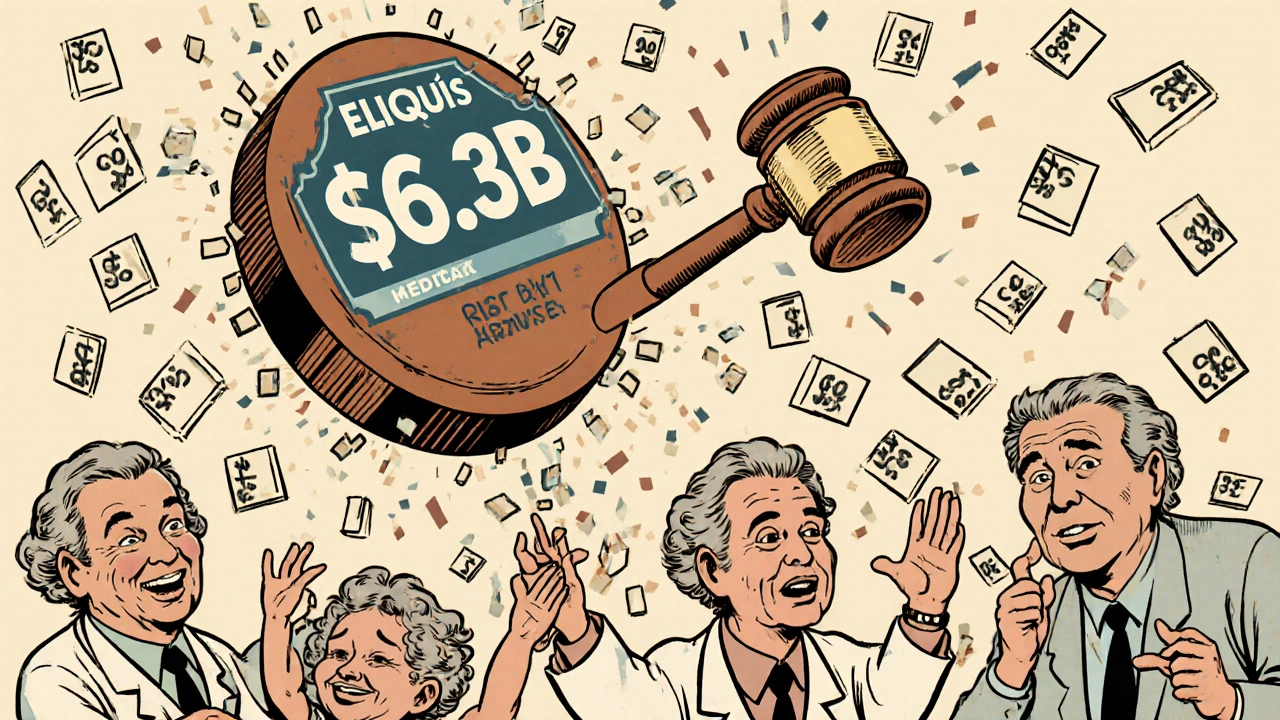
The program doesn’t touch every drug. It only targets high-cost, single-source medications with no generic or biosimilar competition. To qualify, a drug must be at least 7 years old for small-molecule pills (like blood thinners) or 11 years for biologics (like injectables for arthritis or diabetes). That means brand-new miracle drugs are off-limits-for now. The first 10 drugs selected for negotiation include big-name medications like Eliquis (for blood clots), Jardiance (for diabetes), and Xarelto (for stroke prevention). These drugs cost Medicare over $50 billion in 2022 alone. Eliquis, for example, accounted for $6.3 billion in spending that year. Medicare’s goal isn’t to slash prices to zero. It’s to set a “Maximum Fair Price” (MFP)-a price that reflects what the drug is actually worth based on its clinical value, how often it’s used, and what alternatives exist. The final price is the result of back-and-forth talks between the Centers for Medicare & Medicaid Services (CMS) and the drugmakers.How the Negotiation Process Actually Works
It’s not a casual chat over coffee. It’s a tightly timed, rule-bound process with clear deadlines. On February 1, 2024, CMS sent its first offer to each of the 10 drugmakers. That offer wasn’t random. It was built using real data: how many people use the drug, what other treatments are available, and how much Medicare has paid for it in the past. Each offer included a short explanation of how CMS arrived at that number. Drugmakers had exactly 30 days to respond with a counteroffer. Then, CMS scheduled up to three in-person or virtual meetings with each company between March and July 2024. During these meetings, both sides tweaked their numbers. CMS could raise its offer if new data came in. Manufacturers could lower their counteroffers if they saw the writing on the wall. Five of the 10 drugs reached agreement during these meetings. The other five were settled through final written offers. By August 1, 2024, the process was done. The results? Discounts between 38% and 79% off what those drugs cost before.Why This Matters for You
If you’re on Medicare Part D (the prescription drug plan), those discounts will show up in your out-of-pocket costs starting January 1, 2026. You won’t see a price drop on the shelf-drugmakers still set the list price. But Medicare’s negotiated price becomes the baseline that your plan uses to calculate your share. That means:- If you’re in the coverage gap (the “donut hole”), you’ll pay less. Your cost-sharing is tied to the negotiated price, not the inflated list price.
