Antipsychotic Symptom & Side Effect Match Tool
How Can We Help You?
This tool helps you compare Solian (amisulpride) with other antipsychotics based on your specific symptoms and side effect concerns.
Symptom Concerns
Side Effect Concerns
Your Medication Match
Based on your selections, we've matched the best options for your symptoms and concerns.
Solian (Amisulpride)
Risperidone
Olanzapine
Quetiapine
Aripiprazole
Paliperidone
Important: This tool is for informational purposes only. Always consult with your psychiatrist before making any changes to your medication. Individual responses to medications vary significantly.
When someone is prescribed Solian (amisulpride), they’re often facing serious mental health challenges-like schizophrenia, severe depression with psychotic features, or persistent negative symptoms that other meds haven’t touched. But finding the right treatment isn’t just about taking what’s given. Many people wonder: Amisulpride might help, but are there better or safer options? This isn’t about switching meds on a whim. It’s about understanding how it stacks up against the competition-what it does well, where it falls short, and what else you might try if it’s not working.
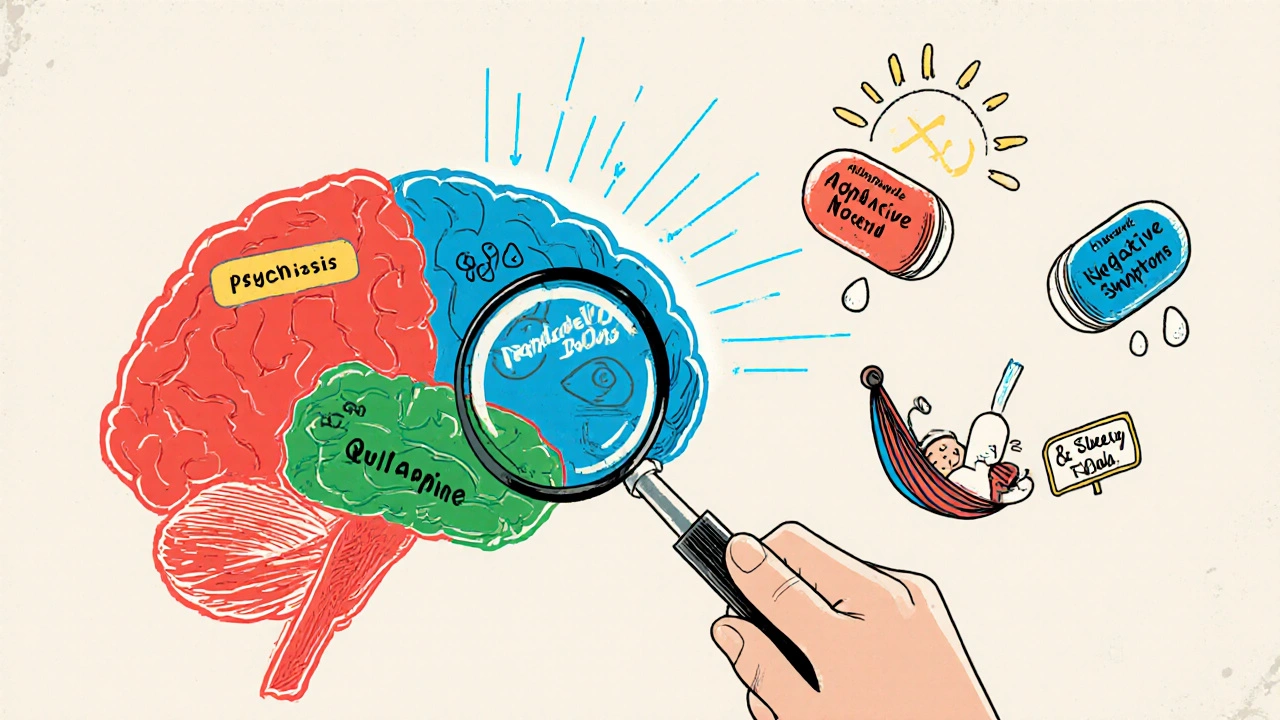
What Solian (Amisulpride) Actually Does
Amisulpride is an atypical antipsychotic, meaning it works differently than older drugs like haloperidol. It mainly targets dopamine D2 and D3 receptors in the brain, but with a twist: at low doses (50-300 mg/day), it boosts dopamine in areas linked to mood and motivation. At higher doses (400-1200 mg/day), it blocks dopamine where it’s overactive-like in the mesolimbic pathway, which helps reduce hallucinations and delusions.
