Googling Trileptal at 2am usually means one thing: you need straight answers-what it does, how to take it, what to watch for, and how it fits with life (school run, work, sleep). Here’s the plain-English guide I wish every GP had time to give: clear, UK-focused, and honest about trade-offs. Expect practical steps, not abstract jargon.
- TL;DR: Trileptal (oxcarbazepine) treats focal (partial) seizures in adults and children; it’s also used off‑label for trigeminal neuralgia and sometimes bipolar. It’s not a cure; it’s a tool to reduce seizure frequency and severity.
- Start low, go slow: typical adult start is 300 mg twice daily, titrating to 600-1200 mg twice daily. Kids use weight‑based dosing. Don’t stop suddenly.
- Common side effects: sleepiness, dizziness, nausea, double vision. Important risks: low sodium (hyponatraemia), serious skin rash (rare), allergy (especially if carbamazepine caused one).
- Interactions: reduces effectiveness of many hormonal contraceptives; can raise phenytoin; extra risk of low sodium with SSRIs/diuretics. Alcohol boosts drowsiness.
- UK specifics: follow DVLA rules for driving with epilepsy. If pregnancy is possible, plan contraception carefully and use high‑dose folic acid if trying to conceive.
What Trileptal (oxcarbazepine) is-and who it’s for
Trileptal is the brand name for oxcarbazepine, an anti‑seizure medicine. In the UK, you’re most likely to receive generic oxcarbazepine. It stabilises overactive brain electrical activity to reduce focal (partial) seizures, with or without secondary generalisation. NICE (epilepsies guideline NG217, updated 2024) lists oxcarbazepine among first‑line options for focal epilepsy in adults and children, depending on individual factors like sex, comorbidities, and potential pregnancy.
What it’s licensed for (UK): focal seizures as monotherapy or add‑on therapy in adults and children. What it’s often used for off‑label: trigeminal neuralgia when carbamazepine isn’t tolerated, and sometimes bipolar disorder (evidence is mixed; not a UK licence). If a consultant has suggested it for pain or mood, it’s because its mechanism overlaps with carbamazepine but with a somewhat different side‑effect profile.
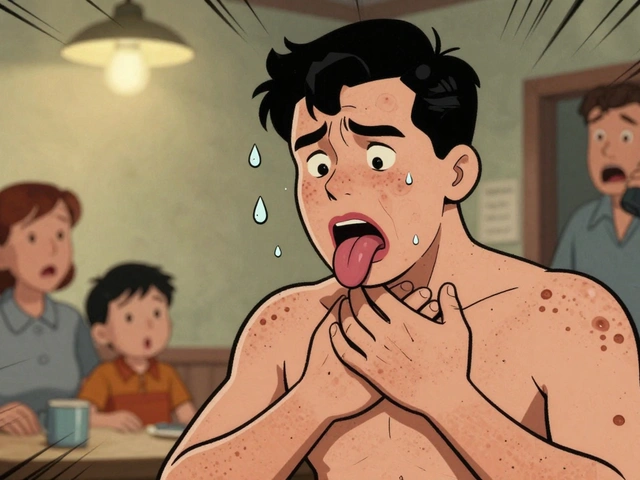
How it feels: many people notice a few days of wooziness when starting or increasing the dose-dizziness, sleepiness, mild nausea, and visual blur are common. These usually settle as your brain adapts. If they don’t, call your prescriber; small dose changes often help.
Who might benefit: people with focal seizures who haven’t done well with levetiracetam (mood issues) or carbamazepine (drug interactions, rash, or hyponatraemia). Oxcarbazepine is less prone than carbamazepine to certain enzyme interactions, but it still lowers hormonal contraceptive efficacy and can cause low sodium.
Who should be cautious: anyone with a prior serious rash to carbamazepine (there’s cross‑reactivity), older adults (higher hyponatraemia risk), those on SSRIs or diuretics, and people of Han Chinese, Thai, or other high‑risk Asian ancestry (screening for HLA‑B*1502 is often advised because of the rare but serious rash risk). These points are reflected in the BNF (September 2025), the Trileptal product information, and MHRA advice.
How to take it safely: dosing, titration, and everyday routines
Good treatment is boringly consistent: same times every day, slow titration, and no abrupt stops. Here’s the practical version you can live with.
