Medication Swelling Risk Checker
1
Describe your swellingSwelling in your ankles, feet, or hands after starting a new medication isn’t always harmless. It’s common-but that doesn’t mean you should ignore it. Thousands of people experience this every year, and most assume it’s just a "side effect" they’ll get used to. But sometimes, that swelling is a warning sign. It could be your body telling you something more serious is going on. Knowing when to act can prevent hospital visits, heart complications, or even life-threatening situations.
What Exactly Is Medication-Related Edema?
Edema is fluid trapped in your tissues, causing visible puffiness. It most often shows up in the legs, ankles, or feet, but can also appear in the hands, face, or even lungs. When it’s caused by a drug, it’s called medication-induced edema. This isn’t rare. In the U.S. alone, about 4.4 million people deal with this each year. The good news? Most cases are mild. The bad news? Many people don’t realize how dangerous it can become if left unchecked.
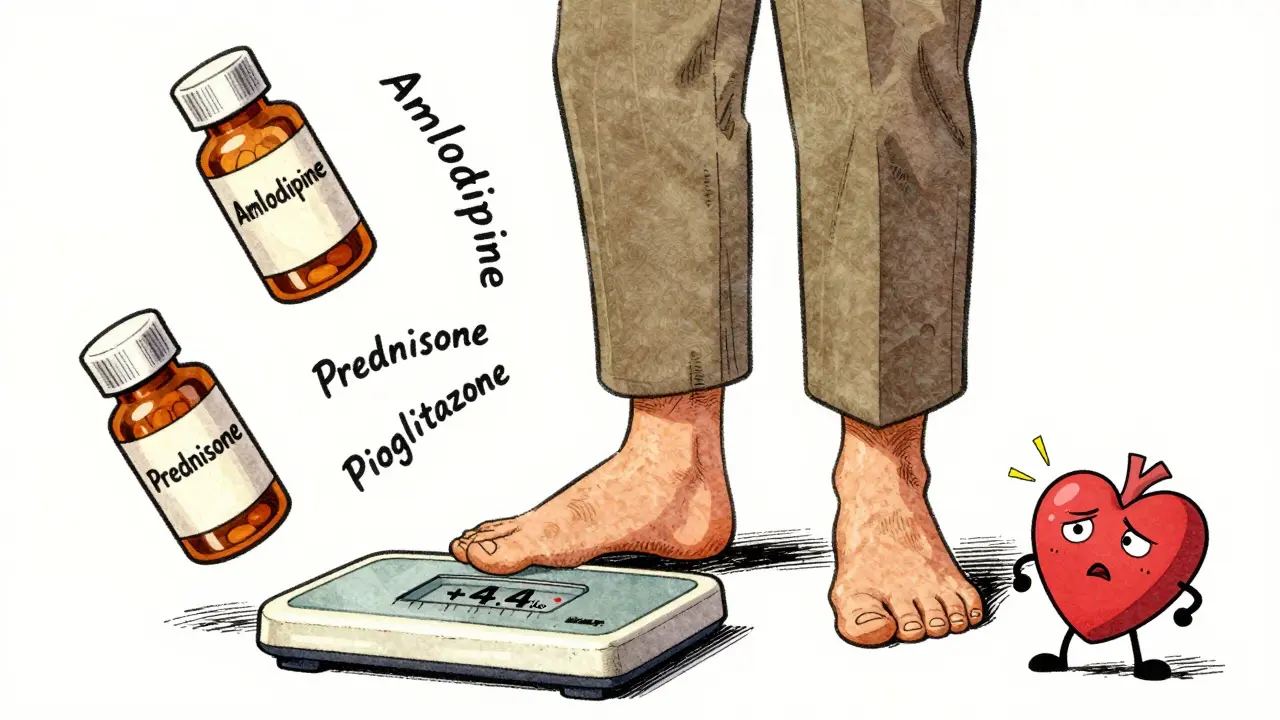
Some medications make tiny blood vessels leak fluid into nearby tissues. That’s it. Simple. But the drugs that do this aren’t harmless. Common offenders include:
- Calcium channel blockers like amlodipine (Norvasc) - causes swelling in 10-20% of users. At 10mg daily, nearly 1 in 4 people notice puffy ankles.