This dual action makes it unique. For people with schizophrenia who struggle with apathy, social withdrawal, or lack of emotion (negative symptoms), low-dose amisulpride often works better than other antipsychotics. In a 2023 meta-analysis of 12 randomized trials, amisulpride showed significantly better improvement in negative symptoms compared to risperidone and olanzapine. It’s also one of the few antipsychotics with FDA-approved use for acute depressive episodes in major depressive disorder, especially when psychosis is involved.
But it’s not magic. Side effects happen. Weight gain? Less than olanzapine, but still possible. Sedation? Mild. But the big one: elevated prolactin levels. That can mean breast enlargement, milk production, missed periods, or low libido. For some, this is a dealbreaker.
How It Compares to Risperidone
Risperidone is one of the most commonly prescribed antipsychotics worldwide. It’s effective for both positive and negative symptoms, and it’s available as a long-acting injection-something amisulpride isn’t. That makes risperidone easier for people who struggle with daily pills.
But here’s the catch: risperidone causes more movement disorders-tremors, stiffness, restlessness-than amisulpride. In a 2022 head-to-head trial of 312 patients with schizophrenia, 28% of those on risperidone developed akathisia (inner restlessness), compared to just 9% on amisulpride. That’s a big difference for daily life.
On the other hand, risperidone has less impact on prolactin than amisulpride. If you’re worried about sexual side effects or hormonal changes, risperidone might be gentler. But if your main issue is emotional flatness or lack of drive, amisulpride often wins.
Olanzapine: The Weight Gain Giant
Olanzapine is powerful. It works fast and helps with mood, psychosis, and even anxiety. But it’s also notorious for weight gain. In clinical trials, patients on olanzapine gained an average of 4.5 kg (10 lbs) in 6 weeks. Some gained over 15 kg. That increases risk for diabetes, high cholesterol, and heart disease.
Amisulpride? Much lighter. In the same studies, average weight gain was under 1.5 kg. For someone already struggling with metabolic health, that matters. Amisulpride also causes less sedation than olanzapine, so people can stay more alert during the day.
But olanzapine has one edge: it’s often better for severe agitation and aggression. If someone is in crisis-yelling, violent, disoriented-olanzapine may calm them faster. Amisulpride takes longer to kick in. It’s not a rescue drug.
Quetiapine: The Sleepy Alternative
Quetiapine is everywhere-not just for psychosis, but for insomnia, anxiety, and bipolar depression. It’s a sedative first, an antipsychotic second. That’s why doctors sometimes prescribe it off-label for sleep issues.
Compared to amisulpride, quetiapine causes way more drowsiness. People on quetiapine often report being too tired to work or drive. It also increases blood sugar and cholesterol more than amisulpride. But if you’re struggling with insomnia or severe anxiety alongside psychosis, quetiapine’s calming effect can feel like a lifeline.
Amisulpride doesn’t make you sleepy. That’s good if you need to stay functional. But if your brain won’t shut off at night, amisulpride won’t help you sleep. You’d need something else.

Aripiprazole: The Balanced Option
Aripiprazole works differently than the others. Instead of just blocking dopamine, it partially activates dopamine receptors-kind of like a dimmer switch. That’s why it’s often called a “dopamine stabilizer.”
It’s less likely to cause weight gain, high prolactin, or sedation. For people who had bad side effects with other antipsychotics, aripiprazole is often the go-to alternative. It’s also available as a monthly injection.
But here’s the downside: it’s weaker for negative symptoms. If your main problem is not caring about anything, not talking to people, or losing interest in life, aripiprazole might not help much. Amisulpride does better there. Also, aripiprazole can cause agitation or anxiety in some people-something amisulpride rarely does.
Paliperidone: The Long-Acting Cousin
Paliperidone is the active metabolite of risperidone. It’s available as a once-monthly injection (Invega Sustenna), which makes it perfect for people who miss doses or don’t trust their memory.
Its side effect profile is similar to risperidone: moderate weight gain, some movement issues, and a moderate rise in prolactin-less than amisulpride but more than aripiprazole.
If adherence is your biggest challenge, paliperidone is a strong contender. But if you’re trying to fix emotional numbness or social withdrawal, amisulpride still has the upper hand. Plus, paliperidone doesn’t have the same evidence for treating depressive episodes in major depression.
When Amisulpride Might Not Be Right
Amisulpride isn’t for everyone. Avoid it if you:
- Have a history of prolonged QT interval or heart rhythm problems
- Are pregnant or breastfeeding (data is limited)
- Have severe liver disease
- Are already taking other drugs that raise prolactin (like some antidepressants)
Also, don’t try to self-adjust the dose. Low dose = mood booster. High dose = psychosis blocker. Mixing them up can make things worse.