Typical adult dosing:
- Start: 300 mg twice daily.
- Increase: by 300 mg/day every 3-7 days, as tolerated.
- Usual range: 600-1200 mg twice daily (1200-2400 mg/day). Max 2400 mg/day.
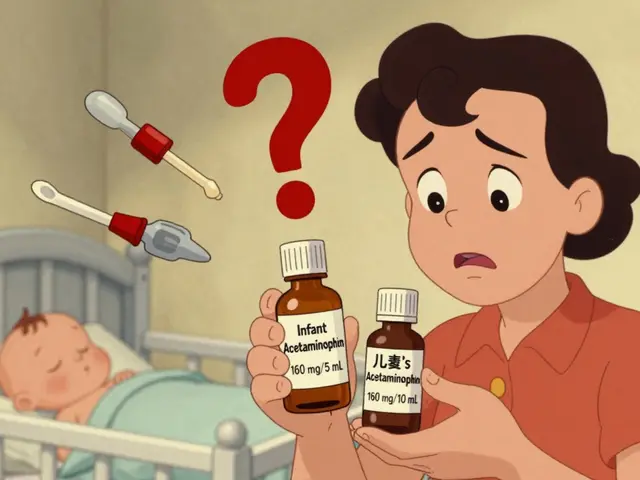
Paediatric dosing (common approach; your specialist will tailor):
- Start: ~8-10 mg/kg/day divided twice daily.
- Target: up to ~30-46 mg/kg/day (usually capped at adult max).
- Liquid: 60 mg/mL suspension helps for smaller bodies and fine‑tuning.
Table-quick reference on forms, dosing, and watch‑outs:
| Item | Details |
|---|---|
| Active drug | Oxcarbazepine; main active metabolite is MHD |
| Forms | Tablets: 150 mg, 300 mg, 600 mg; Oral suspension: 60 mg/mL |
| Adult start | 300 mg twice daily |
| Adult maintenance | 600-1200 mg twice daily (max 2400 mg/day) |
| Child start | ~8-10 mg/kg/day in 2 doses |
| Child target | Up to ~30-46 mg/kg/day (specialist sets cap) |
| Onset | Days to weeks; full effect after titration |
| Stop/withdraw | Never suddenly; taper over weeks under medical advice |
| Key labs | Sodium (baseline and during titration or if symptomatic) |
| Major cautions | Hyponatraemia, severe rash, hypersensitivity |
| Contraception | Reduces effectiveness of many hormonal methods |
| Driving (UK) | Follow DVLA epilepsy rules; avoid driving until you know your response |
How to build the habit (actual life, not perfect life):
- Pair doses with anchors you never skip: teeth brushing and the evening kettle. I keep a sticky note by the tea caddy because mornings with Elowen and Caius are… lively.
- Use a weekly pill organiser. It’s a tiny cost for a huge reduction in missed doses.
- If you miss a dose and it’s within 6 hours, take it. If it’s close to the next one, skip and carry on. Don’t double up unless your prescriber told you to.
- Alcohol: a small drink may be fine, but it adds to drowsiness and balance issues-test on a quiet night in, not at a party.
Switching from another anti‑seizure med: this is a cross‑taper over weeks. Your prescriber will raise oxcarbazepine to a therapeutic dose before lowering the old one. Stopping abruptly can trigger seizures (including status epilepticus). This cross‑taper approach mirrors BNF and NICE practice.
Monitoring plan worth agreeing in advance:
- Baseline sodium (Na+), repeat 2-4 weeks after starting or dose increases, then if symptomatic (headache, confusion, worse seizures, nausea, falls).
- Consider sodium checks more often if you’re over 60, or on SSRIs, thiazide diuretics, or have kidney issues.
- Skin check and low threshold to seek help for rashes in the first 2 months.
Side effects you might feel vs red flags you can’t ignore
Most people experience something at the start; most side effects ease as your body adjusts. Here’s the split between “annoying but common” and “stop and call” territory, with the why behind each.
Common, usually short‑lived:
- Drowsiness, dizziness, fatigue-dose‑related; go slower on titration, and split doses 12 hours apart.
- Nausea, vomiting-try with food; ginger tea helps some.
- Blurred or double vision-dose‑related; check you’re not increasing too fast.
