When you have chronic kidney disease (CKD), even a small change in your kidneys’ function can be dangerous. Acute Kidney Injury (AKI) on top of CKD isn’t just a temporary setback-it can lead to permanent damage, dialysis, or even death. The biggest threats? Contrast dye used in imaging scans and common medications you might not think twice about. Avoiding these isn’t optional. It’s survival.
What Happens When AKI Hits CKD?
CKD means your kidneys are already working at reduced capacity-maybe 30%, 40%, or even less of what they should. When something like contrast dye or an antibiotic pushes them further, they can’t recover. This is AKI on CKD. It’s not a new disease. It’s a crisis layered on top of an existing one.
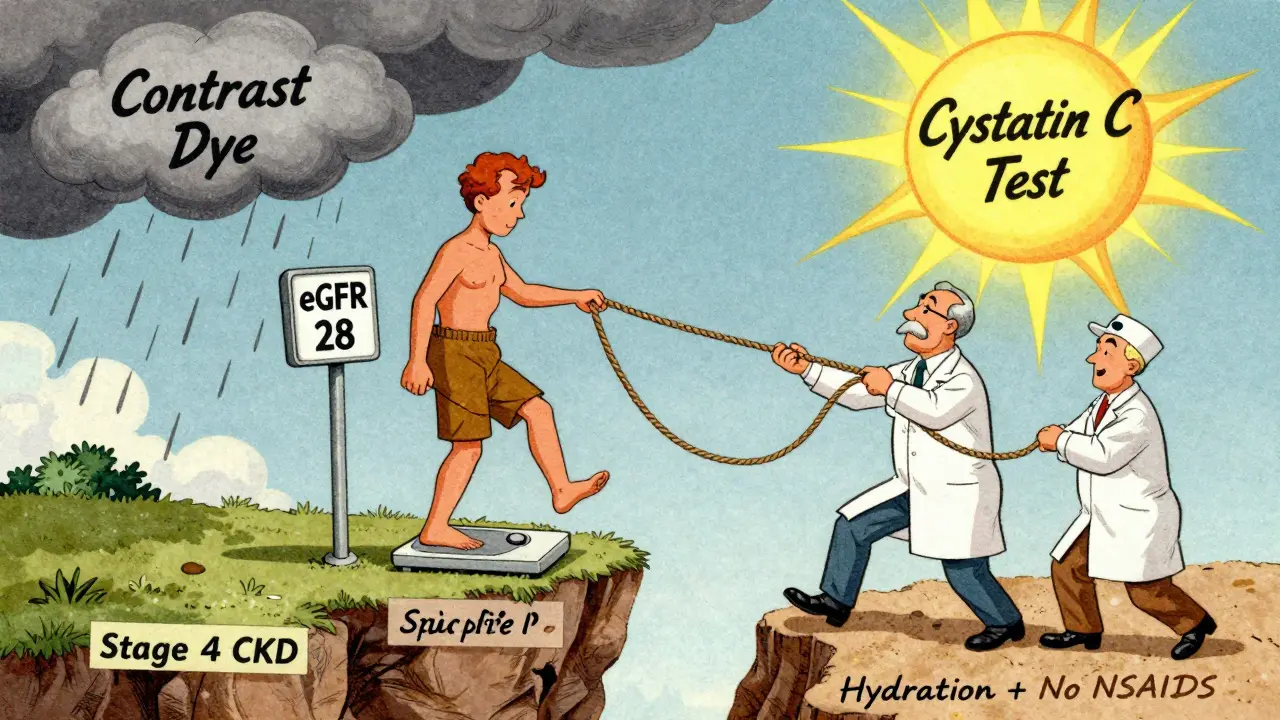
The KDIGO 2012 guidelines define AKI as a sudden drop in kidney function-seen as a rise in serum creatinine by 0.3 mg/dL or more within 48 hours, or a 50% jump from your baseline. If you’re already in CKD stage 3 or worse (eGFR below 60), you’re in the danger zone. Studies show up to 50% of these patients develop contrast-induced kidney injury after a CT scan with iodinated dye. And that’s just one trigger.
Contrast Dye: The Silent Threat
CT scans, angiograms, and other imaging tests often use iodinated contrast to make blood vessels and organs show up clearly. For someone with healthy kidneys, this is routine. For someone with CKD, it’s risky.
The risk isn’t the same for everyone. If you have diabetes and CKD, your chances of AKI jump to 20-50%. If you’re also dehydrated or have heart failure, it’s even higher. That’s why guidelines say: avoid contrast if you can. Use ultrasound or MRI instead. If you absolutely need a CT scan, use the smallest possible dose-usually under 100 mL-and hydrate before and after.