- Gabapentin and pregabalin - used for nerve pain and seizures. About 6-8% of users develop noticeable swelling.
- Thiazolidinediones like pioglitazone (Actos) - prescribed for type 2 diabetes. Fluid retention is so common, it’s listed as a major risk in the drug’s safety label.
- NSAIDs - ibuprofen, naproxen. Even over-the-counter versions can cause mild swelling in 3% of regular users.
- Corticosteroids like prednisone - especially when taken above 20mg daily for more than two weeks. Up to 30% of users retain fluid.
- Hormonal medications - birth control pills and estrogen therapy can trigger swelling in 5-15% of users.
None of these drugs are "bad." They save lives. But their side effects aren’t always obvious until the swelling starts. And that’s where things get tricky.
When Is Swelling Just a Side Effect - and When Is It Dangerous?
Not all swelling is the same. If you’ve just started a new medication and notice mild puffiness in your ankles after standing all day, it might be harmless. But if the swelling changes - gets worse, spreads, or comes with other symptoms - it’s time to pay attention.
Here’s how to tell the difference:
- Benign medication swelling: Usually bilateral (both legs), pitting (leaves an indentation when pressed), worse at the end of the day, improves with rest or elevation, no pain or redness.
- Warning signs: One-sided swelling, sudden weight gain (over 2-3 pounds in 2-3 days), shortness of breath, chest tightness, abdominal bloating, dizziness, or confusion.
Why does this matter? Because these symptoms could mean something far worse:
- Heart failure: When the heart can’t pump well, fluid backs up into the legs and lungs. People with heart failure often have swelling that gets worse at night, and they may need to sleep propped up on pillows. A 2023 American Heart Association report says 90% of advanced heart failure patients show this kind of swelling.
- Kidney disease: Nephrotic syndrome causes massive swelling, especially around the eyes and legs. It’s linked to high protein loss in urine - over 3.5 grams in 24 hours. This isn’t just puffiness. It’s a sign your kidneys are failing.
- Deep vein thrombosis (DVT): A blood clot in the leg causes swelling in just one leg, often with warmth, redness, or pain. It can lead to a pulmonary embolism - a life-threatening emergency.
- Liver cirrhosis: Fluid builds up in the belly (ascites) and legs. If you’ve had long-term liver damage, new swelling could mean your condition is worsening.
Dr. Mark Danchenko, a cardiologist at Johns Hopkins, says: "Any new bilateral swelling in someone on amlodipine should trigger a heart check - especially if they’re also short of breath or can’t lie flat." That’s not an overreaction. That’s standard care.
Who’s at Highest Risk?
You might think young, healthy people don’t get dangerous edema. But age and other conditions change everything.
The American Geriatrics Society’s 2023 Beers Criteria lists amlodipine, gabapentin, and pioglitazone as "potentially inappropriate" for people over 65 - not because they’re unsafe, but because older adults are far more likely to develop severe swelling. In fact, 40% of patients over 75 experience noticeable edema from these drugs, compared to just 15% under 65.
Other high-risk groups:
- People with existing heart, kidney, or liver disease
- Those taking multiple medications (polypharmacy)
- Patients on long-term steroids or diabetes drugs
- Women on hormone therapy or birth control
One Reddit user, u/MedWatcher2023, shared how their amlodipine-induced swelling became so severe they couldn’t wear shoes. Switching to losartan - a different blood pressure drug - fixed it in two weeks. But not everyone gets that lucky. Another user, HeartPatient99, said their doctor dismissed their pioglitazone swelling as "just a side effect" - until they ended up in the hospital with fluid in their lungs.

What You Can Do Right Now
If you’re experiencing swelling and you’re on one of these medications, don’t panic - but don’t wait either. Here’s what to do:
- Track your weight daily. A gain of 2.2 pounds (1 kg) in 24 hours or 4.4 pounds (2 kg) in a week is a red flag. Keep a log - even a note on your phone works.
