Opioid Itching Treatment Calculator
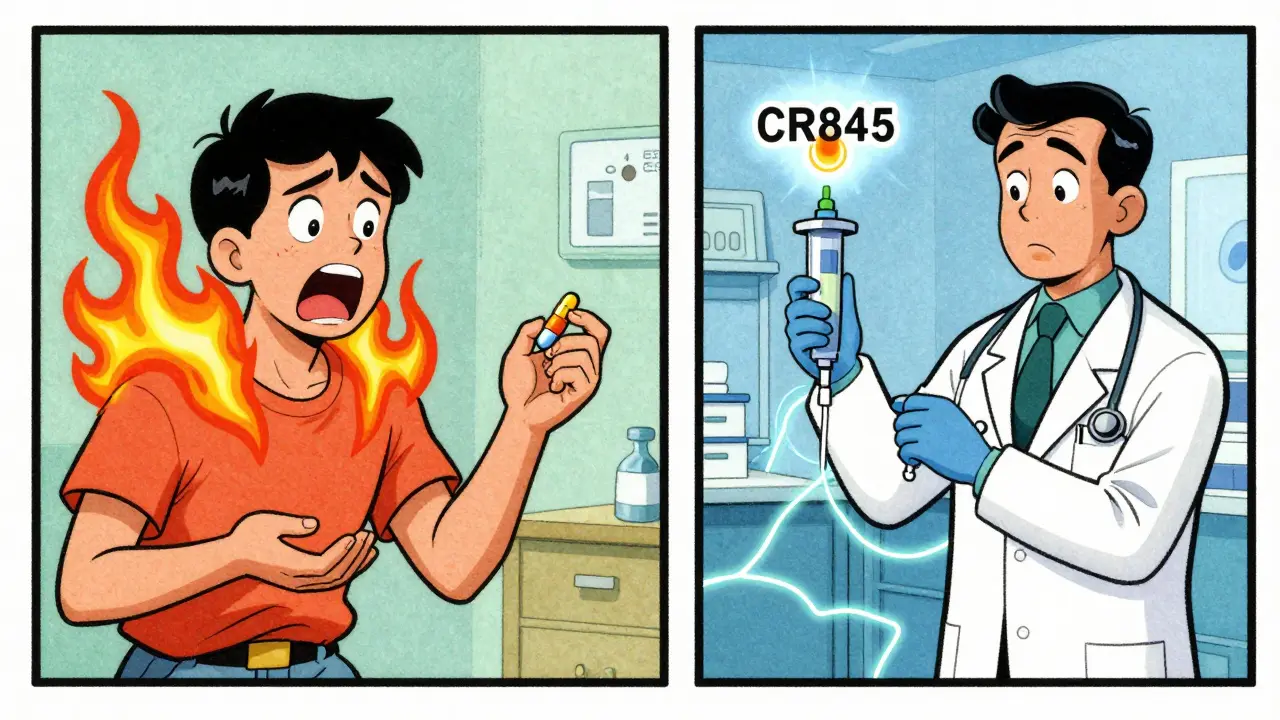
Select a treatment option and enter patient weight to calculate the appropriate dosage for opioid-induced itching. This tool is based on clinical evidence showing that traditional antihistamines are ineffective for most cases.
Recommended Treatment
Enter patient weight and select a treatment to see dosage recommendations
Important: This calculation is for clinical guidance only. Always consult current medical guidelines and patient-specific factors. Treatments must be administered within 5-10 minutes of itching onset for maximum effectiveness.
Think opioids only block pain? Think again. For many people, especially after surgery or childbirth, opioids bring a relentless, maddening side effect: itching. Not just a little tickle - full-body, face-scraping, sleep-destroying itch that makes you want to tear your skin off. It’s not an allergy. It’s not dry skin. It’s opioid-induced pruritus, and it’s more common than most doctors admit.
Why Do Opioids Make You Itch?
For decades, doctors blamed histamine. The idea was simple: opioids like morphine and codeine trigger mast cells in your skin to dump histamine, just like an allergic reaction. That’s why diphenhydramine (Benadryl) became the go-to fix. But here’s the problem - it doesn’t work well. Only 20-30% of patients get relief. That’s because histamine isn’t the main culprit.