- Headache-often early on; watch for low sodium symptoms (see below) if persistent.
Important risks (call for advice urgently; emergency care if severe):
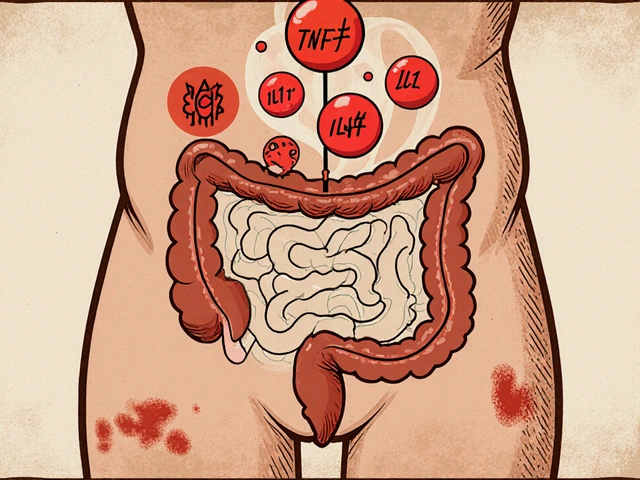
- Hyponatraemia (low sodium). Signs: increasing tiredness, confusion, nausea, headache, unsteadiness, cramps, seizures. Risk rises with age, higher doses, SSRIs, and diuretics. Clinically significant low sodium occurs in a minority but isn’t rare. The product info and BNF highlight this; monitoring helps catch it early.
- Serious skin reactions (rare): Stevens-Johnson syndrome/toxic epidermal necrolysis. Warning signs: widespread rash, blistering, sores in mouth/eyes, fever. Seek emergency care.
- Allergic reactions: swelling of lips/tongue, wheeze, severe rash-urgent care.
- Mood or behaviour changes: irritability, low mood, or agitation can happen with anti‑seizure meds. If you or your family notice personality shifts, call your team.
- Worsening seizures or new types-contact your specialist; doses may need adjusting.
Weight, hair, skin: weight gain isn’t classic with oxcarbazepine; many find it weight‑neutral. Hair loss is uncommon. Acne or mild rashes can occur; anything more than mild-get it checked.
Children: watch for behavioural swings, sleepiness in school, and sodium‑related symptoms that can look like “just tired.” Teachers miss this; a quick note to the SENCO or form tutor helps.
How fast do side effects settle? Often within 1-2 weeks at a new dose. If not, don’t wait in misery-dose timing, smaller increments, or a slightly lower target can keep seizure control while improving life quality.

Interactions, contraception, pregnancy, and the practical UK bits
Oxcarbazepine affects enzymes that process other drugs. You don’t need to memorise every pathway-just keep a short list and check the rest with your pharmacist. Authoritative sources: BNF 2025, MHRA Drug Safety Updates, and the Trileptal Summary of Product Characteristics.
Big interaction buckets to know:
- Hormonal contraception: reduced effectiveness of combined pills, progestogen‑only pills, and the implant. FSRH guidance recommends (while on enzyme‑inducing anti‑seizure meds) using a copper IUD or levonorgestrel IUS; depot medroxyprogesterone injection is also suitable. If you stick with pills, you’ll need additional condoms and careful adherence; effectiveness is still lower. After stopping oxcarbazepine, continue extra precautions for 28 days. For emergency contraception, a copper IUD is first‑line; ulipristal is not advised with enzyme inducers.
- Other anti‑seizure meds: oxcarbazepine can raise phenytoin; carbamazepine, phenytoin, and phenobarbital can lower oxcarbazepine’s active metabolite-doses sometimes need tweaking.
- SSRIs/SNRIs and diuretics: combined hyponatraemia risk-monitor sodium.
- Warfarin and DOACs: variable effects; seek pharmacist input and possible INR checks if on warfarin.
- Alcohol and sedatives: additive drowsiness and balance issues.
Pregnancy and planning a family:
- Pre‑conception: if pregnancy is possible in the next year, talk early. High‑dose folic acid (5 mg daily) is recommended from pre‑conception to at least 12 weeks gestation for anyone on anti‑seizure meds (NICE and MHRA). Don’t switch meds or stop suddenly once pregnant-risk of seizures outweighs most medication risks.