- Elevate your legs. Lie down and prop your feet above heart level for 15-20 minutes, four times a day. Studies show this can reduce ankle swelling by 1.5 cm in just two days.
- Wear compression socks. 20-30 mmHg pressure socks reduce fluid buildup by 30% in under a week. They’re not glamorous, but they work.
- Reduce sodium. The average American eats 3,400mg of sodium a day. The goal is under 2,000mg. Cut processed foods, canned soups, and salty snacks. You’ll see a difference in 72 hours.
- Don’t stop your meds on your own. If you think a drug is causing swelling, talk to your doctor. Stopping suddenly can be dangerous - especially with blood pressure or diabetes meds.
One user on Reddit, u/SwellingSolution, said compression socks and leg elevation cut their amlodipine swelling by 80% - without changing their medication. That’s a win.
When to Call Your Doctor - Immediately
Don’t wait for your next appointment. Call your provider or go to urgent care if you have:
- Swelling in only one leg (could be a blood clot)
- Sudden weight gain over 5% in a month (e.g., 10 pounds for a 200-pound person)
- Shortness of breath, especially when lying down
- Chest pain or rapid heartbeat
- Swelling with fever, redness, or warmth
- Abdominal swelling with yellowing skin or dark urine (signs of liver issues)
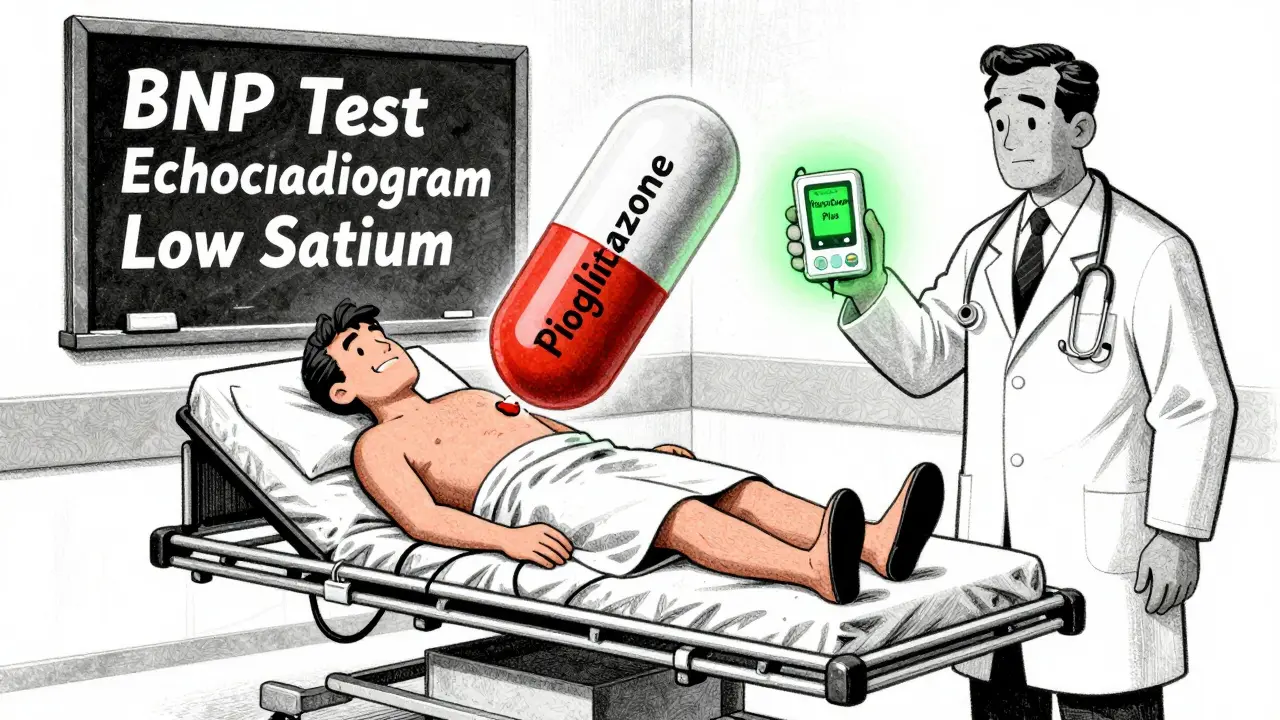
Dr. Sarah Wood, an endocrinologist at Mayo Clinic, says: "Pioglitazone-induced edema requires immediate discontinuation if you gain more than 5% of your body weight in a month or develop trouble breathing." That’s not a suggestion. That’s a medical emergency.
