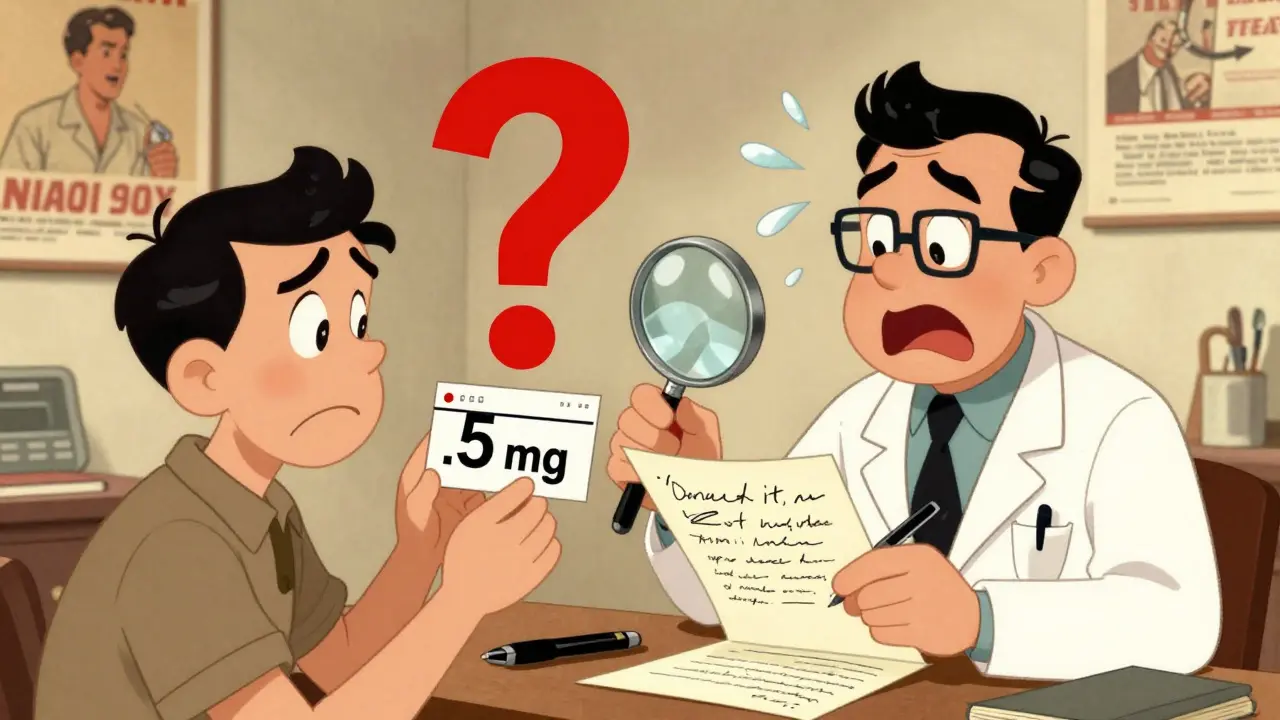
You’ve just picked up your prescription. The label says 5 mg of your new medication, taken once daily. But you remember your doctor said 0.5 mg. Did they mean 5 or 0.5? What if you took the wrong dose? You’re not alone. Thousands of people face this exact confusion every day-not because they misunderstood, but because the prescription itself was written poorly.
Prescription writing errors are one of the most common and dangerous types of medical mistakes. They don’t happen in the pharmacy. They start at the doctor’s desk. And if you don’t catch them, you could end up taking too much, too little, or the wrong drug entirely. The good news? You don’t have to wait for someone else to fix it. You can spot these errors yourself-and you should.
What Exactly Counts as a Prescription Error?
A prescription error isn’t just a typo. It’s any mistake made when a doctor writes or sends a medication order. These can be deadly. The FDA has documented cases where patients died after taking 10 times the intended dose because a doctor wrote ‘.5 mg’ without the leading zero-and the pharmacy read it as ‘5 mg’. That’s not a small mistake. That’s life or death.
