Alcohol & Warfarin INR Risk Calculator
How Alcohol Affects Your INR
Alcohol can cause dangerous INR fluctuations. This tool estimates your bleeding risk based on your alcohol consumption.
\u26a0\uFE0F Warning: This calculator provides general guidance only. Always follow your doctor's advice and monitor your INR regularly.
Your INR Risk Assessment
Important Notes
- \u26a0\uFE0F Binge drinking (4+ units at once) can cause rapid INR spikes within 48 hours
- \u26a0\uFE0F Alcohol interacts differently with warfarin based on your genetics
- \u26a0\uFE0F INR above 3.5 increases bleeding risk by 30-50% per 0.5 point
- \u26a0\uFE0F Always inform your anticoagulation clinic if you increase alcohol consumption
If you're taking a blood thinner like warfarin, you've probably heard mixed things about alcohol. Some doctors say it's fine in small amounts. Others warn you to avoid it completely. The truth? It’s not black and white. But it is dangerous if you don’t understand how alcohol changes your blood’s ability to clot - and why that matters.
How Warfarin Works - And Why INR Matters
Warfarin, sold under the brand name Coumadin, has been used since the 1950s to stop dangerous blood clots. It doesn’t thin your blood like water. Instead, it blocks vitamin K, which your body needs to make clotting proteins. Without enough of those proteins, your blood takes longer to clot - which is exactly what you want if you have atrial fibrillation, a mechanical heart valve, or a history of deep vein thrombosis. But here’s the catch: the window for safety is tiny. Your doctor wants your INR (International Normalized Ratio) to stay between 2.0 and 3.0 for most conditions. For some, like those with a mechanical mitral valve, it might go up to 2.5-3.5. If your INR drops below 2.0, you’re at risk for clots. If it climbs above 3.5, your risk of bleeding shoots up. Every 0.5-point rise above your target INR means a 30-50% higher chance of bleeding. At an INR above 9, nearly 1 in 3 hospitalized patients will bleed. And 1 in 6 won’t survive. That’s not a hypothetical. That’s real data from patients who didn’t realize how much alcohol could push them over the edge.Alcohol Doesn’t Just Affect Your Liver - It Messes With Your INR
Alcohol doesn’t just make you feel loose. It interferes with how your body processes warfarin. The liver uses enzymes - mainly CYP2C9 - to break down warfarin. Alcohol competes for the same enzymes. When you drink, especially in large amounts, your liver gets busy processing alcohol and slows down warfarin metabolism. That means warfarin builds up in your blood. Your INR climbs. You bleed more easily. But it’s not always that simple. Sometimes, heavy drinking over days or weeks actually makes your liver work harder to clear warfarin. That can drop your INR. Suddenly, your blood clots too fast. You’re at risk for stroke or pulmonary embolism. This back-and-forth is why doctors hate unpredictable alcohol use. One weekend of binge drinking can send your INR from 2.4 to 4.8 in 48 hours. A 62-year-old man in the UK reported exactly that after six pints of beer. His INR jumped from 2.8 to 5.2. He ended up in the hospital with gastrointestinal bleeding. He didn’t think six beers were a big deal. But for someone on warfarin, they were.Genetics Play a Role - And You Might Not Know Yours
Not everyone reacts the same way to alcohol and warfarin. Some people have genetic variants that make them extra sensitive. The CYP2C9*2 and *3 variants mean their liver breaks down warfarin slowly. Combine that with alcohol, and the drug sticks around longer. Another gene, VKORC1, affects how your body responds to vitamin K. If you have the 1173G>A variant, alcohol can multiply your bleeding risk. Studies show these genetic differences aren’t rare. About 30% of people of European descent carry at least one of these variants. But most doctors don’t test for them unless you’ve had a bad reaction. If you’ve had unexplained bleeding or wild INR swings, ask your doctor: “Could my genes be making me more sensitive?”
How Much Alcohol Is Safe?
There’s no perfect number. But guidelines from the UK Chief Medical Officers and the British Heart Foundation are clear: no more than 14 units of alcohol per week. That’s about six pints of average-strength beer or six 175ml glasses of wine. Spread it over three or more days. Don’t save it all for Friday night. Binge drinking - four or more drinks in one sitting for women, five or more for men - is the biggest danger. It causes sudden, sharp INR spikes. Even if you usually drink moderately, one night of heavy drinking can undo weeks of stable control. The NHS says it plainly: “Drinking heavily, especially binge drinking, is dangerous while taking warfarin.” Medical News Today adds that exceeding 14 drinks per week for men or 7 for women significantly raises bleeding risk. And that’s not a suggestion. That’s a warning backed by clinical data.What About Newer Blood Thinners?