The FDA has even required black box warnings on thiazolidinediones like pioglitazone because of this exact risk. If you’re on one of these drugs and you’re over 65 or have heart disease, your doctor should be monitoring you closely - not dismissing your swelling.
What’s Being Done to Fix This?
This isn’t just a patient problem - it’s a system problem. In 2022, medication-related edema led to over 5 million doctor visits in the U.S. and cost $4.8 billion. But change is happening.
- The FDA approved the VascuComp Plus wearable device in March 2023. It uses bioimpedance to detect fluid buildup before you even notice swelling - with 92% accuracy.
- Mayo Clinic started using EHR alerts in January 2022 to flag patients on high-risk meds. Result? A 22% drop in severe edema cases.
- New guidelines from the American Heart Association now include blood tests (like BNP levels) and heart scans to distinguish drug swelling from heart failure.
These aren’t futuristic ideas. They’re being used now. And they’re saving lives.
Final Thoughts
Swelling from medication isn’t always an emergency. But it shouldn’t be ignored. Too many people assume it’s just "part of taking pills." It’s not. It’s your body’s signal - and you need to listen.
If you’re on a medication known to cause swelling, pay attention. Track your weight. Elevate your legs. Cut the salt. Talk to your doctor. Don’t wait until you’re gasping for air or your ankles are too swollen to fit into shoes. The difference between a minor side effect and a life-threatening condition is often just a few days - and a few smart actions.
Can medication swelling go away on its own?
Yes, in some cases. Mild swelling from drugs like amlodipine or gabapentin may improve with lifestyle changes - like reducing salt, elevating your legs, or wearing compression socks. But if the swelling doesn’t improve after 2-3 weeks, or gets worse, you shouldn’t wait. Your doctor may need to switch your medication or check for other underlying causes.
Which medications cause the most swelling?
Calcium channel blockers like amlodipine cause swelling in 10-20% of users. Thiazolidinediones (pioglitazone, rosiglitazone) are next, with 4-10% risk. Gabapentin and pregabalin cause swelling in 6-8%, and corticosteroids like prednisone can trigger it in up to 30% of long-term users. Hormonal medications, including birth control and estrogen therapy, also contribute, especially in women over 50.
Is ankle swelling always a sign of heart problems?
No. Ankle swelling can be caused by many things - including prolonged standing, venous insufficiency, or medications. But if you’re over 65, have a history of heart disease, or have other symptoms like shortness of breath or fatigue, it’s a red flag. A 2023 study found that 90% of advanced heart failure patients had bilateral ankle swelling. Don’t assume it’s just age or medication - get it checked.
How long does it take for swelling to go away after stopping the drug?
It varies. For most people, swelling starts to improve within a week after switching or stopping the medication. Some notice changes in 3-5 days. In others, especially if fluid retention was severe or long-standing, it can take 2-4 weeks. Elevation, compression, and low-sodium diet help speed recovery.
Can I still take my medication if I have swelling?
Maybe - but only under medical supervision. If your swelling is mild and you have no other symptoms, your doctor might recommend lifestyle changes first. But if you have weight gain, shortness of breath, or one-sided swelling, continuing the medication could be dangerous. Never stop a prescribed drug without talking to your provider - but don’t ignore warning signs either.
Are compression socks really effective?
Yes. Studies show 20-30 mmHg compression socks reduce leg swelling by 30% in just 7 days. They work by pushing fluid back into circulation, preventing pooling in the lower legs. They’re especially helpful for people on long-term medications like amlodipine or gabapentin. You don’t need to wear them all day - 2-4 hours twice daily can make a noticeable difference.