- If you’re in the catastrophic phase, your savings might be smaller, because you’re already paying a fixed percentage of the cost. But your plan’s overall costs will drop, which could lead to lower premiums over time.
- If you’re not on Medicare, you might still benefit. Private insurers often use Medicare’s negotiated price as a benchmark. Some have already started adjusting their own rates in anticipation.
What About Doctors and Hospitals?
This isn’t just about pills you pick up at the pharmacy. Some of these drugs-like those given in a clinic or hospital-are covered under Medicare Part B. Starting in 2028, Medicare will begin negotiating prices for those, too. But here’s the twist: Doctors and hospitals get paid based on the drug’s price. Right now, they’re reimbursed at Average Sales Price (ASP) plus 6%. Under the new system, they’ll get the Maximum Fair Price plus 6%. That might sound fair, but it could mean less money for practices that rely on those drugs to stay profitable. The American Medical Association estimates that for the first 15 Part B drugs negotiated, physician practices could lose $1.2 billion in annual revenue. That’s why some clinics are already rethinking which drugs they stock and how they bill.Will This Lower Drug Prices Everywhere?
Yes-and no. The program is designed to impact only Medicare. But the market doesn’t work in silos. When Medicare sets a new price floor, private insurers notice. The Pharmaceutical Care Management Association estimates that private plans could save $200-250 billion over the next decade just from “spillover effects.” Why? Because drugmakers often don’t want to charge private insurers more than what Medicare pays. If they did, those insurers might drop the drug from their formularies entirely. It’s like a ripple effect. Once Medicare locks in a lower price, it becomes harder for companies to justify charging more elsewhere.What’s Next?
The first 10 drugs are just the beginning. In 2027, CMS will negotiate prices for 15 more. In 2028, another 15. Then 20 every year after that. The list includes drugs like Farxiga, Stelara, and Ozempic-medications millions of Americans use daily. The program is also expanding to Part B drugs, which means more injections, infusions, and treatments will be up for negotiation. And if Congress changes the eligibility rules-say, lowering the 7-year waiting period-the number of negotiable drugs could jump by nearly half.
What’s the Pushback?
Drugmakers aren’t happy. Four of the 10 companies sued, claiming the law is unconstitutional. A federal judge dismissed those lawsuits in August 2024, but appeals are expected. PhRMA, the industry group, argues the program will hurt innovation, claiming $112 billion in lost R&D funding over 10 years. But the Office of Management and Budget says those numbers are wildly inflated. Real-world data from the VA-which has negotiated prices for decades-shows drugmakers still make profits even with lower prices. Meanwhile, patient groups like the Arthritis Foundation worry about access. If a drug gets replaced by a cheaper alternative, will you still be able to get the one that works best for you? That’s a real concern for people with complex conditions.What Should You Do Now?
Nothing. Not yet. But pay attention. If you’re on Medicare, review your Part D plan’s formulary in late 2025. You’ll see changes. Some drugs may move to lower tiers. Others might be replaced by generics or biosimilars. If you’re not on Medicare but take one of these drugs, ask your pharmacy if your insurer is adjusting prices. Some already are. And if you’re a caregiver or family member helping someone manage prescriptions, start tracking which drugs they take. If it’s on the 2026 list, you’ll see a noticeable drop in costs next year.Bottom Line
This isn’t a magic fix. It won’t eliminate all high drug prices. But it’s the first time the U.S. government has directly challenged the status quo-and it’s working. The first round of negotiations delivered discounts of up to 79%. That’s not a small win. That’s a seismic shift. The system is still being tested. Legal battles will continue. Drugmakers will adapt. But for millions of Americans paying hundreds or thousands a year for one prescription, this is the first real chance to see those costs go down-and stay down.Will Medicare drug negotiations lower my out-of-pocket costs right away?
No, not yet. The first negotiated prices take effect on January 1, 2026. If you’re on Medicare Part D, you’ll start seeing lower costs at the pharmacy counter starting then. Before that, your plan will still use the old list prices. Keep an eye on your plan’s annual notice in October 2025-it’ll show you exactly which drugs are affected.
Are all prescription drugs eligible for negotiation?
No. Only single-source drugs without generics or biosimilars that are at least 7 years old (for pills) or 11 years old (for injectables) qualify. Newer drugs, like the latest GLP-1 weight-loss medications, won’t be eligible until they hit those age thresholds. Also, drugs with multiple manufacturers or generic versions aren’t included.
Can I choose a different drug if mine gets negotiated?
You can always ask your doctor about alternatives, but the negotiated drug won’t disappear. It’ll just cost less. Your plan might still cover it at a lower tier, meaning you pay less. If your doctor recommends it and it’s still on your plan’s formulary, you can keep using it. The goal isn’t to remove drugs-it’s to make them more affordable.