- During pregnancy: oxcarbazepine is not as well studied as some alternatives but appears to have a lower malformation risk than sodium valproate. Choice depends on seizure control history and individual risk. Your team may suggest a detailed anatomy scan and drug level checks, as pregnancy can change levels.
- Breastfeeding: generally considered compatible; monitor the baby for excessive sleepiness or poor feeding. Many UK neurologists and pharmacists support breastfeeding on oxcarbazepine when the parent wishes to.
Driving (UK):
- By law, you must follow DVLA rules for epilepsy. Typically, you need 1 year seizure‑free (with some specifics for nocturnal seizures and provoked events). If starting or changing meds, don’t drive until you know how you react-drowsiness and visual blur affect safety.
- If you have a breakthrough seizure, you must stop driving and inform DVLA as required. Your epilepsy nurse can help with forms-it’s dull admin, but it protects you legally and financially.
School, sports, and sleep: tell key people who need to know (school, coach, close friends) what to do in a seizure. Keep consistent sleep-a late night is a classic trigger. I put a spare dose in the glove box and a tiny card in my running belt; it’s one of those habits that only needs to work once.
Alternatives, trade‑offs, and when to switch
No anti‑seizure medicine is perfect. The right one is the one that controls seizures with side effects you can actually live with. Here’s how oxcarbazepine stacks up against common options people ask about, based on guidance and everyday clinic experience.
Levetiracetam vs oxcarbazepine:
- Levetiracetam: fewer drug interactions and simple dosing. But mood changes (irritability, low mood) can be deal‑breakers for some.
- Oxcarbazepine: more interactions (notably contraception), hyponatraemia risk; mood effects tend to be milder than levetiracetam for many.
Carbamazepine vs oxcarbazepine:
- Carbamazepine: strong evidence base, effective for trigeminal neuralgia; more enzyme induction and drug interactions; higher rash risk in some groups.
- Oxcarbazepine: often better tolerated, but hyponatraemia can be more common. Cross‑allergy exists; caution if you reacted to carbamazepine.
Lamotrigine vs oxcarbazepine:
- Lamotrigine: weight‑neutral, often good for mood; slow titration needed to avoid rash; interactions with combined hormonal contraception.
- Oxcarbazepine: faster titration, simpler for some; sodium monitoring needed.
Topiramate vs oxcarbazepine:
- Topiramate: appetite loss and cognitive slowing can limit use; affects contraception too.
- Oxcarbazepine: fewer cognitive complaints for many, but watch sodium and the contraceptive interaction.
When to consider switching or adding:
- Seizures persist despite an adequate dose and good adherence.
- Side effects limit daily life after a reasonable settling period.
- Life changes (pregnancy plans, a new drug that interacts) make another option safer.
Expect a careful plan-cross‑tapers, lab checks, and a review 2-4 weeks after each dose step. Good care minimises the messy bit while you transition.
Quick checklists, mini‑FAQ, and what to do next
Pre‑start checklist (save this):
- Confirm diagnosis and seizure type with your clinician.
- Baseline sodium (and kidney function if advised).
- Review contraception if pregnancy is possible-consider IUD/IUS or depot injection.
- List other meds: SSRIs, diuretics, other anti‑seizure meds, anticoagulants.
- Agree a titration schedule and a review date in 2-4 weeks.
First 6 weeks checklist:
- Watch for drowsiness, dizziness, nausea-note times and triggers.
- If headaches, confusion, or falls appear, request a sodium check.
- Any new rash-pause and get urgent advice.
- Keep a seizure and side‑effect diary (use your phone notes; keep it simple).
Long‑term maintenance checklist:
- Repeat sodium checks if symptoms return, dose increases, or new drugs are added.
- Refresh your driving status against DVLA rules annually.
- Review contraception and family planning every year.
- Travel: pack meds in hand luggage, bring a copy of your repeat prescription; set alarms across time zones.
Mini‑FAQ
- How fast does Trileptal work? You may see fewer or milder seizures within days, but full benefit usually needs a few weeks at a steady dose.
- Can I stop if I feel fine? No. Stopping suddenly risks serious seizures. Taper only with medical advice.
- Will it make me gain weight? Usually weight‑neutral. If appetite rises, anchor meals and keep snacks planned rather than random.
