When cancer spreads or treatments like chemotherapy and radiation take their toll, pain doesn’t just come and go-it becomes part of daily life. For nearly half of all cancer patients, pain is moderate to severe. And for more than a third, it spikes unexpectedly, breaking through even the strongest meds. This isn’t just discomfort. It’s exhaustion, sleeplessness, and the slow erosion of what little normalcy remains. The good news? We have more tools than ever to fight it-not just one, but many, working together.
How Cancer Pain Works (And Why It’s Not Just One Thing)
Cancer pain isn’t simple. It can be sharp, burning, aching, or feel like electric shocks. That’s because it’s often a mix of different types. Nociceptive pain comes from tumors pressing on bones, organs, or nerves. Neuropathic pain happens when nerves are damaged by the cancer itself or by chemo. And then there’s breakthrough pain, sudden and intense, even when you’re on regular meds. This complexity is why treating it with just one drug rarely works long-term.The World Health Organization’s three-step analgesic ladder, first introduced in 1986, was a game-changer. It gave doctors a clear path: start mild, step up as needed. But today, we know better. Many patients need more than one approach from day one. A 2023 study found that 42% of cancer patients have mixed pain types right from diagnosis. Waiting to escalate can mean weeks of unnecessary suffering.
Opioids: Powerful, But Not Perfect
For severe cancer pain, opioids are still the gold standard. Morphine, oxycodone, and fentanyl patches can slash pain scores by 4 points on a 10-point scale-something NSAIDs or weak opioids simply can’t match. But they come with a heavy price tag.Eighty-one percent of patients on opioids get constipated. More than half feel nauseous. Nearly half get drowsy. And while these side effects can be managed, many patients still quit because it feels worse than the pain. In one 2024 survey, 78% of patients said they still struggled with constipation even on daily laxatives. That’s not just inconvenient-it’s debilitating.
Not all opioids are the same. Tramadol, often used for moderate pain, only works well in people with a specific gene (CYP2D6). About 7% of people can’t convert it to its active form at all. That means for them, it’s useless-and they waste weeks trying before switching. That’s why leading cancer centers now test for this gene before prescribing codeine or tramadol.
Guidelines have shifted, too. The CDC now allows cancer patients to take up to 90 mg of morphine equivalents daily-higher than the old 50 mg cap-because pain control matters more than arbitrary limits. Still, access is uneven. In 63 countries, opioids are hard to get due to fear, regulation, or cost. In low-income regions, patients often go without.
