Imagine your kidneys are like fine coffee filters. They let waste and extra fluid out, but keep blood and protein safely inside. Now imagine your immune system-designed to protect you-starts attacking those filters. That’s glomerulonephritis. It’s not a single disease. It’s a group of conditions where your body’s own defenses turn against the tiny filtering units in your kidneys, called glomeruli. And when those filters break down, protein leaks into your urine, blood shows up where it shouldn’t, and your kidneys struggle to keep up.
What Exactly Happens Inside the Kidneys?
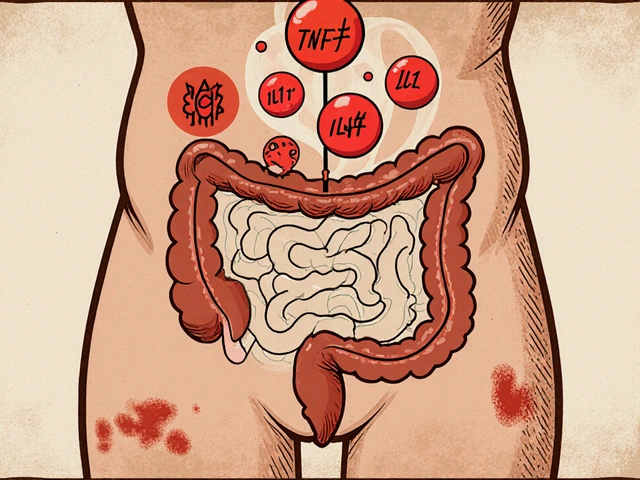
Each kidney has about a million glomeruli. They’re made of three layers: the inner endothelial cells, the basement membrane (a tough mesh), and the outer podocytes-special cells that wrap around the filter like fingers. Together, they act as a precision sieve. In glomerulonephritis, something goes wrong in the immune system. Antibodies or complement proteins build up in or around these layers. This triggers inflammation. The glomeruli swell. The filter gets leaky.There are two main ways this plays out clinically. One is nephritic syndrome: blood in the urine, high blood pressure, reduced kidney function, and swelling. Your creatinine might jump to 1.5-3.0 mg/dL. The other is nephrotic syndrome: huge amounts of protein in the urine (over 3.5 grams a day), low blood protein, high cholesterol, and swelling in the legs or face. Both mean your kidneys are struggling.
The Major Types of Glomerulonephritis
Not all glomerulonephritis is the same. The immune attack can come from different directions.IgA nephropathy is the most common form worldwide. It happens when IgA antibodies, usually fighting infections, get stuck in the glomeruli. In North America, about 2.5 people per 100,000 get it each year. About 20-40% of those will eventually need dialysis after 20 years. It often shows up after a cold or sore throat-like your immune system got distracted and kept going.
C3 glomerulonephritis (C3G) is rarer but more aggressive. Here, the complement system-a part of the immune system that helps clear germs-goes rogue. Instead of turning off after doing its job, it stays on. C3 protein builds up in the glomeruli at levels 3-5 times higher than normal. About 60-70% of C3G cases involve an autoantibody called C3 nephritic factor (C3NeF), which tricks the system into attacking itself.
Immune complex-mediated membranoproliferative GN (IC-MPGN) is caused by immune complexes-clumps of antibodies and antigens-getting trapped in the filter. Biopsies show dense deposits in 95% of cases. It’s often linked to chronic infections like hepatitis or autoimmune diseases like lupus.
Lupus nephritis affects half to two-thirds of people with systemic lupus erythematosus. It’s not just a kidney problem-it’s a sign the whole immune system is out of control. With treatment, 70-80% of patients avoid kidney failure over 10 years.
Post-streptococcal GN mostly hits kids. After a strep throat or skin infection, the immune system overreacts. But here’s the good news: 95% of children recover fully within 6-8 weeks.
Why Diagnosis Takes Time-and a Biopsy
There’s no blood test that says, “You have glomerulonephritis.” You might have blood in your urine, swelling, or high blood pressure. But those symptoms show up in many conditions. The only way to know for sure is a kidney biopsy.That means a needle goes into your kidney, and a tiny piece of tissue is pulled out. It sounds scary. Complications like bleeding happen in 3-5% of cases. But it’s necessary. Under the microscope, nephropathologists look for patterns: where the immune deposits are, what kind of proteins are stuck there, how the cells are damaged. It takes 5-7 years of training to read these patterns accurately.
Patients report an average of 4.2 months from first symptoms to diagnosis. One in three sees three or more doctors before getting answers. That delay can cost you kidney function. The sooner you know what you’re dealing with, the better your chances.