What to Do If Amisulpride Isn’t Working
If after 6-8 weeks you’re still hearing voices, feeling empty, or can’t get out of bed, talk to your doctor. Don’t quit cold turkey. Stopping suddenly can cause rebound psychosis or severe withdrawal.
Options include:
- Switching to aripiprazole if side effects are the issue
- Trying paliperidone injection if you forget pills
- Adding a low-dose antidepressant if depression dominates
- Trying clozapine (last-resort) if nothing else works-though it needs weekly blood tests
Some people benefit from combining meds. For example, low-dose amisulpride + a low-dose SSRI like sertraline can help both psychosis and depression. But this needs careful monitoring.
Real-World Choices
Imagine two people:
- Person A: 32, diagnosed with schizophrenia. Feels emotionally flat, doesn’t talk to friends, can’t get motivated. Lost 8 lbs in 3 months. No weight gain, no movement issues. Amisulpride 300 mg/day improved their energy and interest in life within 6 weeks. Prolactin rose, but they’re okay with it.
- Person B: 45, with depression and hallucinations. Struggles with sleep, gained 12 lbs on olanzapine. Blood sugar up. Switched to amisulpride 400 mg/day. Hallucinations gone. No weight gain. Still tired, but not sleepy. Now they’re working part-time.
Neither would’ve done as well on quetiapine or aripiprazole. That’s the point: there’s no universal best drug. It’s about matching the drug to your symptoms and your body.
Final Thoughts
Amisulpride isn’t the first-line drug in every country, but it’s one of the most targeted treatments for negative symptoms and treatment-resistant depression with psychotic features. If you’re stuck with apathy, emotional numbness, or lack of drive-and other antipsychotics haven’t helped-it’s worth serious consideration.
But if you’re worried about prolactin, need a long-acting shot, or struggle with sleep, alternatives like aripiprazole, paliperidone, or even quetiapine might fit better.
The key? Track your symptoms. Keep a journal: mood, sleep, energy, side effects. Bring it to your doctor. Don’t just accept the first prescription. Your brain deserves a tailored plan-not a one-size-fits-all pill.
Is Solian (amisulpride) better than risperidone for negative symptoms of schizophrenia?
Yes, studies show amisulpride is more effective than risperidone for improving negative symptoms like emotional flatness, social withdrawal, and lack of motivation. Risperidone works well for hallucinations and delusions but often doesn’t help with these deeper, persistent symptoms. Amisulpride’s unique action on dopamine receptors in the brain’s mood centers gives it an edge here.
Does amisulpride cause weight gain like olanzapine?
No, amisulpride causes significantly less weight gain than olanzapine. In clinical trials, patients on olanzapine gained an average of 4.5 kg in 6 weeks, while those on amisulpride gained less than 1.5 kg. This makes amisulpride a better choice for people with metabolic concerns like prediabetes or high cholesterol.
Can I take amisulpride if I have heart problems?
Amisulpride can prolong the QT interval on an ECG, which may increase the risk of dangerous heart rhythms. If you have a history of long QT syndrome, heart failure, or are taking other drugs that affect heart rhythm (like certain antibiotics or antidepressants), amisulpride may not be safe. Always get an ECG before starting and monitor it regularly.
Why does amisulpride raise prolactin levels?
Amisulpride blocks dopamine receptors in the pituitary gland, where dopamine normally suppresses prolactin production. When dopamine is blocked, prolactin rises. This can lead to breast enlargement, milk production, missed periods, or low libido. It’s a known side effect, not a mistake. If it’s troubling, alternatives like aripiprazole or quetiapine have less impact on prolactin.
Is amisulpride used for depression without psychosis?
In some countries, low-dose amisulpride (50-100 mg/day) is approved for major depressive disorder-even without psychotic features. Studies show it can improve energy, motivation, and mood in treatment-resistant depression. It’s not first-line, but it’s an option when SSRIs and SNRIs fail. Always use under medical supervision.
How long does it take for amisulpride to start working?
For negative symptoms or depression, improvement may take 2-4 weeks. For psychosis, it can take 4-6 weeks to reach full effect. Unlike some antipsychotics that act quickly on agitation, amisulpride works gradually. Don’t give up too soon-stick with it for at least 6 weeks before deciding it’s not working.
Can I switch from olanzapine to amisulpride safely?
Yes, but not abruptly. Taper olanzapine slowly over 1-2 weeks while starting amisulpride at a low dose. This prevents withdrawal symptoms or rebound psychosis. Monitor for changes in mood, sleep, and movement. Many people switch successfully, especially if weight gain or metabolic issues were problems with olanzapine.