According to research from the National Coordinating Council for Medication Error Reporting and Prevention, these errors happen in about 1 in 5 prescriptions. Some of the most common types include:
- Wrong dosage (like 50 mg instead of 5 mg)
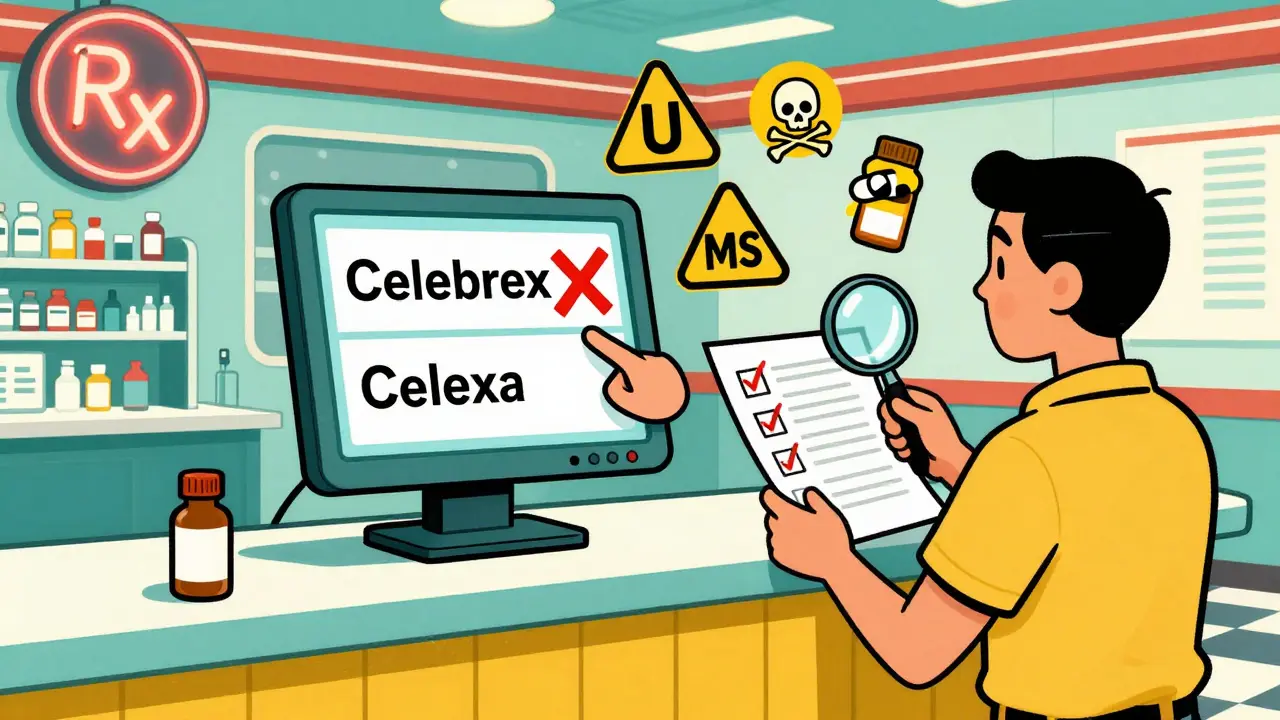
- Incorrect drug name (Celebrex instead of Celexa)
- Confusing abbreviations (‘U’ for units, ‘QD’ for daily)
- Missing or unclear instructions (‘take as needed’ without context)
- Drug interactions (prescribing blood thinners with NSAIDs without checking)
- Forgetting to list the reason for the drug (e.g., no indication for the painkiller)
Even small things matter. Writing ‘MS’ for morphine sulfate? That could be confused with magnesium sulfate-a totally different drug that can stop your heart if given the wrong way. Or using ‘Ug’ for micrograms? That’s often read as ‘units’, leading to fatal insulin overdoses.
Why Do These Errors Happen?
You might think, ‘My doctor is trained. They wouldn’t make this mistake.’ But the truth is, they’re under pressure. A 2021 JAMA study found doctors in busy clinics spend an average of just 17 seconds writing each prescription. That’s less time than it takes to brew a cup of coffee.
Handwriting used to be the biggest problem. Now, with electronic prescriptions, the issue has shifted. Instead of messy scrawl, you get dropdown menus with 50 similar-sounding drugs. Pick the wrong one by accident? You’ve just prescribed the wrong medication. A 2019 JAMA Internal Medicine study found that 34% of new prescription errors came from electronic systems-not because they were broken, but because they were too easy to misuse.
High-alert medications are especially risky. Insulin, blood thinners, opioids, and seizure drugs cause 72% of fatal prescription errors, even though they make up only 8% of all prescriptions. These drugs don’t have room for error. And yet, doctors still write them without clear dosing instructions, patient-specific warnings, or purpose statements.
And here’s the kicker: only 58% of prescriptions follow basic safety rules like using metric units, avoiding abbreviations, and stating why the drug is being given. That means more than 4 in 10 prescriptions are missing critical safety info.
What to Look for When You Get Your Prescription
You don’t need to be a doctor to catch these mistakes. You just need to know what to look for. Before you leave the pharmacy, check your prescription label against these seven key points:
- Full drug name-No abbreviations. It should say ‘Lamotrigine’, not ‘Lamictal’ (which is the brand name and can cause confusion). Brand names aren’t always safe to use on prescriptions.
- Precise dosage-Always written with a leading zero for numbers under 1. So it’s ‘0.5 mg’, never ‘.5 mg’. And never a trailing zero: ‘5.0 mg’ should be ‘5 mg’. Trailing zeros can be mistaken for extra zeros, turning 5 mg into 50 mg.
- Clear frequency-Avoid ‘QD’, ‘BID’, or ‘TID’. Those are medical shorthand. It should say ‘once daily’, ‘twice daily’, or ‘three times daily’.
- Total quantity-Does the number of pills match what you expect? If you’re on a 30-day course, you should get 30 pills. If you get 90, ask why.
- Purpose of the drug-It should say why you’re taking it: ‘for high blood pressure’, ‘for anxiety’, ‘for nerve pain’. If it’s blank, ask.
- Prescriber’s contact info-If the pharmacy calls with a question, they need to be able to reach the doctor. No phone number? That’s a red flag.
