When your doctor writes a prescription for a brand-name medication, and the pharmacy tells you it’s not covered unless you switch to the generic version, you’re seeing the direct result of insurer pressure. It’s not a random policy-it’s a systematic, nationwide effort by health insurers to cut costs by pushing generic drugs. And providers? They’re caught in the middle, trying to do what’s best for patients while navigating a maze of rules that often feel designed to slow them down, not help them.
How Insurers Enforce Generic Substitution
Insurers don’t just ask providers to use generics-they make it mandatory. The main tools? Formulary tiers, prior authorization, and step therapy. In most plans, generics sit in Tier 1: a $5-$15 copay. Brand-name drugs? Tier 3 or 4, with copays of $40-$100 or more. Some plans won’t cover the brand at all unless you prove the generic won’t work. That’s step therapy: you have to fail on the cheaper option first. In 2022, 90% of all prescriptions in the U.S. were filled with generics, according to the FDA. That’s up from 50% in 2000. The reason? Cost. Generics cost 80-85% less than brand-name drugs. For insurers, that’s billions saved every year. But behind those numbers are real people and real clinical decisions.What Providers Actually Do
Providers aren’t passive recipients of these rules. They’ve adapted-often in ways that add hours to their workday. Many now pre-fill electronic prior authorization (ePA) requests with clinical notes before they even hit the prescription screen. One cardiologist in Minnesota told the AMA that he now includes a full paragraph of clinical justification on every brand-name script, even when he doesn’t think it’s needed. Why? Because last year, an insurer denied coverage for a patient with documented GI sensitivity to the generic version. It took three appeals and 22 days. In that time, the patient had two ER visits for bleeding. A 2023 MGMA survey found physicians spend an average of 16.9 minutes per prior authorization request. That’s not just time-it’s mental load. Multiply that by 15-20 requests a day, and you’re looking at over five hours a week just fighting insurance systems. And that’s not counting the calls to case managers, the paperwork, the appeals. Some practices have hired dedicated prior authorization staff. Medium-sized clinics now spend an average of $112,400 per year per full-time employee just to handle these requests. It’s a hidden cost of care-one that doesn’t show up on patient bills but eats into provider margins.When Generics Don’t Work-And Insurers Won’t Budge
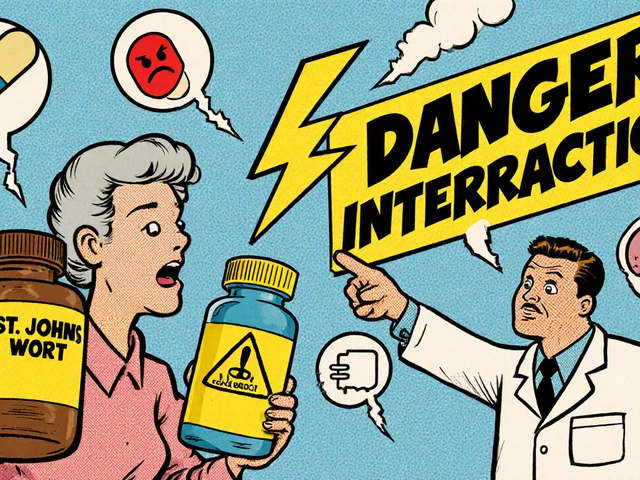
Not all drugs are created equal. For medications with a narrow therapeutic index-like levothyroxine, warfarin, or certain seizure drugs-small differences in absorption can mean treatment failure or even danger. The AMA reports 28% of physicians have seen adverse outcomes after an insurer-mandated switch to a generic version of these drugs. One psychiatrist in California described a patient on a brand-name antipsychotic who stabilized after months of trial and error. The insurer switched her to a generic. Within weeks, she relapsed. The insurer denied the appeal, saying the generic was "bioequivalent." But bioequivalent doesn’t mean identical in effect. The FDA allows generics to vary by 80-125% in blood concentration compared to the brand. For some patients, that’s enough to trigger psychosis. Providers have learned to fight back with data. The AMA says appeals with objective clinical evidence-lab results, hospital records, documented side effects-are 37% more likely to succeed. Generic substitution isn’t always the issue. It’s the lack of clinical context in the insurer’s decision-making.