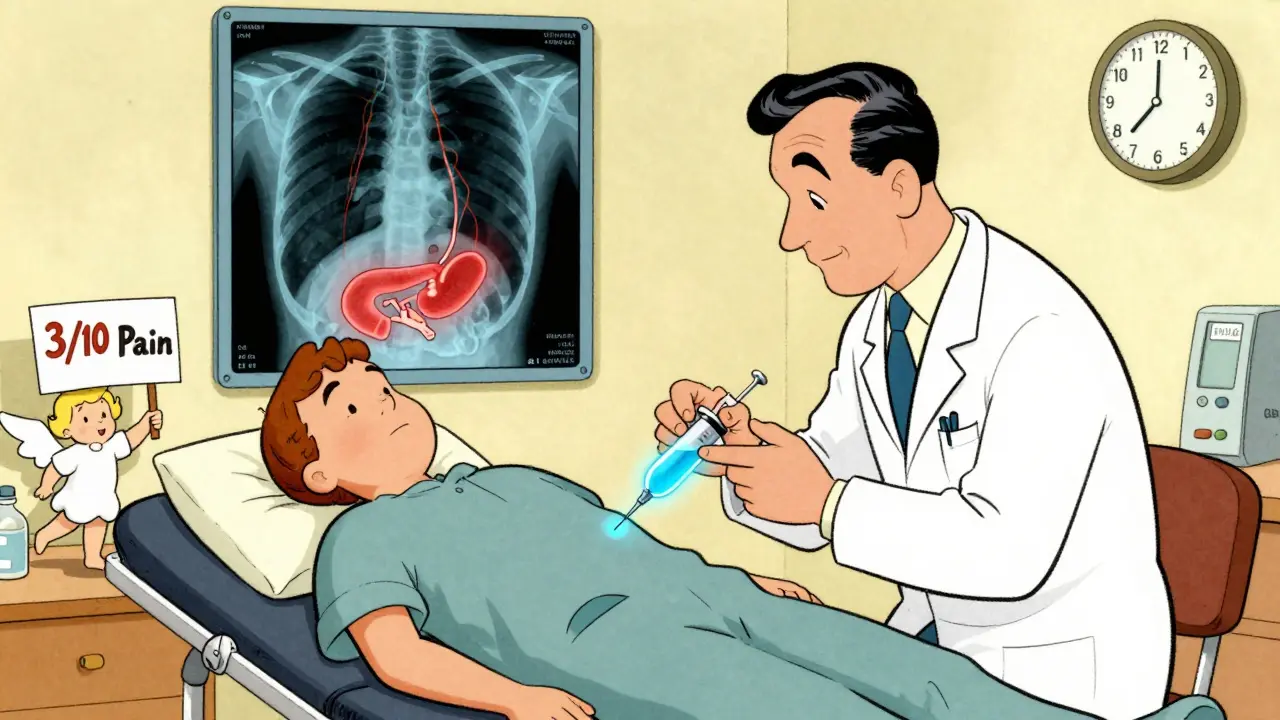
Nerve Blocks: Targeted Relief When It Counts
If your pain is localized-say, from a tumor pressing on your pancreas or spine-nerve blocks can be life-changing. These aren’t magic. They’re precise injections that shut down pain signals at their source.A celiac plexus block, for example, targets nerves around the pancreas. For pancreatic cancer patients, it can reduce pain from an 8/10 to a 3/10-and keep it there for up to four months. One study showed median relief lasting 132 days. The catch? It’s not a one-time fix. Most people need repeat injections every 3 to 6 months.
Epidural catheters, often used after surgery or for advanced spine metastases, deliver pain meds directly to the spinal cord. They’re highly effective, with success rates of 75% or higher. But they require hospital placement and ongoing care. Peripheral nerve blocks, using thin catheters taped to the skin, let patients control their own pain relief at home. These are ideal for localized pain from bone metastases in arms or legs.
Despite their power, only 22% of patients who could benefit from nerve blocks actually get them. Why? Lack of access, fear of the procedure, or doctors who don’t know how to refer. A 2024 European review called this a “systemic failure.”
Integrative Care: The Quiet Heroes of Pain Relief
While opioids and nerve blocks tackle the physical fire, integrative therapies help patients breathe through it.Acupuncture has the strongest evidence. A 2024 review of 17 studies found it reduced cancer pain by 38.7% on average. Patients reported less nausea, better sleep, and lower opioid use. One Reddit user shared that acupressure wristbands cut her chemo nausea by 70% and halved her opioid intake.
Mindfulness and meditation don’t erase pain-but they change how the brain reacts to it. In 54 studies reviewed, 87% of patients using mindfulness-based stress reduction reported meaningful improvement. It’s not about ignoring pain. It’s about not letting it take over your mind.
Massage and reflexology are gentler. They don’t reduce pain scores as much as acupuncture, but they lower anxiety and improve quality of life. In one survey, 68% of patients using acupuncture said it helped “meaningfully.” Only 55% said the same for massage. But massage was more accessible and affordable.
Cannabinoids? They’re trending. A 2023 meta-analysis showed they reduced pain 32% more than placebo. But they didn’t beat opioids-and 41% of users quit because of dizziness or brain fog. They’re not a first-line option, but for some, they’re a useful backup.
