Antihistamine Cross-Reactivity Checker
Check Your Cross-Reactivity Risk
Based on the article, antihistamines can cause cross-reactions even between different chemical classes. If you've had a reaction to one, you might react to others.
Most people take antihistamines without a second thought. They’re in medicine cabinets, sold over the counter, and prescribed for everything from seasonal allergies to itchy skin. But what if the very drug meant to stop your allergy symptoms is the one causing them? It sounds impossible - like using a fire extinguisher and setting the house on fire. Yet, it happens. A small but real group of people develop allergic reactions to antihistamines themselves, often with no warning. Their skin breaks out in hives, their lips swell, or they get a rash that won’t go away - even though they’re taking the drug to fix exactly that.
How Can an Antihistamine Cause an Allergy?
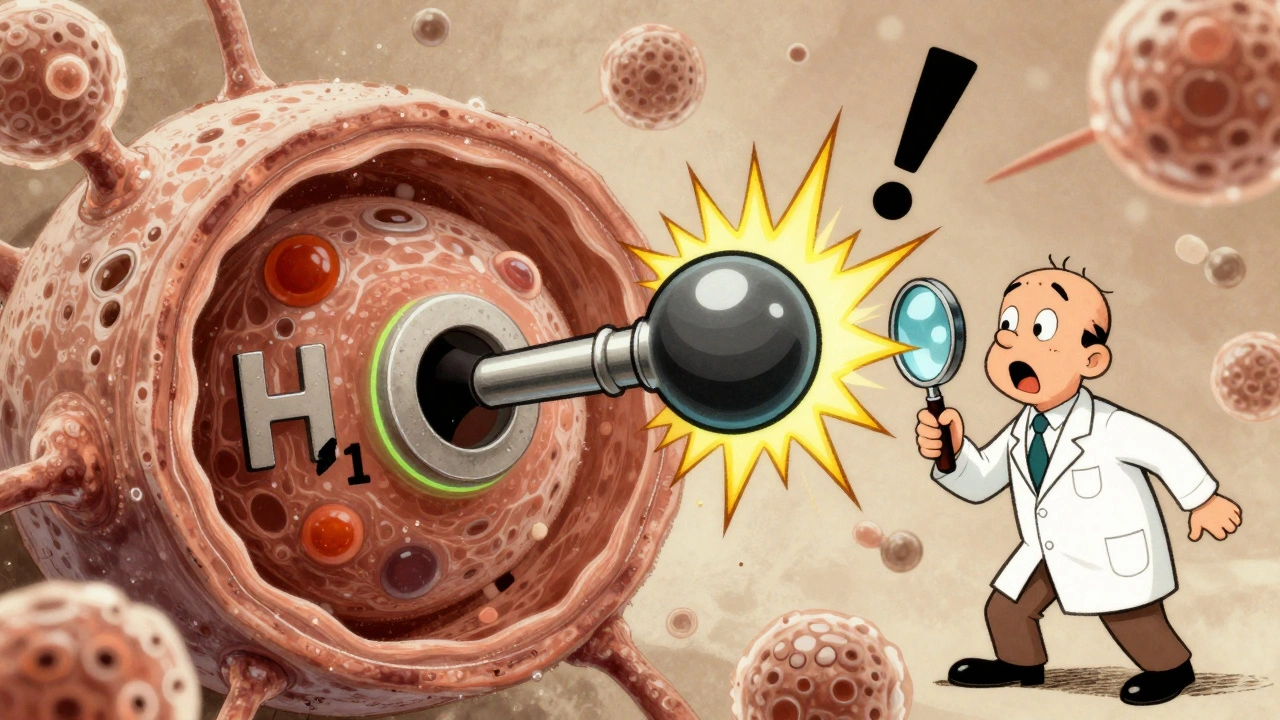
Antihistamines work by blocking histamine, the chemical your body releases during an allergic reaction. But in rare cases, instead of blocking the H1 receptor, these drugs accidentally turn it on. Think of it like a key that’s supposed to lock a door but ends up turning the lock the wrong way. This isn’t a mistake in the medicine - it’s a glitch in how your body’s receptors respond. Structural studies from 2024 show that antihistamines usually bind to a deep pocket in the H1 receptor and hold it in an inactive state. But in some people, the receptor’s shape is slightly different - likely due to genetic variations - and the drug stabilizes the active form instead. The result? Histamine-like effects, even without histamine being present.