Modern research shows opioid-induced itching comes from two places: your nerves and your spinal cord. When you take morphine, it binds to mu opioid receptors (MOR) - the same ones that stop pain. But in certain nerve cells, especially those with TRPV1 proteins, that same binding turns on itch signals. These nerves run from your spinal cord up to your skin, especially in your face, chest, and arms. That’s why the itching hits there first.
Studies using selective MOR agonists like DAMGO proved this. When injected under the skin, they caused itching - and naloxone, a drug that blocks opioid receptors, stopped it. Even more telling: when researchers destroyed those TRPV1 nerves with resiniferatoxin, the itching vanished. No histamine involved. This isn’t an allergic reaction. It’s a direct neural hijack.
How Common Is It?
It’s not rare. It’s routine. If you get morphine through your spine (intrathecal), like during a C-section, there’s a 70-100% chance you’ll itch. IV morphine? 30-50%. Oral opioids? Lower, around 10-30%. Why the difference? It’s about where the drug hits first. Spinal delivery means opioids act directly on nerve centers that control itch. Oral opioids get broken down in the liver first, so less reaches those critical spots.
Real-world stories back this up. In postpartum forums, 78% of mothers said itching kept them from bonding with their newborns. One woman wrote: ‘I couldn’t hold my baby because I was scratching my face raw.’ On Reddit, 89 out of 147 people described uncontrollable itching within minutes of IV morphine. Nurses report the same thing - itching starts fast, hits hard, and doesn’t care if you’re in pain or not.
Why Antihistamines Fail
Diphenhydramine and cetirizine are still used - but they’re outdated tools. They block histamine receptors, but if histamine isn’t driving the itch, they’re useless. Clinical trials show they help only a fraction of patients. Worse, they cause drowsiness. One nurse practitioner on AllNurses said: ‘Nalbuphine works in 5 minutes. Benadryl makes patients sleep for 45 - and they still itch.’
There’s also confusion between itching and true allergic reactions. In 32% of cases, doctors mistake opioid itching for anaphylaxis and give epinephrine unnecessarily. That’s dangerous. True allergic reactions come with swelling, low blood pressure, or breathing trouble. Opioid itching? Just the itch. No hives. No wheezing. Just that burning, crawling feeling.
What Actually Works
Forget antihistamines. The real solutions target the opioid system itself.
- Naloxone - given at 0.25 mcg/kg/min as a slow drip, it blocks opioid receptors just enough to stop itching without touching pain relief. Studies show 60-80% reduction in itching. Hospitals like the University of Copenhagen use this as standard.
- Nalbuphine - this drug is a mixed agent. It blocks mu receptors (which cause itching) but activates kappa receptors (which suppress itch). At 5-10 mg IV, it cuts itching by 85%. It’s fast - works in under 5 minutes. And it doesn’t wake patients up like Benadryl does.
- Butorphanol - another kappa agonist. In C-section patients, it dropped itching scores from 8.2 to 2.1 on a 10-point scale.
- Naltrexone - 1.2 mg IV gives 75% relief. Used less often because it’s stronger and can blunt pain if overdosed.
- Lidocaine (IV) - 1.5 mg/kg reduces itching by 70%. But it needs cardiac monitoring. Not first-line, but useful when other options fail.
The key? Timing. Give these drugs within 5-10 minutes of itching starting. Wait too long, and the nerve signals lock in. It’s harder to stop.
The New Frontier: Kappa Agonists
The future is here. CR845 (difelikefalin), a peripherally restricted kappa agonist, just finished Phase II trials. It reduces itching by 65% - without crossing the blood-brain barrier. That means no drowsiness, no pain relief loss, no risk of addiction. It’s targeted, safe, and designed specifically for this problem.
By 2028, experts predict 75% of major hospitals will use mu antagonist/kappa agonist combos as standard. That’s the shift: from treating symptoms to fixing the broken signal.
What Patients Say
Behind the stats are real people. In chronic pain forums, 22% say they quit opioids because of the itching. One user wrote: ‘I’d rather have pain than feel like fire ants are crawling under my skin 24/7.’
This isn’t just discomfort. It’s a barrier to recovery. New moms can’t sleep. Surgery patients can’t rest. People on long-term opioids stop taking them - not because the pain returned, but because the itch became unbearable.
What Hospitals Are Doing Right
Some places have fixed this. The American Society of Anesthesiologists released a toolkit in 2022 with dosing calculators for naloxone infusions. It shows how to reduce itching by 75% while keeping pain control at 90%. Hospitals that use it see 40% fewer rescue meds.