Treatment: Steroids, Side Effects, and New Hope
For decades, the go-to treatment has been corticosteroids like prednisone. They calm the immune system. About 60-80% of patients respond at first. But the cost is high. Seventy-two percent gain weight. Thirty-five percent get infections. Twenty-eight percent lose bone density-some with fractures after just 18 months.And here’s the hard truth: 30-50% of patients don’t respond well at all, even with high doses. That’s why new treatments are urgent.
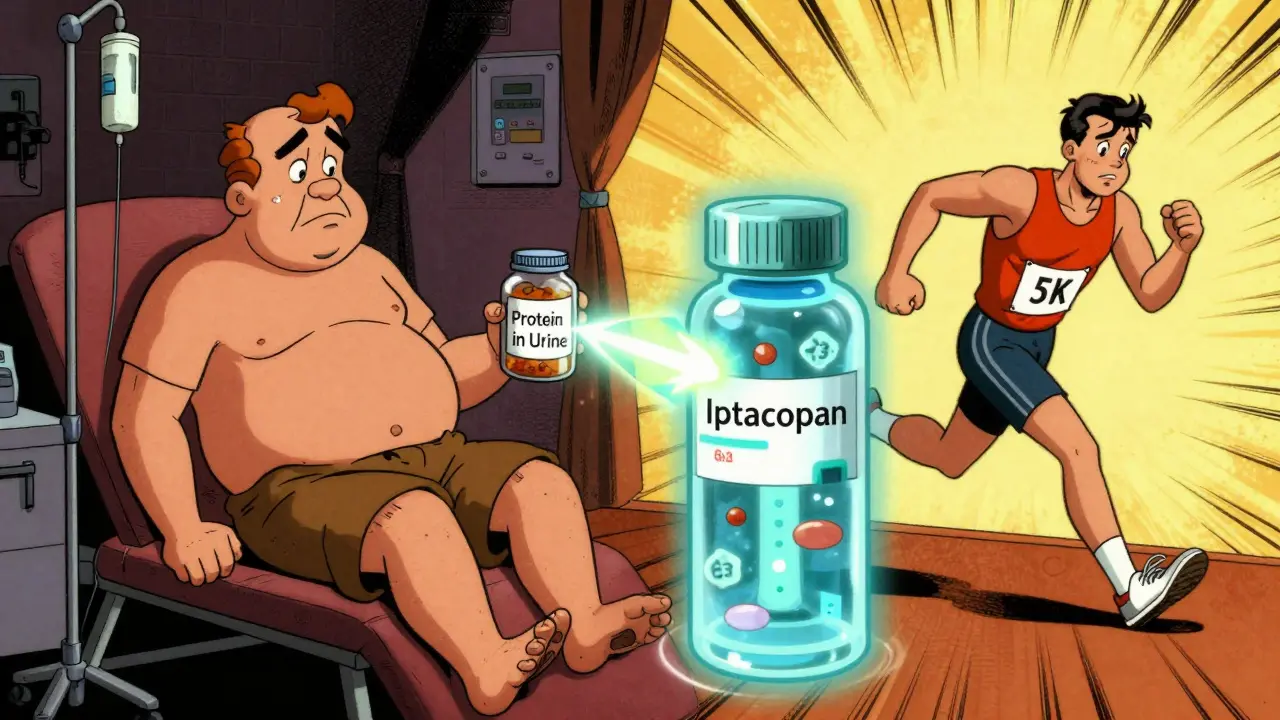
One breakthrough is iptacopan, a drug approved for C3G in early 2023. In trials, it cut proteinuria by 52% in 12 months. It targets a specific part of the complement system-C3-without wiping out the whole immune response. It’s not cheap: about $500,000 a year. But for someone who would otherwise need dialysis, it’s life-changing.
Other targeted drugs like eculizumab and rituximab are also showing promise. One Reddit user shared that starting rituximab within two months of diagnosis kept them off dialysis. That’s the kind of story that gives hope.
But access isn’t equal. In low-income countries, patients have 90% less access to these new drugs. Even in the U.S., insurance battles can delay treatment for months. The KDIGO guidelines now say: try standard therapy for at least six months before moving to expensive targeted drugs. But for some, waiting that long means losing kidney function for good.
What Patients Are Really Saying
Behind the statistics are real people. On support forums like Inspire.com, 78% of posts talk about swelling-how their ankles puff up, how their face looks different in the mirror. Forty-two percent say fatigue is their worst symptom. It’s not just tiredness. It’s the kind of exhaustion that makes getting out of bed feel impossible.Sixty-three percent worry about steroid side effects. One woman wrote: “Prednisone gave me osteoporosis and two broken vertebrae. I didn’t know the cure could hurt you worse than the disease.”
But there’s also hope. People who get diagnosed early and find the right treatment often report returning to work, playing with their kids, hiking again. One man on Reddit said, “I didn’t know I was sick until I passed blood in my urine. Two months later, I was on a new drug. Now I’m running 5Ks.”