Hydration isn’t just drinking water. It’s IV fluids at 1.0-1.5 mL per kg per hour for 6-12 hours before and after the scan. Normal saline is the gold standard. Don’t waste time on expensive alternatives like albumin or hydroxyethyl starch-KDIGO says they don’t help. And forget about sodium bicarbonate. Recent studies show it’s no better than plain saline.
Nephrotoxic Medications: The Everyday Killers
You might be taking these without knowing they’re dangerous:
- NSAIDs (ibuprofen, naproxen, celecoxib): These are the #1 preventable cause of AKI in CKD patients. A 2021 study in the Veterans Health Administration found NSAID use increases AKI risk by 2.5 times. Even a few days of OTC painkillers can trigger kidney failure in someone with CKD.
- ACE inhibitors and ARBs (lisinopril, losartan): These are lifesavers for blood pressure and heart protection-but they reduce blood flow to the kidneys. In AKI, they can make things worse. Don’t stop them abruptly. Work with your doctor to adjust the dose, not cancel it.
- Aminoglycosides (gentamicin, tobramycin): Used for serious infections, these drugs are directly toxic to kidney cells. Up to 25% of patients on a full course develop damage.
- Vancomycin: Often used for resistant infections. Risk spikes when blood levels go above 15 mcg/mL. Monitoring is critical.
- Amphotericin B: A powerful antifungal. Nephrotoxicity hits 30-80% of users. It’s a last-resort drug for a reason.
Here’s the hard truth: 30-50% of AKI cases in CKD patients happen because someone didn’t stop a nephrotoxic drug in time. Dr. Matthew A. Sparks from Duke University says discontinuing these meds can prevent 30-50% of severe AKI cases. That’s not a guess. That’s data.
What Medications Should You Never Take?
Some drugs have no place in CKD patients with AKI:
- Dopamine: Once thought to protect kidneys. Now proven useless-and potentially harmful. KDIGO gives this a strong A-level recommendation against use.
- Diuretics (furosemide, hydrochlorothiazide): These don’t prevent AKI. They can make dehydration worse. Only use if you’re truly fluid overloaded.
- Fenoldopam: A kidney vasodilator. Multiple trials show zero benefit. Avoid.
And yes-this includes over-the-counter supplements. Herbal remedies like aristolochic acid (found in some traditional medicines) can cause irreversible kidney scarring. Don’t assume ‘natural’ means safe.
How Do You Know If You’re at Risk?
Most people with CKD don’t know their exact eGFR. If you haven’t had a blood test in the last 6 months, you’re flying blind. Your eGFR tells you your kidney stage:
- Stage 3: eGFR 30-59 mL/min/1.73m²
- Stage 4: eGFR 15-29 mL/min/1.73m²
- Stage 5: eGFR under 15 mL/min/1.73m²
If you’re in stage 3 or worse, you’re high-risk. That means:
- Any imaging test with contrast needs pre-approval
- All new prescriptions must be reviewed for kidney safety
- You should never take NSAIDs without explicit doctor approval
And here’s something most patients don’t realize: your creatinine level can be misleading. If you’ve lost muscle mass from illness or aging, your creatinine might look normal-even if your kidneys are failing. That’s why KDIGO recommends checking cystatin C, a more reliable marker that isn’t affected by muscle changes.