If you’re considering a switch or wondering why your current treatment isn’t working, talk to your psychiatrist. Bring your symptom journal. Ask about prolactin levels, weight trends, and energy changes. There’s no single best drug-only the best fit for you.





9 Comments
Man, I’ve been on amisulpride for almost a year now, and honestly? It’s the first thing that didn’t make me feel like a zombie. I used to just stare at the wall for hours, couldn’t even text my mom. Low dose (200mg) totally flipped a switch-suddenly I wanted to cook, walk outside, even rewatch my favorite shows without feeling guilty. Yeah, prolactin spiked-I got some weird breast tenderness-but my doctor monitored it, and we just adjusted. If you’re stuck in emotional numbness, don’t give up too soon. It’s slow, but it’s real.
How quaint. You’re all acting like amisulpride is some miraculous elixir, when in reality, it’s just another dopamine antagonist with a fancy marketing campaign. The ‘negative symptom’ narrative is largely a pharmaceutical fabrication-designed to push drugs onto patients who’ve already been failed by SSRIs. And prolactin elevation? That’s not a ‘side effect,’ it’s a physiological red flag. Anyone prescribing this without rigorous endocrine monitoring is practicing dangerous, outdated medicine. Aripiprazole, at least, respects the hypothalamic-pituitary axis.
There’s something deeply human about how this drug works-not by drowning out the noise, but by gently turning up the volume on the parts of you that got silenced. I used to think depression was just sadness. But this? This is the quiet erosion of being. Amisulpride doesn’t cheer you up. It doesn’t make you happy. It just lets you feel again. Even the pain. Even the emptiness. And somehow, that’s the first step back. I’ve seen people come back from the edge with this. Not because it’s perfect. But because it doesn’t erase them. It lets them be. And that’s rarer than you think.
Just a quick note: if you’re switching from olanzapine, do NOT go cold turkey-seriously, don’t. I did it once, and I had a 72-hour panic spiral that felt like my brain was rewiring itself in reverse. Taper slowly, like over 10–14 days. Start amisulpride at 50mg, even if your doc says 100. Give your body time. Also-get a baseline prolactin test before you start. And track your sleep, energy, and cravings. I kept a spreadsheet. It saved me.
Stop romanticizing this drug. It’s not magic. It’s chemistry. And if you’re not getting regular ECGs because you’re ‘afraid’ of the hospital, you’re playing Russian roulette with your heart. Also, prolactin isn’t ‘just a side effect’-it’s endocrine disruption. Women, you’re getting bone density loss. Men, you’re getting gynecomastia. Stop pretending this is some gentle, soulful fix. It’s a powerful neuroactive compound with serious trade-offs. If you’re not monitoring, you’re not treating-you’re gambling.
I’ve been on aripiprazole for two years, and while it’s clean-no weight gain, no prolactin issues-I still feel like I’m watching my life through foggy glass. My partner says I smile less. My therapist says I’m ‘detached.’ I tried amisulpride for six weeks on a trial basis. It didn’t kill my libido. It didn’t make me fat. But it did something quieter: it made me care again. About the plants on my windowsill. About whether my dog liked his new bed. I didn’t cry. I didn’t laugh. I just… noticed things. And that was enough to keep going. I’m not saying it’s better. Just different. And sometimes, different is all you need.
Hey-I’ve been there. Lost 15 pounds. Couldn’t get out of bed. Tried everything. Amisulpride at 100mg changed my life. Not because it fixed everything. But because it gave me back the space to try. I started journaling. Took walks. Called my sister. It didn’t fix my trauma. But it let me face it. If you’re scared of side effects? Talk to your doctor. Get blood work. But don’t let fear stop you from trying something that might actually help. You’re worth the effort.
You know what’s worse than the drug? The silence. The way people look at you when you say you’re on an antipsychotic. Like you’re broken. Like you’re not human anymore. Amisulpride didn’t cure me. But it gave me back my voice. I started writing poetry again. I told my mom I loved her. I cried in the shower. No one talks about this. The quiet victories. The moments when you choose to live, even when your brain tells you not to. This isn’t just medicine. It’s a lifeline. And if you’re afraid of prolactin? Then be afraid of dying alone in silence instead.
Just want to say-don’t compare yourself to Person A or Person B in the article. Everyone’s different. I’m on 400mg, had zero weight gain, prolactin’s elevated but I’m okay with it. I’m working full-time. I’m dating again. I still have bad days. But now I have tools. If you’re reading this and you’re scared? You’re not alone. Talk to someone. Even if it’s a Reddit stranger. We’ve all been there.
Write a comment