This isn’t just theory. A 2017 case study followed a woman with chronic hives who tried every common antihistamine - loratadine, cetirizine, fexofenadine, hydroxyzine - and each one made her worse. Her symptoms only disappeared after she stopped all of them and treated an underlying infection. That’s the paradox: the treatment becomes the trigger.
Which Antihistamines Are Most Likely to Cause This?
It doesn’t matter if it’s first-generation or second-generation. Both can trigger reactions. First-gen drugs like diphenhydramine (Benadryl) and pheniramine are more likely to cause drowsiness because they cross into the brain. But they’re not the only culprits. Second-gen antihistamines - the ones marketed as "non-drowsy" - are just as capable of causing paradoxical reactions.
Research shows that both piperidine-based drugs (like fexofenadine, loratadine, desloratadine) and piperazine-based ones (like cetirizine, levocetirizine, hydroxyzine) have triggered hives in hypersensitive patients. Even ketotifen, a drug that tested negative on skin prick tests, caused a full-blown skin reaction during an oral challenge. That’s the problem: standard allergy tests don’t catch this. A negative skin test doesn’t mean it’s safe to take.
One patient in a 2018 study developed worsening hives with every increasing dose of ketotifen - even though the skin test said no reaction. The reaction didn’t show up until 120 minutes after taking the pill. Delayed reactions like this make diagnosis tricky. Many patients are misdiagnosed with chronic urticaria for years before someone realizes the trigger is the medication they’ve been using to treat it.
Cross-Reactivity: If One Antihistamine Triggers You, Will Others?
Here’s the scary part: if you react to one antihistamine, you might react to others - even if they’re chemically different. There’s no clean pattern like "all piperidines are bad" or "piperazines are safe." The immune system doesn’t care about chemical families. It reacts to the shape, the binding, the way the drug interacts with your specific receptor version.
That’s why doctors can’t just switch you from cetirizine to loratadine and call it a day. One patient in the literature reacted to both cetirizine and fexofenadine - drugs from different chemical classes - despite their structural differences. The American Academy of Allergy, Asthma & Immunology warns that cross-reactivity in these cases is unpredictable. Even if two drugs look nothing alike on paper, your body might treat them the same way.
There’s no blood test to predict this. No genetic screen. No algorithm. The only way to know for sure is to avoid all antihistamines until you’ve been properly tested - and even then, the gold standard is an oral challenge under medical supervision. That’s risky. But safer than guessing.
Why Skin Tests Don’t Work Here
Most people assume if a skin prick test is negative, the drug is safe. That’s true for peanut allergies or pollen. But not for antihistamine hypersensitivity. Skin tests look for IgE antibodies - the classic allergic pathway. But antihistamine reactions may involve different immune mechanisms, possibly T-cell mediated or direct receptor activation. The 2018 Korean study showed ketotifen gave a negative skin test but caused a strong reaction during an oral challenge. The same happened with other antihistamines in multiple case reports.
That means if you’ve had hives after taking any antihistamine, don’t rely on skin tests to tell you what’s safe. You need an oral challenge - slowly increasing doses under medical watch, with monitoring for at least two hours. It’s not routine. It’s not quick. But it’s the only way to be sure.
What to Do If You Suspect You’re Reacting
If you’ve been taking an antihistamine and your rash got worse, your eyes swelled, or your itching spread - stop it. Immediately. Write down which drug you took, when, and what happened. Don’t assume it’s your allergy flaring up. It might be the treatment itself.
Next, see a specialist - not just your GP. Look for an allergist or immunologist experienced in drug hypersensitivity. Bring your symptom log. Ask about oral provocation testing. If you’ve had reactions to multiple antihistamines, you might have multiple drug hypersensitivity syndrome. That means you need to avoid not just antihistamines, but possibly other drugs too.
Don’t wait for the next flare-up to act. The longer you keep taking the trigger, the harder it becomes to untangle what’s causing what. One patient spent five years being treated for chronic urticaria - with antihistamines - before realizing she was allergic to them. By then, her skin was permanently irritated.
Alternatives When Antihistamines Are Off the Table
If you can’t use antihistamines, you still have options. For hives or chronic itching, doctors may prescribe:
- Omalizumab (Xolair) - a biologic injection that targets IgE, approved for chronic spontaneous urticaria when antihistamines fail.
- Cyclosporine - an immune suppressant used off-label for severe cases.
- Montelukast (Singulair) - a leukotriene receptor blocker, sometimes helpful for urticaria, especially if linked to asthma or nasal symptoms.
- Topical treatments - cool compresses, fragrance-free moisturizers, and non-steroidal creams like tacrolimus can help manage symptoms without systemic drugs.