Monoclonal antibodies like denosumab (Xgeva) are new players. They target bone pain specifically, reducing it by nearly half in trials. And they cause far fewer stomach issues than opioids. Sales hit $3.2 billion in 2024. But they’re expensive and only for certain types of cancer.
Putting It All Together: The Modern Approach
The best cancer pain plan doesn’t rely on one tool. It’s a blend. A patient with advanced pancreatic cancer might start with a fentanyl patch for constant pain, a nerve block for breakthrough spikes, daily acupuncture to reduce nausea, and mindfulness to handle the emotional toll. That’s multimodal care.Studies show this approach cuts hospital readmissions by 23% and helps 38% more patients stick with their cancer treatments. Why? Because when pain is under control, people can eat, sleep, and keep going.
It’s not about choosing between opioids and acupuncture. It’s about using both. The WHO updated its guidelines in 2024 to officially recommend integrative therapies alongside meds. The National Comprehensive Cancer Network says the same: acupuncture isn’t “alternative.” It’s part of standard care.
What You Can Do Right Now
If you or someone you love is dealing with cancer pain:- Ask for a pain assessment every time you see your oncologist. Use a 0-10 scale. Don’t say “it hurts.” Say “it’s a 7.”
- Request a referral to palliative care. It’s not just for end-of-life. It’s for improving life now.
- Ask if nerve blocks are an option for your type of pain. Don’t assume they’re too risky or unavailable.
- Try acupuncture or mindfulness-even if you’re skeptical. Many clinics offer free or low-cost sessions.
- Track your pain and side effects. Use a notebook or the free Cancer Pain Relief app (downloaded over 147,000 times).
- Speak up about constipation. If laxatives aren’t working, ask about newer options like methylnaltrexone.
There’s no shame in needing help. Pain isn’t a sign of weakness. It’s a signal that your body needs support. And with today’s tools, you don’t have to suffer in silence.
What’s Coming Next
The future of cancer pain care is personal. AI is being trained to predict pain spikes before they happen, using data from electronic records. By 2030, genetic testing for CYP2D6 metabolism will be routine in most European centers. Blockchain systems are being tested to safely track opioid prescriptions and prevent misuse without blocking access for patients who need them.One thing won’t change: the goal. It’s not just to numb the pain. It’s to help people live-fully, clearly, and with dignity-through the hardest parts of their journey.
Are opioids safe for long-term cancer pain?
Yes, when used correctly under medical supervision. Unlike in chronic non-cancer pain, addiction is rare in cancer patients using opioids for legitimate pain. The bigger risks are side effects like constipation, nausea, and drowsiness-but these can be managed. Guidelines now support higher doses for cancer patients, with regular monitoring to ensure safety and effectiveness.
Can nerve blocks cure cancer pain?
No, nerve blocks don’t cure cancer. They interrupt pain signals from specific nerves to give relief. For some, like those with pancreatic cancer, the relief can last months. But because the cancer keeps growing, the pain often returns, and repeat blocks are needed. They’re a powerful tool for control, not a cure.
Is acupuncture really effective for cancer pain?
Yes, multiple high-quality studies show acupuncture reduces cancer-related pain, nausea, and fatigue. In one review of 17 trials, it lowered pain scores significantly compared to no treatment. It’s now recommended by the WHO and NCCN as part of standard care. Many patients find it helps them reduce opioid use, which lowers side effects.
Why aren’t nerve blocks used more often?
Access is the main barrier. Not all hospitals have pain specialists trained in nerve blocks. Insurance coverage varies. Some doctors aren’t aware of the evidence. And patients often don’t know to ask. In Europe and the U.S., only about 22% of eligible patients receive them-despite 79% success rates in those who do.
Can I use cannabis instead of opioids for cancer pain?
Cannabis can help some people, especially with nausea and mild to moderate pain. But studies show it’s not stronger than opioids for severe cancer pain. It also causes dizziness and brain fog in about 40% of users. It’s best used as a supplement-not a replacement-for standard pain meds, unless your doctor advises otherwise based on your specific case.