But adoption is slow. Only 37% of U.S. hospitals have formal protocols. Academic centers? 68%. Obstetrics units? They’re ahead - they see it every day. Orthopedics? Not so much.
The European Pain Federation now recommends checking for itching risk in every patient getting spinal opioids. That’s progress.
Final Takeaway
Opioid-induced itching isn’t a minor side effect. It’s a neurological glitch. Histamine plays a role in some cases - especially with hives - but for most people, it’s the nerves. Antihistamines are outdated. The real fix is smarter drug use: nalbuphine, naloxone, or newer kappa agonists. If you’re on opioids and itching, speak up. Ask for nalbuphine. Don’t settle for Benadryl. Your sleep, your recovery, and your peace of mind matter more than you think.





14 Comments
I had this after my C-section. Thought I was going crazy. Scratched my face raw trying to sleep. No one told me this was normal. I just felt like a broken person.
THIS. 😭 I was on morphine after my appendectomy and I swear I could feel ants crawling under my skin. Benadryl did NOTHING. I was so relieved to find this post. Thank you for validating what felt like madness.
Of course it's not histamine. We're talking about Americans who think Advil is a cure-all and still drink soda for 'energy.' No wonder doctors are clueless. In Russia, they used to just give you a shot of vodka and tell you to shut up. Works better than Benadryl anyway.
Ah yes, the grand tragedy of modern medicine: we’ve replaced suffering with suffering. First, the opioid that numbs your pain - then the same opioid makes you beg for pain. It’s poetic. Like a god who gives you a rose, then sets it on fire to see if you’ll still kneel. 🌹🔥
Okay but like… why is everyone still using morphine? It’s 2025. We have fentanyl patches, tapentadol, even non-opioid combos. And we’re still stuck on this 19th-century relic that makes you itch like a demon? 😒
I remember my sister screaming in the recovery room after her surgery. She kept saying, ‘It’s like my nerves are on fire.’ We all thought it was anxiety. Turns out? She just needed nalbuphine. No one asked. No one knew. This post? Lifesaver.
My nurse gave me Benadryl and I fell asleep for 3 hours. Woke up still itching. Felt like a zombie who got scalded. I asked for something else and they gave me naloxone drip. Instant relief. Why isn’t this standard??
Good post. I’ve seen this a lot in post-op units. Nurses know what to do but docs don’t always listen. We need better training. Simple as that.
You’re not alone. If you’re itching after opioids, don’t suffer in silence. Ask for nalbuphine. It’s not hard. Just say ‘I need the itch drug, not the sleepy pill.’ You got this.
It’s fascinating how the body hijacks its own systems. Pain and itch share pathways. One is survival. The other? Just… noise. But the brain doesn’t know the difference. We’re wired to respond to both. Maybe that’s why it feels so urgent. 🤯
Wow. So you’re telling me people are still giving Benadryl? Like, in 2025? That’s not ignorance, that’s malpractice. If your doctor doesn’t know about nalbuphine or naloxone infusions, fire them. Seriously.
wait so benadryl dont work?? i thought it was just me being weak… i thought i was just allergic… i cried so much after my surgery
Let me be clear: this isn’t a ‘minor side effect.’ It’s a systemic failure. Hospitals are still using 1950s protocols because they’re cheap and easy. But the science is here: kappa agonists, targeted naloxone drips, even lidocaine infusions. We’re not talking about ‘experimental’ stuff - we’re talking about proven, published, peer-reviewed solutions. Why aren’t they standard? Because change is hard. Because someone’s got to do the work. And too many hospitals still think ‘it’s just itching.’ It’s not. It’s a neurological emergency disguised as annoyance. If you’re a clinician reading this: stop treating the symptom. Treat the circuit. If you’re a patient: demand nalbuphine. Don’t let them gaslight you with Benadryl. You deserve to rest. You deserve to heal. And you deserve to not feel like your skin is trying to escape your body.
Of course it’s not histamine. Only someone who thinks ‘allergies’ are the root of all medical problems would still believe that. Honestly, if your doctor still prescribes Benadryl for this, they’re practicing medicine like it’s 1998. I’m not even mad - I’m just disappointed. 🙄
Write a comment