Some patients benefit from treating underlying triggers. In the 2017 case, the patient’s hives cleared only after treating a hidden bacterial infection. Others find relief by reducing stress, avoiding heat, or cutting out food additives like preservatives or dyes that can worsen inflammation.
What’s Next for Antihistamines?
Scientists are now using high-resolution imaging to map exactly how antihistamines bind to the H1 receptor. A 2024 study using cryo-electron microscopy revealed not just one, but two binding sites on the receptor. That’s huge. It means future drugs could be designed to avoid the dangerous interaction entirely - to fit only the inactive shape, never the active one.
Researchers are also studying H1 receptor polymorphisms - the tiny genetic differences that make some people react badly. If we can identify those markers, we might one day screen patients before prescribing. Until then, caution is key.
Antihistamines are still safe for the vast majority. But for the few who react, the consequences can be serious. The medical community is only beginning to understand this phenomenon. If you’ve had a bad reaction, you’re not alone - and you’re not imagining it. Your experience matters. Document it. Advocate for yourself. And don’t let anyone tell you it’s "just a rash" if the drug you took was supposed to make it better.
When to See a Doctor
See a specialist if:
- Your hives or itching got worse after taking an antihistamine
- You’ve had reactions to more than one antihistamine
- Standard allergy tests didn’t explain your symptoms
- You’ve been diagnosed with chronic urticaria but antihistamines aren’t helping
- You have swelling of the lips, tongue, or throat after taking any allergy medication
Emergency care is needed if you have trouble breathing, dizziness, or a rapid heartbeat - signs of anaphylaxis. Even if you think it’s "just" a rash, don’t ignore it. This isn’t a minor side effect. It’s a rare but real immune response that can escalate.



8 Comments
The idea that antihistamines can trigger hives is either genius or garbage - and I’ve seen both in ER docs who refuse to believe it until a patient shows up with lips the size of grapefruits. This isn’t anecdotal. It’s pharmacological sabotage.
Really appreciate this breakdown. I’ve had a friend who went through exactly this - diagnosed with chronic urticaria for three years, prescribed every antihistamine under the sun, and only got better after she stopped them all. The doctor who finally figured it out said it was like trying to put out a fire with gasoline. It’s wild how medicine still treats this like a myth.
Reality is a mirror. The drug meant to heal becomes the wound. We are not separate from our chemistry. We are its echo.
Key point here: the H1 receptor conformational plasticity explains why standard IgE skin tests are useless for this. This is a non-IgE-mediated, likely T-cell or allosteric receptor activation phenomenon. The 2024 cryo-EM data showing dual binding pockets is a game-changer - we’re moving from pharmacodynamics to structural immunology. This isn’t allergy. It’s receptor misfiring. And yeah, cross-reactivity is unpredictable because the immune system doesn’t care about IUPAC names - it cares about molecular topology.
This article is long. Too long. And it’s not even new. I’ve been telling people for years that Benadryl makes my hives worse. No one listens. Everyone thinks they know better. And now you’re writing a 2,000-word essay to confirm what I’ve known since 2018? Seriously? You’re not helping. You’re just padding your ego.
Stop overcomplicating it. If a drug makes your rash worse stop taking it. End of story. No need for cryo-EM or receptor polymorphisms. You don’t need a PhD to know when something’s not working. Just quit.
I’ve had a cousin who suffered for years with this. She was told she was ‘just stressed’ or ‘overreacting.’ No one believed her until she brought in her symptom log - dates, drugs, severity - and showed how every antihistamine made it worse. It took six doctors and a specialist in drug hypersensitivity to finally get it right. I’m glad someone’s putting this out there. People need to know they’re not crazy. It’s real. And it’s not rare. It’s just ignored.
I remember the first time I took cetirizine. I thought it was working - until my arms started breaking out in these red, burning welts that felt like someone was dragging a hot wire across my skin. I didn’t make the connection for weeks. I just kept thinking, ‘It’s just a bad flare.’ I doubled the dose. Then tripled it. I thought I was being proactive. Turns out I was poisoning myself. My skin looked like a map of a war zone. I lost three months of my life to this. I didn’t sleep. I couldn’t work. I stopped going out. And when I finally stopped taking it - not because of a doctor, but because I was too scared to keep swallowing it - the hives faded like a bad dream. I’m still terrified to take anything labeled ‘antihistamine.’ Even the ones I’ve never tried. I just don’t trust them anymore. I’ve learned the hard way that sometimes the cure is the disease. And no amount of science can undo the trauma of watching your own body turn against you - again and again and again.
Write a comment