What should I do if my pain isn’t improving?
Speak up immediately. Don’t wait until your next appointment. Ask for a pain specialist or palliative care consult. Request a full pain assessment-including type, location, triggers, and what helps. Your current plan might need tweaking: maybe you need a nerve block, a different opioid, or integrative support. Pain that doesn’t respond to treatment is a red flag that needs urgent attention.






9 Comments
I’ve seen this too many times. One week they say opioids are fine, next week they’re villains. Meanwhile, I’m lying awake wondering if my pain is ‘too much’ or if I’m just being dramatic. I don’t need a lecture. I need relief. And sometimes, that’s just a patch and a quiet room.
While the article presents a comprehensive overview of multimodal pain management, it lacks critical analysis of cost-benefit ratios across global healthcare systems. The assertion that integrative therapies are ‘standard care’ is misleading without addressing reimbursement disparities. In the U.S., acupuncture coverage varies by state and insurer, creating de facto inequity. Furthermore, the 32% pain reduction attributed to cannabinoids is statistically significant but clinically marginal when compared to opioid efficacy. Without granular data on patient-reported outcomes over time, such claims risk overpromising.
My aunt had the celiac block. It was like someone turned off a loud alarm inside her. She didn’t smile more, but she stopped flinching when she breathed. That’s all I needed to see. She still had bad days, but now she could sit with us at dinner. No big speeches. Just… quieter nights.
Y’all act like opioids are the devil but then act shocked when someone’s in agony. My cousin died because they waited 3 months to give her morphine ‘cause of ‘addiction fears’. That’s not medicine. That’s cruelty wrapped in paperwork. They let people suffer like animals while bureaucrats debate guidelines. Wake up. Pain ain’t optional. And neither is help.
Oh wow, so now acupuncture is ‘evidence-based’ but only if it reduces opioid use? Interesting. So the real goal isn’t pain relief-it’s opioid reduction? That’s not patient-centered. That’s cost-cutting with a yoga mat. And don’t get me started on ‘mindfulness’ being sold as a cure for bone metastases. I’ve seen people try it. They come back saying, ‘I still hurt, but now I feel guilty for being angry about it.’ Thanks, but no thanks.
ok so i read this whole thing and i just wanna say… why is everyone so scared of opioids?? i mean like… if you have cancer and your bones are on fire, why are we still whispering about ‘addiction’ like its a dirty word?? i had a friend on fentanyl and she said it was the first time in months she slept without crying. but her doc kept giving her ‘alternatives’ like… crystals?? i swear to god. also constipation is the worst. like… i get it. but can we just… fix that too??
These integrative therapies are a luxury for those who can afford them. In America, a single acupuncture session costs more than a week’s worth of generic gabapentin. We cannot allow the wealthy to buy comfort while the poor are told to ‘meditate through it.’ This article romanticizes access. Real medicine is not a boutique service. Pain management must be universal or it is unjust.
Let me tell you about my mum. She had breast cancer spread to her spine. They gave her morphine, sure-but she also did yoga every morning with a video on her tablet, and she’d rub lavender oil on her wrists. And she’d talk to her dead dad while she did it. Not because she believed in ghosts-but because it made her feel like she wasn’t alone. That’s not ‘alternative.’ That’s human. Pain isn’t just a number on a scale. It’s loneliness wrapped in aching bones. We treat the body like a machine, but it’s a heart with bruises. Nerve blocks? Great. Acupuncture? Sure. But what saved her was knowing someone sat with her in silence, holding her hand, not trying to fix it-just being there. That’s the part no study measures.
Hey everyone-just wanted to say this post is a lifeline. If you’re reading this and you’re scared to ask for help? Please, do it. Your pain matters. Ask for the block. Ask for the acupuncturist. Ask for the palliative care team. They’re not giving up on you-they’re fighting for your quality of life. And if your doctor says no? Find another one. You deserve to breathe. 💪❤️
Write a comment