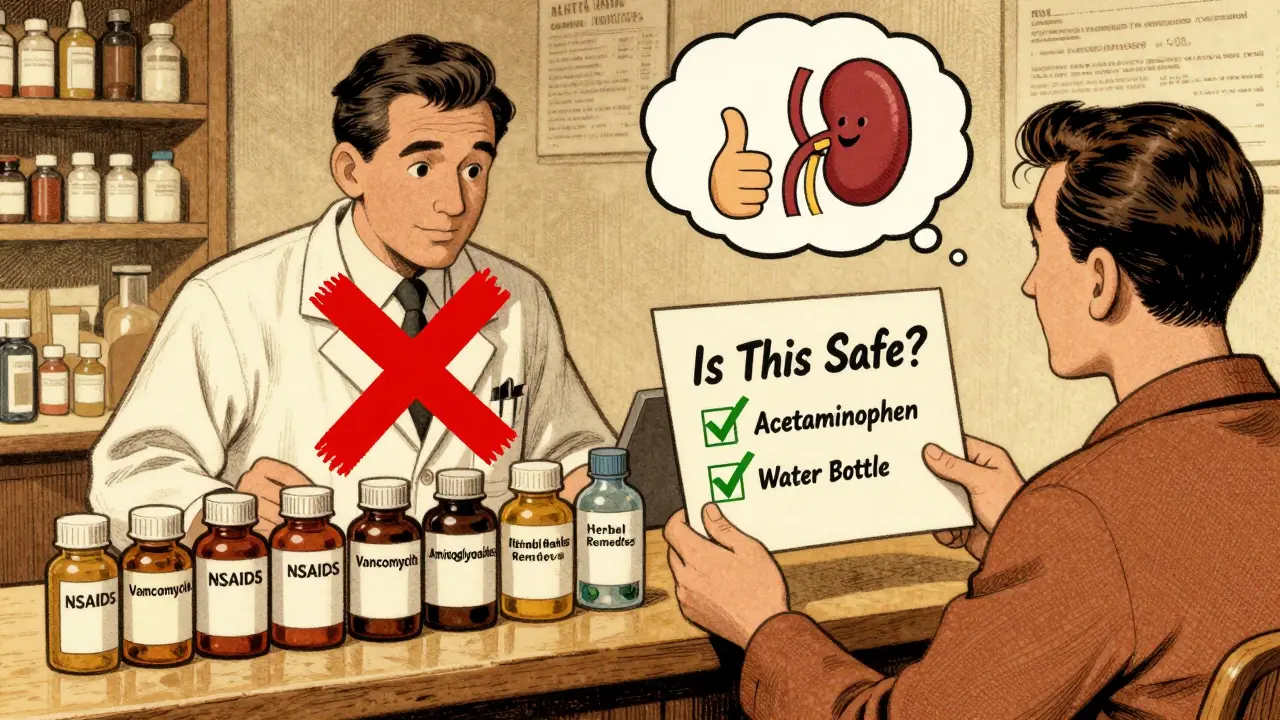
The Role of Your Pharmacist
You don’t have to be the only one watching for danger. Pharmacists are your secret weapon.
Studies show pharmacist-led reviews of medication lists reduce AKI rates in CKD patients by 22%. They spot interactions, flag high-risk drugs, and suggest safer alternatives. Ask your pharmacist to do a full med review every time you get a new prescription-even if it’s from a different doctor.
Electronic health record alerts help too. One study showed they cut inappropriate prescribing by 35%. But they’re not perfect. Doctors override them 40% of the time because they think the patient “needs” the drug. That’s why you have to speak up. If you’re on a high-risk med, ask: “Is this absolutely necessary? Is there a safer option?”
What Happens After an AKI Episode?
Recovery isn’t guaranteed. About 30% of AKI episodes in CKD patients lead to permanent loss of kidney function. 10-15% will need dialysis within five years.
If your kidneys don’t bounce back in 7 days, you may have Acute Kidney Disease (AKD)-a new term recognized since 2019. That means your kidneys are injured but not yet in full failure. It’s a warning sign. You need follow-up testing: eGFR and urine albumin-to-creatinine ratio (uACR) every 3 months.
And don’t assume you’re out of danger just because your creatinine dropped. The damage might still be there-silent, progressive. That’s why monitoring doesn’t stop after discharge.
What You Can Do Today
Here’s your action plan:
- Get your eGFR and uACR tested if you haven’t in the last 6 months.
- Make a list of every medication and supplement you take-prescription, OTC, herbal.
- Take that list to your doctor or pharmacist. Ask: “Which of these are risky for my kidneys?”
- Never take NSAIDs without explicit approval. Use acetaminophen instead for pain.
- Stay hydrated. Drink water daily. Avoid dehydration, especially if you’re sick or in hot weather.
- If you’re scheduled for a CT scan, ask: “Can we do an ultrasound or MRI instead? If not, will you hydrate me before and after?”
- Know your baseline. Write down your last eGFR number. Keep it on your phone.
Patients who get specific counseling about avoiding NSAIDs and staying hydrated have 25% fewer AKI hospitalizations. Knowledge isn’t power-it’s protection.
What’s New in 2025?
Guidelines are evolving. The KDIGO update expected in late 2024 won’t change the core advice-but it will add new tools. Biomarkers like TIMP-2 and IGFBP7 can now predict AKI within 12 hours, before creatinine even rises. That means earlier intervention.
Also, early dialysis isn’t always better. The 2022 AKIKI 2 trial showed no benefit to starting dialysis right away in severe AKI on CKD. Waiting until there are clear signs of toxicity or fluid overload is now preferred. This reduces complications and saves lives.
