When your shoulder aches after lifting groceries, or your knee hurts when you kneel to tidy the floor, it’s easy to blame it on "arthritis" or "just getting older." But more often than not, the real culprit is something more specific: bursitis or tendinitis. These aren’t just buzzwords-they’re two very different kinds of joint inflammation that need very different treatments. And mixing them up can make your pain last longer, not shorter.
What Exactly Is Bursitis?
Bursitis is inflammation of the bursae (small fluid-filled sacs that cushion bones, tendons, and muscles near joints). Think of them like tiny water balloons sitting between your bones and skin or tendons. They reduce friction so your joints move smoothly. When they get irritated-usually from repeated pressure or sudden trauma-they swell up and become painful.
The most common spots? Your shoulder (subacromial bursa), elbow (olecranon bursa), hip (trochanteric bursa), and knee (prepatellar bursa). If you’ve ever had a swollen elbow after leaning on it too long, or hip pain when you sleep on that side, you’ve likely experienced bursitis.
Here’s what sets bursitis apart: the pain is often dull, widespread, and worse at night. Lying directly on the sore area? That’s usually the worst part. You might notice swelling or warmth over the joint, and the pain doesn’t always follow a specific movement-it’s more about pressure.
What Exactly Is Tendinitis?
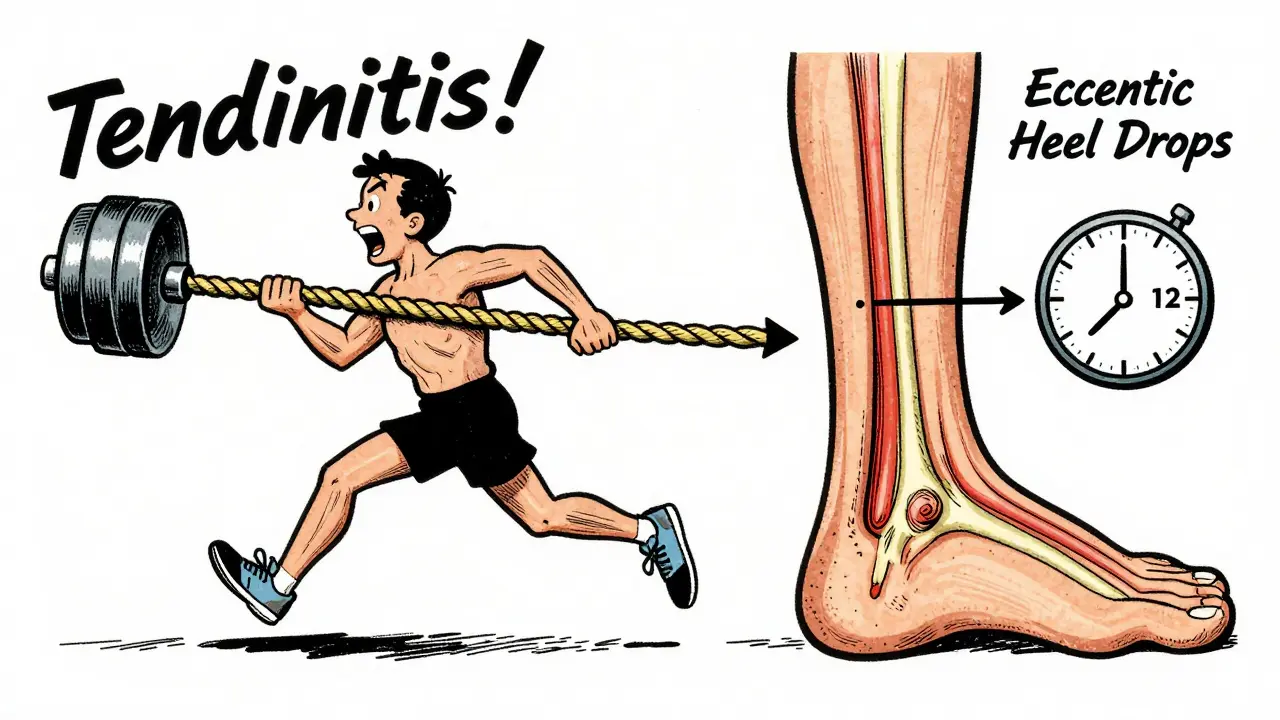
Tendinitis is inflammation of a tendon (the thick, fibrous cord that connects muscle to bone). Unlike bursae, tendons are under constant tension. Every time you lift, reach, or push, your tendons are working. When they’re overused-especially with repetitive motion-they start to fray and inflame.