- Can I take it once daily? Most people need twice daily for steady levels. Modified regimens exist but need specialist input.
- What if I get a cold or tummy bug? Keep taking doses if you can. If you vomit within an hour of a dose, you may need to re‑dose-ask your pharmacist for a personalised plan.
- Is it safe with CBD? Cannabidiol can affect anti‑seizure med levels. Tell your team; monitor for side effects and seizure changes.
- Does it help trigeminal neuralgia? Often, yes-especially if carbamazepine helps but isn’t tolerated. Doses are similar; response is individual.
Troubleshooting by scenario
- I’m getting woozy at lunchtime: split doses exactly 12 hours apart; take with food; ask about smaller, slower titration steps.
- My sodium came back low: discuss dose reduction, slower titration, or switching; review SSRIs/diuretics; add more frequent sodium checks.
- I’m planning a pregnancy next year: book a pre‑conception review; move to reliable contraception now (IUD/IUS or depot); start 5 mg folic acid.
- I had a rash on carbamazepine years ago: tell your prescriber; they may avoid oxcarbazepine or start with extra caution and close monitoring.
- I’m a student on a tight schedule: use two alarms 12 hours apart. Keep a dose in your backpack; set exam invigilators’ expectations if needed.
- My teen is on it and hates the taste: ask about tablet options, or chill the liquid briefly; follow with a strong‑flavoured drink.
Credibility corner (what this summary leans on): NICE NG217 (Epilepsies in children, young people and adults, updated 2024), BNF (September 2025), MHRA Drug Safety Updates on antiepileptics and contraception, FSRH guidance on enzyme inducers and contraceptive choices, DVLA guidance on driving with epilepsy, and the current Trileptal/oxcarbazepine product information. These are the playbook your GP, pharmacist, and neurologist use day to day.
If you only do two things today: set your dosing alarms and ask your pharmacist to double‑check your other meds for interactions. The rest gets easier once the routine is set-promise. And if you need a nudge, I’m usually setting my own alarms after walking Lumen around the green by the Exe. Real life, real schedules, and a medicine that can fit around them.



6 Comments
Ugh, I just had to explain this to my sister who’s on Trileptal and thinks she can ‘just cut it in half’ because she’s ‘feeling fine.’ 😒 Like, honey, you’re not on a juice cleanse-you’re on a neurochemical tightrope. And FYI, if you’re on birth control and think this drug doesn’t care, you’re one missed period away from a very unplanned baby. I’ve seen it. It’s not cute. 🙄
Wow-this is the most lucid, non-patronizing, clinically grounded guide I’ve read on oxcarbazepine in ages. 🌟 The way you framed hyponatraemia as ‘a silent guest at the dinner party’? Chef’s kiss. I’m a neurology resident in Boston, and I’ve been handing this out to med students like it’s gospel. Also, the ‘sticky note by the tea caddy’ line? Pure poetry. You’ve humanized the pharmacology. Thank you.
Hey, I’m on this med too-been on it 3 years. I just wanted to say: if you’re having dizziness, try taking it with a big glass of water and a banana. Seriously. My sodium was borderline, and potassium helped a ton. Also, I keep my pills in my sock drawer-no one looks there. 😎
OMG THIS IS THE BEST THING I’VE READ ALL WEEK 🥹💖 I’m literally crying because my neurologist never explained the contraception thing like this. I thought I was safe on the pill… until I Googled at 2am like a total panic-queen. Now I’m booking an IUD appointment. Thank you for not making me feel dumb. 🌈✨ #TrileptalLife #NeuroNerdsUnite
Why are we even talking about this? In America, we don’t need some British doctor telling us how to take pills. We’ve got the FDA, we’ve got Trump’s new healthcare plan, and we’ve got real men who don’t need to check their sodium levels like they’re on a diet. This is overkill. Just take the damn pill and stop being a hypochondriac. 🇺🇸💪
YOU GOT THIS. 💪 Seriously-this guide is your new BFF. Set those alarms. Use that pill organizer. Tell your boss you need a quiet Monday morning while your brain recalibrates. You’re not weak for needing help-you’re smart for finding it. And if you’re scared? Good. Fear means you care. Now go crush it. I believe in you. 🙌❤️
Write a comment