State Laws Are Changing the Game
Not all insurers operate under the same rules. California’s AB 347, effective January 2024, forced a major shift. It requires insurers to approve step therapy exceptions within 72 hours for urgent cases and 5 business days otherwise. The result? Approval rates jumped from 45% to 92% on first submission. Arizona took it further with HB 2175, signed in May 2025. It bans insurers from using AI alone to deny care based on medical necessity. A medical director must review every denial. Implementation is required by June 30, 2026. These laws are rare. Only 34 states introduced prior authorization reform bills in 2024-2025. Most providers still face a patchwork of conflicting rules. One insurer’s definition of "medical necessity" might be a 10-page document. Another’s might be a checkbox in an algorithm.Who’s Really in Control?
Behind every insurer is a Pharmacy Benefit Manager (PBM)-CVS Caremark, Express Scripts, OptumRx. These companies control 85% of formularies in the U.S. They decide which drugs get covered, at what tier, and under what conditions. Many PBMs are owned by the same companies that run the insurers (like UnitedHealthcare owning Optum). That vertical integration means the pressure to push generics isn’t just about saving money-it’s about profit. And then there are the coupons. When Lipitor went generic in 2010, Sun Life reported a 138% spike in "no substitution" claims. Why? Patients were using manufacturer coupons to pay less for the brand than the generic cost after insurance. Insurers had to scramble to block those coupons, often by excluding the brand entirely from coverage.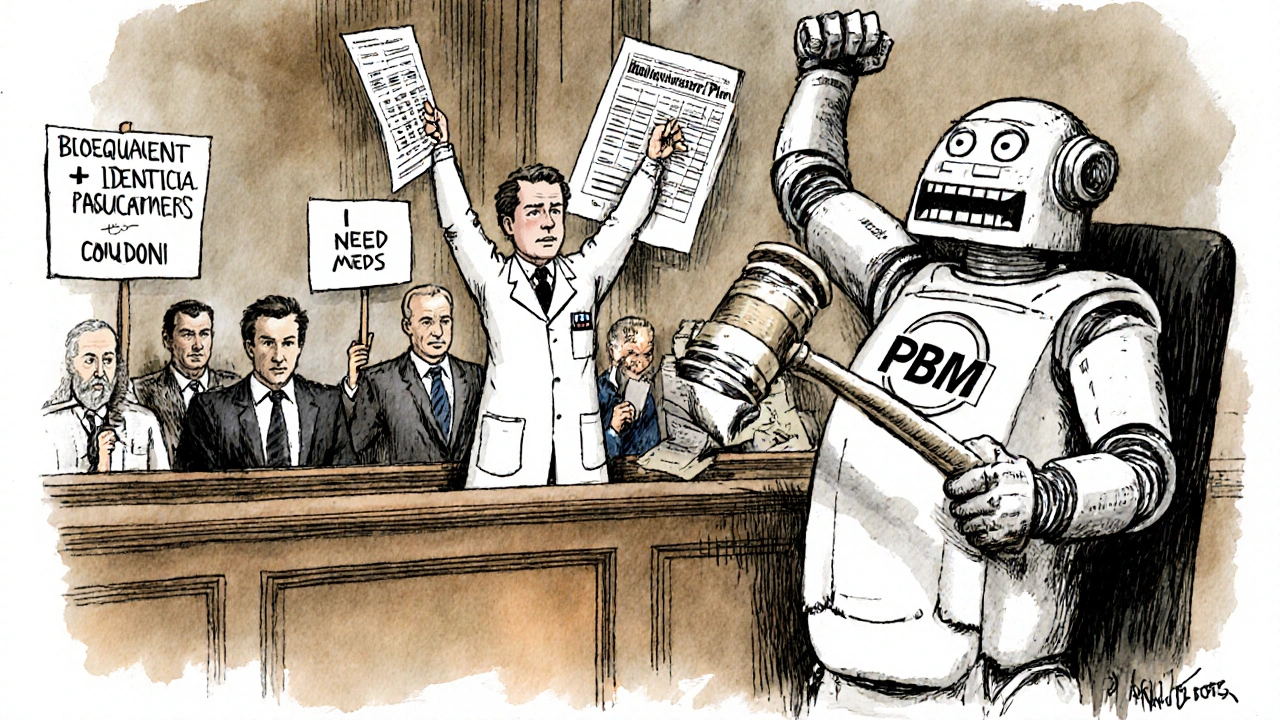
What Works for Providers
The most successful providers have built systems around the chaos:- They use EHR-integrated ePA tools that auto-populate forms with clinical data.