The usual suspects? The rotator cuff in the shoulder, the Achilles tendon in the heel, and the patellar tendon below the kneecap. If you’re a runner, a painter, a gardener, or someone who types all day, you’re at higher risk.
Tendinitis pain is different. It’s sharp, localized, and gets worse with movement. Try lifting your arm overhead if you have shoulder tendinitis? Ouch. Try jumping or running if your Achilles is inflamed? Pain shoots up the back of your leg. The pain follows the path of the tendon-not just around the joint.
Why Mixing Them Up Makes Things Worse
Here’s the scary part: 65% of shoulder pain cases involve both bursitis and tendinitis together. That’s why so many people get stuck in a cycle of ineffective treatment.
Let’s say you have shoulder pain and assume it’s "rotator cuff tendinitis." You start doing aggressive strengthening exercises-exactly what you shouldn’t do if the real issue is inflamed bursae. Those exercises rub the tendon against the swollen bursa, making everything worse. Meanwhile, if you have bursitis and get a cortisone shot thinking it’s just a "tendon problem," you might be fine. But if you get the same shot for tendinitis? You risk weakening the tendon itself.
Studies show that corticosteroid injections help 78% of bursitis patients within four weeks. But for tendinitis? Only 52% get relief-and 34% actually feel worse after the shot. Why? Because tendons don’t respond well to steroids. They need time, specific loading, and patience.
How Doctors Tell Them Apart
It’s not magic. It’s observation.
A good clinician will ask you to move your joint in specific ways. If pain flares when you lift your arm overhead or reach behind your back, it’s likely tendinitis. If it hurts when you lie on your side or press on the bump near your hip or elbow, it’s probably bursitis.
Ultrasound is now the gold standard for diagnosis. It can show swelling in the bursa, fraying in the tendon, or both-with 92% accuracy. MRI is overkill for most cases. You don’t need a fancy scan unless the pain lasts more than six weeks or doesn’t respond to basic treatment.
And here’s a critical point: 40% of people over 50 have signs of bursitis or tendinitis on MRI-even if they feel fine. That means imaging alone doesn’t diagnose the problem. Symptoms matter more than pictures.
What Actually Works: Treatment That Makes Sense
Both conditions start with the same first step: rest, ice, and avoid the trigger.
- Ice the area for 15 minutes, 3-4 times a day. Use a frozen water bottle-it molds better to your elbow or shoulder.
- Stop doing the thing that hurts. That doesn’t mean total inactivity. Just avoid the motion that causes pain. If typing triggers wrist pain, try voice-to-text for a week.
- NSAIDs like ibuprofen can help, but don’t take them for more than 10-14 days. They mask pain but don’t fix the root cause.
After a few days, gentle movement is key. For bursitis, slow, pain-free range-of-motion exercises help the fluid drain. For tendinitis, you need something called eccentric strengthening. That means slowly lowering a weight, not lifting it.
For example, if you have Achilles tendinitis, you do heel drops: stand on a step, rise up on both feet, then slowly lower the injured foot down. Do 3 sets of 15, twice a day, for 12 weeks. Yes, 12 weeks. No shortcuts.
And here’s the rule most people ignore: keep pain under 3 out of 10 during exercise. If it’s a 5 or higher, you’re doing too much. Pain is your body’s way of saying, "Stop. This isn’t helping."
When to Consider Injections or Surgery
Corticosteroid injections can be helpful-for bursitis. They reduce swelling fast. But for tendinitis? They’re a gamble. Only use them if conservative care fails, and limit them to 2-3 per year. Too many can weaken tendons and lead to rupture.
Surgery? Rare. Fewer than 5% of cases need it. That’s usually only if a tendon has completely torn, or if bursitis becomes infected (which is uncommon).