Will this affect my private insurance?
Not directly, but likely indirectly. Many private insurers use Medicare’s negotiated price as a benchmark. If Medicare pays less, insurers may adjust their own rates to match. Some already have. You might see lower copays or fewer restrictions on certain drugs over time-even if you’re not on Medicare.
What if my drug is on the 2027 list but I’m not on Medicare yet?
You still might benefit. Drugmakers often apply the same lower price to all markets to avoid complexity. If Medicare negotiates a price for a drug in 2027, your private insurer may adopt that same price for their members. It’s not guaranteed, but it’s becoming more common.





15 Comments
Finally, something that actually helps people instead of lining pharma executives’ pockets. I’ve been watching my mom struggle to afford her diabetes meds for years. If this cuts her costs by half, it’s a win. No hype, no spin-just real relief.
While the structural integrity of this policy is commendable, one must not overlook the systemic disincentives it introduces into the innovation ecosystem. The marginal cost of R&D capital allocation is being artificially suppressed, which may lead to a suboptimal equilibrium in pharmaceutical advancement over the next decade.
Oh wow, the government’s now playing drug dealer? Next they’ll be negotiating the price of oxygen. Maybe they’ll start telling us how to breathe too. Free market? More like free-for-all socialism with a side of insulin.
In India, we’ve seen how price controls can backfire-fewer drugs reach rural clinics. But this feels different. It’s targeted, transparent, and tied to real usage data. Maybe the U.S. is finally learning that healthcare isn’t a casino.
I remember when my sister had to choose between her arthritis drug and paying her rent. She took the drug. She lost her apartment. This isn’t about politics-it’s about dignity. People aren’t numbers in a spreadsheet. They’re mothers, fathers, grandparents trying to stay alive. If this saves even one person from that choice, it’s worth every second of the fight.
And yes, I know the drug companies say it’ll hurt innovation. But they’ve been making record profits for decades while people ration pills. Maybe innovation doesn’t mean making a drug cost $10,000 a year. Maybe it means making sure the people who need it can actually get it.
I don’t care if it’s ‘socialist’ or ‘un-American.’ What’s un-American is letting someone die because they can’t afford a pill that costs $5 to make.
so like… if the drug is like 7 years old, then they can negotiate? so like, what if the company just releases a new version with like, a different color? does that reset the clock? because that’s what they always do lol
The negotiation process is flawed. The 30-day window is arbitrary. The data used by CMS lacks longitudinal validation. This is regulatory theater masquerading as policy.
They’re using this to track us. Once they control drug prices, they control our health data. Next thing you know, they’ll be forcing us to take ‘approved’ meds and deleting our medical records if we don’t comply. 🕵️♂️
Been working in a clinic for 12 years and I’ve seen patients skip doses because they can’t afford the copay. This is huge. The 7-year rule is smart-lets companies recoup costs before the government steps in. And the spillover effect? That’s the real win. Private insurers will have to follow. It’s not perfect but it’s a start
Wow. Another government overreach wrapped in feel-good language. The real issue? Doctors got paid too much. Let’s just cut their salaries instead of pretending we’re helping patients. This is performative policy for the middle class.
This is the end of freedom. You think the government’s gonna stop at drugs? Next they’ll tell you what kind of milk to drink, what car to buy, what color socks to wear. They’re just getting started. This is the slippery slope to full control. I’ve seen it happen in other countries. Now it’s here. And people are cheering?
My cousin in Canada can’t get his cancer drug for 18 months. That’s what happens when the government runs healthcare. We’re turning into Canada. And we’re proud of it?
They say it’s only 10 drugs. But what about the 15 next year? And the 20 after that? Where does it end? When they’re negotiating the price of your insulin and your blood pressure pill and your heart med and your antidepressant? When your doctor says ‘I’m sorry, but the government won’t pay for that one anymore’?
This isn’t about lowering costs. It’s about control. And they’re using our pain to get it.
Let’s be real-this is just a distraction. The real problem is that the FDA approves drugs too fast and the courts let pharma get away with patent evergreening. This is theater. They’re pretending to fix the system while the real rot continues. You want to lower prices? Break the patents. Not negotiate like it’s a used car lot.
While the Inflation Reduction Act’s pharmaceutical provisions represent a significant departure from prior policy paradigms, one must acknowledge the nuanced implications for market dynamics. The introduction of a state-mediated pricing mechanism, albeit limited in scope, introduces a structural reconfiguration of value-based reimbursement that may, over time, recalibrate global pricing norms.
Drug companies are making billions. Doctors are getting paid more than teachers. And you’re mad because the government is finally asking them to stop gouging? You’re not poor-you’re just mad your rich uncle’s stock portfolio took a hit. Get over it.
One might reasonably question whether the imposition of a Maximum Fair Price constitutes a regulatory taking under the Fifth Amendment. The absence of a clear, market-based valuation methodology renders the entire framework susceptible to arbitrary application. The moral appeal of the policy cannot, in law, substitute for constitutional rigor.
Write a comment