- Expiration date-Medications can degrade. If the expiration is more than a year away, it’s fine. But if it’s already expired, don’t take it.
Use this checklist every time. A 2022 University of Michigan study showed patients who used this exact list caught 63% of errors before leaving the pharmacy. Without it, only 22% caught anything.
Red Flags You Should Never Ignore
Some errors are easy to spot if you know what to watch for. Here are the most dangerous ones:
- ‘U’ for units-Always spelled out as ‘units’. ‘U’ looks like a ‘0’ or a ‘4’ in bad handwriting or on blurry screens.
- ‘MS’ or ‘MSO4’-This could mean morphine sulfate or magnesium sulfate. The difference? One calms pain. The other can stop your heart.
- ‘HC’ for hydrocortisone-Mistaken for heparin (a blood thinner). One treats skin rashes. The other prevents clots.
- Look-alike/sound-alike drugs-Celebrex (for arthritis) vs. Celexa (for depression). Zyprexa (for schizophrenia) vs. Zyrtec (for allergies). These pairs cause confusion even in electronic systems.
- High-alert meds without context-If you’re given insulin, warfarin, or fentanyl and no one explains why, ask. Don’t assume.
Keep the ISMP’s list of error-prone drug pairs handy. You can find it online. Bookmark it. Print it. Keep it in your wallet. You don’t need to memorize all of them-just know that if two drugs sound alike, they might be dangerous to mix up.
How to Verify Your Prescription Out Loud
Don’t just nod and walk away. Say something. Use the teach-back method. It’s simple: when the pharmacist explains how to take your medicine, repeat it back in your own words.
Example: Pharmacist says, ‘Take one tablet by mouth twice a day with food.’ You say, ‘So I take one pill in the morning and one in the evening, right after eating?’
Johns Hopkins Medicine found this method reduces misunderstandings by 81%. It forces the pharmacist to clarify if you got it wrong-and if they don’t correct you, you’ve just caught a mistake.
For electronic prescriptions, check the pharmacy’s printed label against your condition. If you have diabetes and they gave you insulin, that’s correct. If they gave you a blood pressure pill instead, that’s wrong. Don’t assume the system got it right.
Use the ‘Ask Me 3’ Questions
The National Patient Safety Foundation created a simple tool called ‘Ask Me 3’. It’s three questions every patient should ask:
- What is my main problem?-This makes sure you understand the diagnosis.
- What do I need to do?-This confirms the treatment plan, including medication.
- Why is it important for me to do this?-This helps you understand the risk of skipping or misusing the drug.
A 2021 JAMA Network Open study showed patients who asked these three questions had 44% fewer medication errors. It’s not about being difficult. It’s about being safe.
What About Electronic Prescriptions?
Yes, e-prescribing cut handwriting errors by 55%. But now you have new risks: dropdown menus with similar names, default doses that don’t match your needs, and safety alerts you can just click past.
Here’s what you can do:
- Ask your doctor if they use a system with patient verification. Some now require you to confirm the medication before it’s sent.
- Use apps like MedSafety. They let you take a photo of your prescription and scan it for errors. In a 2023 pilot study, they reduced patient-identified errors by 68%.
- Check your patient portal. By 2025, all electronic health records in the U.S. will let you see your prescriptions in real time. Log in. Verify. Report anything that looks off.
If your doctor doesn’t use a system that shows you the prescription before it’s sent, ask them to. You have the right to see it.
What If You Catch an Error?
Don’t panic. Don’t argue. Just say: ‘I think there might be a mistake here. Can we double-check?’
Pharmacists are trained to catch these. They’re the last line of defense. If they don’t respond, call your doctor’s office. If you’re still not sure, go to a different pharmacy. Don’t take the medication until you’re certain.
And if you’re helping an elderly parent or someone with low health literacy? Sit with them. Go over the checklist together. Read the label out loud. Many errors happen because people are too afraid to ask questions.
What’s Changing in the Future?
Things are getting better. By 2027, patient-mediated error detection could reduce prescribing errors by 60%. New systems will send you an automated text with your prescription details the moment it’s written. You’ll be able to reply with ‘correct’ or ‘wrong’ before the pharmacy fills it.
Some hospitals are even testing blockchain-based tracking-so you can see exactly what was prescribed, what was dispensed, and who changed it. And by 2030, most prescriptions will require your digital signature before they’re processed.
But none of that matters if you don’t look. The biggest barrier isn’t technology. It’s silence. Too many people assume someone else is checking. But no one else is looking out for you like you are.
Final Thought: Your Prescription Isn’t Final Until You Say So
You’re not just a patient. You’re a partner in your care. And your life depends on you speaking up. A single question-‘Is this right?’-could save you from a hospital stay, a bad reaction, or worse.
Next time you get a prescription, don’t just take it. Check it. Ask about it. Repeat it back. Use the checklist. Use the ‘Ask Me 3’. Use the app. Don’t wait for someone else to fix it. You’re the only one who knows how you feel, what you’ve been told, and what feels off.
Be the one who catches the error. Because if you don’t, no one else will.