The message hasn’t changed: avoid the triggers. Protect your kidneys. Your next CT scan, your next antibiotic, your next pain pill-they all matter.
When to Call Your Doctor
Call immediately if you notice:
- Sudden decrease in urine output
- Swelling in legs or face
- Unexplained fatigue or confusion
- Nausea or vomiting without other cause
These aren’t normal. They’re red flags. Don’t wait for your next appointment. Act fast.




13 Comments
Wow. Just... wow. This is the kind of post that makes me want to scream at the entire medical system. People are dying because doctors don’t listen, and patients don’t know enough to demand better. I’ve seen it firsthand-my aunt was given NSAIDs for ‘a little back pain’ and ended up in dialysis. This isn’t just advice-it’s a lifeline. And if you’re still taking ibuprofen without asking your doctor? You’re playing Russian roulette with your kidneys. 😔
It is imperative to underscore, with the utmost gravity, the clinical imperative surrounding nephrotoxic pharmacological agents in the context of chronic kidney disease (CKD) with concomitant acute kidney injury (AKI). The KDIGO guidelines, as referenced, represent the current gold-standard paradigm; however, their implementation remains suboptimal due to systemic fragmentation in primary care pathways. The risk-benefit calculus must be recalibrated at the point-of-care, particularly with regard to iodinated contrast media and non-steroidal anti-inflammatory drugs (NSAIDs), which, in aggregate, account for approximately 47% of iatrogenic AKI episodes in this cohort. Prophylactic hydration with isotonic saline remains the only evidence-based, cost-effective intervention with Level A recommendation.
you dont need to be a doctor to save your kidneys. just stop the ibuprofen. drink water. ask your pharmacist. thats it. i had stage 3 ckd and i did nothing fancy-just stopped the painkillers and started reading labels. my creatinine dropped. no magic. just common sense. 🤷♀️
Ugh, I’m so tired of this ‘avoid contrast’ nonsense. We’re in America-why are we letting fear stop us from getting the scans we need? My uncle had a CT and lived to 85. If you’re scared of medicine, maybe don’t live here. We’ve got the best healthcare in the world, and people are too lazy to trust it.
i read this and i cried. my mom has ckd and she’s always taking pain meds because she doesn’t know they’re dangerous. thank you for writing this like you actually care. i’m printing this out and taking it to her next appointment. she’s gonna be okay because of posts like this. 💛
OMG I just realized I’ve been taking Advil for my headaches for 3 years 😱 I’m going to the pharmacy right now to ask if they can check my kidney numbers. Also-hydration is everything. I’m drinking 3L of water today. 💪💧 #KidneyAwareness
There is merit in the assertion that pharmacists represent an underutilized frontline resource in the prevention of iatrogenic AKI. Their role in medication reconciliation and flagging nephrotoxic agents-particularly in polypharmacy patients-is empirically supported. The 22% reduction in AKI incidence via pharmacist-led review is not statistically insignificant. Systemic integration of pharmacy services into routine CKD management protocols should be prioritized.
I’m not a doctor, but I’ve been on dialysis for 8 years. I didn’t know any of this until after I lost 70% of my kidney function. I wish someone had told me NSAIDs were dangerous. I thought they were just like Tylenol. Please-don’t wait until it’s too late. This information matters.
This is beautifully written. I’m from India, and here, people take NSAIDs like candy-no prescription, no thought. I’ve seen friends with diabetes and high BP ruin their kidneys because they didn’t know. I’m sharing this with my family and my community group. Knowledge should not be a privilege.
my cousin died last year from ak on ckd. he was 42. he took ibuprofen for his back and thought it was fine. no one told him. this post is so important. thank you.
Wow. A 2000-word lecture on avoiding Tylenol and water. Groundbreaking. Next up: ‘How to Avoid Breathing: A Guide to Preventing Oxygen Toxicity.’
Why are we letting foreigners tell us how to do medicine? In America, we don’t fear scans. We don’t fear meds. We fix things. This post reads like a WHO pamphlet translated by someone who hates innovation. If your kidneys are weak, maybe you shouldn’t be living in a country with processed food and pollution. Blame the system, not the drugs.
Let me just say-this post is a goddamn masterpiece. I was a nurse for 18 years. I’ve watched people die because they took a Motrin for a headache. I’ve seen doctors shrug and say, ‘It’s just one pill.’ ONE PILL. And then they’re on dialysis at 52. This isn’t just medical advice-it’s a war cry. Print this. Frame it. Tape it to your fridge. Your kidneys are screaming. Are you listening?
Write a comment