The Future: Personalized Medicine
The field is shifting fast. Instead of treating all glomerulonephritis the same, doctors are starting to look at the molecular fingerprint of each case. Are you a C3G patient with C3NeF? Do you have a genetic mutation in your complement regulators? Is your IgA abnormal in structure? These details matter.By 2028, the global market for GN treatments is expected to hit $4.7 billion. Why? Because science is catching up. New classification systems now use biomarkers alongside biopsies, predicting treatment response with 85% accuracy-up from 65% with biopsies alone.
Dr. Richard Lafayette from Stanford predicts that within five years, genetic and proteomic profiling will guide therapy. Instead of guessing which drug to try, you’ll get a personalized plan. That could push success rates from 60-70% to over 85%.
But the big question remains: who gets these advances? Glomerulonephritis accounts for 10-15% of new dialysis cases in the U.S. That’s 12,000-18,000 people a year. If we don’t fix access, we’ll just be giving high-tech solutions to the wealthy while others wait.
What You Can Do
If you’ve been told you have protein or blood in your urine, don’t ignore it. See a nephrologist. Ask for a biopsy if it’s not offered. Track your blood pressure. Watch for swelling. Keep a symptom journal.If you’re already diagnosed, ask about your specific type. Is it IgA? C3G? Lupus? Ask if genetic testing or biomarker panels are available. Don’t accept “we’ll start with steroids” as the end of the conversation. Ask about clinical trials. Ask about alternatives.
Glomerulonephritis isn’t a death sentence. It’s a signal. Your immune system is screaming. The goal isn’t just to suppress it-it’s to redirect it. And with new tools, we’re getting closer than ever.




9 Comments
Just read this after my cousin got diagnosed with IgA nephropathy 😔 Honestly, I had no idea kidney filters could get attacked by your own body. That analogy of coffee filters? So spot on. I’m sending this to her doctor just to make sure they’re considering all the new drugs like iptacopan. She’s only 32 and already scared stiff.
Oh wow, another ‘you’re immune system is a traitor’ piece. How original. Next up: ‘Your pancreas is having an identity crisis.’ At least the author knows how to write-unlike the 90% of medical bloggers who think ‘glomeruli’ is a brand of yoga mat.
Glomerular filtration rate’s the key metric here, but most clinicians still rely on outdated KDIGO protocols. The real issue is complement dysregulation-C3NeF titers aren’t being tracked in 70% of cases. We’re treating symptoms, not the underlying immune dysbiosis. And don’t even get me started on steroid-induced osteonecrosis.
As someone who’s been on rituximab for 18 months, I can confirm-this isn’t just academic. My proteinuria dropped from 8g/day to 0.9g. But the access issues? Real. My insurance denied it for 5 months. I had to appeal twice, submit 3 letters from nephrologists, and cry in a voicemail to the medical director. If you’re reading this and you’re on the waiting list-don’t give up. Keep pushing. There’s a path.
so like... our bodies are just glitchy robots? and our immune system is the ai that went rogue? and now we're stuck paying $500k for a firmware update? 🤔
YOU’RE ALL IGNORING THE REAL ISSUE!!! THE PHARMA COMPANIES ARE MAKING BILLIONS OFF OUR PAIN!!! THEY KNOW THE TRUTH-STEROIDS ARE A SCAM!!! THEY’RE KILLING US WITH OSTEOPOROSIS AND DIABETES AND THEN SELLING US $500K DRUGS TO FIX WHAT THEY BROKE!!! THIS IS A SYSTEMIC CRIME!!!
why do people keep saying biopsy is necessary when most cases resolve on their own
Think about it. Every cell in your body is a tiny universe. Your glomeruli? They’re not just filters-they’re sacred temples of homeostasis. And when your immune system attacks them, it’s not disease-it’s cosmic rebellion. The body isn’t broken. It’s awakening. We’ve been trained to see inflammation as the enemy. But what if it’s the soul screaming for alignment? What if prednisone isn’t curing you-it’s silencing your inner truth? I’ve seen patients heal after ditching meds and doing breathwork, grounding, and chanting mantras to their kidneys. Science doesn’t measure soul resonance. But I do. And mine says: the body knows. We just forgot how to listen.
Actually, the real win here is the shift toward molecular phenotyping. We’re finally moving past ‘one-size-fits-all’ nephrology. If you’ve got C3NeF, iptacopan isn’t just an option-it’s the only rational choice. And yes, it’s expensive. But dialysis costs $90k/year. This drug? $500k over 5 years. Math isn’t hard. The problem isn’t the cost-it’s the bureaucracy. We need to stop treating rare diseases like they’re optional. If you’re going to diagnose it, you’ve got to treat it. Full stop.
Write a comment