- They keep template letters for common exceptions (68% of physicians use them).
- They cultivate relationships with specific insurer case managers-knowing who to call, when to call, and how to phrase requests.
- They document everything: lab values, prior treatment failures, side effect logs. Subjective statements like "the patient doesn’t feel right" rarely win.




8 Comments
Ugh, I just had to fight my insurer for 3 weeks because they switched my mom’s levothyroxine to a generic and she started having heart palpitations. 🤮 They kept saying "bioequivalent" like that’s some magical word that erases reality. My mom’s not a lab rat. She’s a person who just wants to not feel like she’s dying every morning. I’m done being polite about this.
Y’know, I find it fascinatin’ how the system’s designed to optimize for cost-efficiency, yet utterly ignores the messy, beautiful chaos of human biology. 🤔 I mean, sure, generics are 80% cheaper-but what if the 20% difference is the difference between a patient sleeping at night… or ending up in the ER? It’s like trying to replace a Stradivarius with a Walmart violin and then being shocked when the symphony sounds like a cat in a blender. 🎻🐱
My doc just told me he spends more time on prior auth than actual patient care. And you know what? I don’t blame him. I’ve had to call my insurance 12 times just to get a refill on my antidepressant. They kept asking for "clinical justification" like I’m a criminal trying to smuggle serotonin. I’m not asking for a yacht-I’m asking to not cry in the shower every day.
Okay but have y’all seen the PBM profits?? 😳 CVS Caremark made $4.7 BILLION last year off this crap. And we’re supposed to feel bad for the insurers?? 🤡 They’re not the ones getting sued for denying life-saving meds. Also, I’m so done with the "bioequivalent" excuse. My brain doesn’t care if it’s 85% the same. It needs the ONE that works. 🙄 #StopTheGenericGreed
THIS IS WHY AMERICA IS FALLING APART. We let these corporate suits in New York and Connecticut dictate how doctors treat patients. We’re not China. We’re not Canada. We’re AMERICA. And we don’t let bean counters decide who lives and who dies. If your kid needs the brand-name seizure med, you damn well better get it. No more "step therapy"-that’s just medical neglect with a spreadsheet. 🇺🇸🔥
Hey, I know it’s frustrating-but you’re not alone. 🙌 I’m a nurse in Texas, and I’ve seen firsthand how providers are bending over backwards to fight this. The good news? You CAN win. Document everything. Use the templates. Call the case manager by name. And never, ever give up. One of my patients got her brand-name antipsychotic approved after 17 appeals. She’s back to painting again. That’s the win. Keep going. 💪❤️
Just wanted to say-this whole thing reminds me of how my abuela used to say, "El sistema no es malo, pero los que lo manejan sí." The system isn’t broken, but the people running it? They’ve forgotten what healing looks like. I’ve seen doctors cry in their cars after a denied appeal. We’re not just talking about pills-we’re talking about dignity. Maybe if PBMs had to sit in a clinic for a week, they’d understand. 🙏
The data presented in this article is methodologically sound and aligns with peer-reviewed studies from JAMA Health Forum and NEJM Catalyst. The statistical trends regarding prior authorization burden and generic substitution outcomes are consistent with national benchmarks. A nuanced policy response, informed by empirical evidence, is warranted.
Write a comment