There’s new hope, though. Platelet-rich plasma (PRP) therapy is showing better long-term results than steroids for chronic tendinitis. One 2023 study found 67% of patients improved at six months with PRP, compared to 42% with steroids. But it costs around $850 per injection-insurance rarely covers it.
Real People, Real Recovery
On Reddit’s r/PhysicalTherapy, one user shared how he misdiagnosed his shoulder pain as "tendinitis" for eight months. He kept doing push-ups and shoulder presses. Pain got worse. Then he saw a physio who found his bursa was swollen. He stopped all lifting, started ice massages, and used posture correction. Within six weeks, he was pain-free.
Another, a 58-year-old gardener with hip bursitis, used a frozen water bottle to roll over her hip every night. She switched from kneeling to using a kneeling pad. Within four weeks, she was back in the garden.
And then there’s Tom Wilcox, a runner who documented his 27-week recovery from Achilles tendinitis. He didn’t just rest. He did 180 eccentric heel drops a day, tracked his pain on a scale, and waited. No injections. No surgery. Just time and consistency.
Who’s Most at Risk?
These conditions don’t pick favorites-but they do have patterns:
- Age 45-64: Risk jumps sharply after 40. Tendons and bursae lose elasticity.
- Repetitive jobs: Construction workers (kneeling → bursitis), musicians (repeated motions → tendinitis), office workers (typing → wrist tendinitis).
- Overtraining: Runners, tennis players, and weekend warriors often push through pain, making inflammation worse.
Workplace injuries are real. In 2022, over 387,000 U.S. jobs reported bursitis or tendinitis-costing the economy $2.1 billion in lost days. That’s not just a medical issue. It’s a workplace safety issue.
What to Avoid
Don’t:
- Ignore pain and "work through it."
- Get an injection without knowing if it’s bursitis or tendinitis.
- Use heat too early. Ice first-heat can increase swelling in the first 48 hours.
- Believe MRI scans tell the whole story. Pain matters more than pictures.
- Start strengthening too soon. Wait until swelling and sharp pain are gone.
What You Can Do Today
Here’s your simple action plan:
- Identify where it hurts. Is it a specific spot you can press? That’s likely bursitis. Does it hurt when you move? That’s likely tendinitis.
- Ice it 3-4 times a day for 15 minutes.
- Stop the activity that makes it worse-for at least a week.
- Try gentle movement. If it hurts more than 3/10, stop.
- If it doesn’t improve in 10 days, see a physical therapist. Don’t wait months.
Most cases get better in 4-8 weeks with the right approach. The ones that drag on? Those are the ones where someone ignored the difference between bursitis and tendinitis.
Can bursitis and tendinitis happen at the same time?
Yes. In fact, about 65% of shoulder pain cases involve both. The inflamed bursa can rub against the irritated tendon, making the pain worse and harder to treat. That’s why accurate diagnosis matters-treating one without addressing the other delays recovery.
Is rest the best treatment for both conditions?
Rest is the first step, but not the whole solution. For bursitis, rest reduces swelling. For tendinitis, rest alone can make the tendon weaker. After a few days, you need gentle movement-then specific strengthening. Total inactivity for weeks can backfire.
Do cortisone shots cure tendinitis?
No. Cortisone shots reduce inflammation temporarily, but they don’t repair the tendon. For tendinitis, they help about half the time-and can even weaken the tendon if overused. Eccentric exercises are far more effective long-term. For bursitis, though, shots often work well.
How long does it take to recover from tendinitis?
It depends. Mild cases improve in 4-6 weeks. Chronic tendinitis, especially in the Achilles or shoulder, often takes 12-16 weeks. That’s because tendons heal slowly. The key is consistency-daily exercises, even if they feel slow.
Can I prevent bursitis and tendinitis?
Yes. Avoid repetitive motions without breaks. Use padding when kneeling. Warm up before activity. Strengthen muscles around joints to reduce strain. And listen to your body-if something hurts during daily tasks, adjust before it becomes a problem.
If you’ve been told your pain is "just aging," don’t accept that. Bursitis and tendinitis are treatable. But only if you know which one you have-and what to do next.