If you’re on a DOAC - like apixaban, rivaroxaban, or dabigatran - alcohol is less risky. These drugs don’t rely on vitamin K or the same liver enzymes as warfarin. So, they don’t interact the same way. But that doesn’t mean you can drink freely. Alcohol still increases your risk of stomach bleeding, especially if you’re older or take NSAIDs like ibuprofen. It also raises your chance of falls. And if you do bleed, reversing DOACs is harder. There’s no vitamin K fix. And while reversal agents like andexanet alfa exist, they’re expensive, hard to get, and only work for certain drugs. Bottom line: If you’re on a DOAC, moderation still matters. But if you’re on warfarin? Alcohol is a wild card. And you’re the one holding the dice.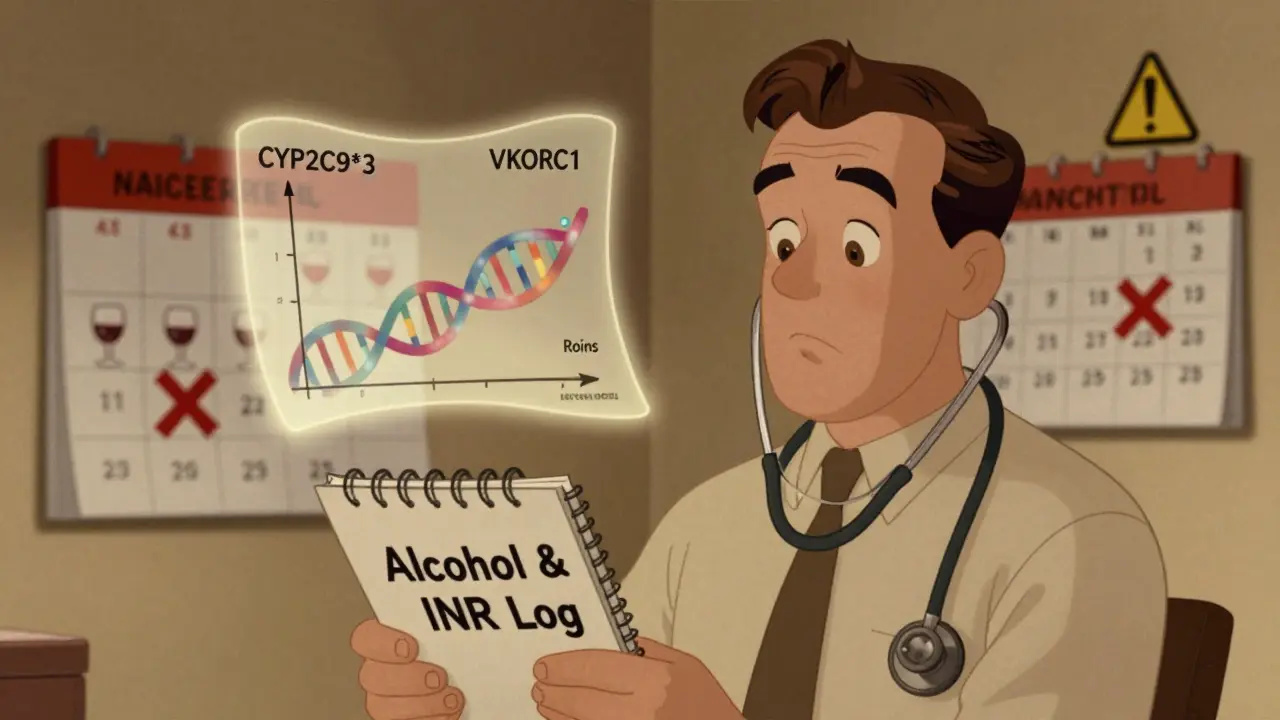
Signs You’re Bleeding - Don’t Wait
You don’t always feel internal bleeding. That’s the danger. Watch for these red flags:- Red or brown urine
- Tar-like or bright red stools
- Bleeding gums or nosebleeds that won’t stop
- Unusually heavy menstrual periods
- Brown or bright red vomit
- Unexplained bruising, especially on your arms or legs
- Severe headache, dizziness, or weakness - could mean bleeding in the brain
What to Do If You Drink
If you choose to drink:- Stick to the 14-unit weekly limit - and spread it out.
- Avoid binge drinking at all costs.
- Tell your anticoagulation clinic or doctor if you’ve had more than usual.
- Get your INR checked sooner than usual after drinking.
- Don’t mix alcohol with aspirin, ibuprofen, or other NSAIDs - they increase stomach bleeding risk.
- Keep a log: write down what you drank, when, and your INR result. Patterns matter.
Why This Isn’t Just About Warfarin
Warfarin isn’t going away. Even with newer drugs, about 2.5 million Americans still take it. That’s because it’s cheap, effective, and works for complex cases. But it demands attention. And alcohol is one of the most common reasons patients lose control of their INR. The American Heart Association estimates 2.7 to 6.1 million Americans have atrial fibrillation - the most common reason for warfarin use. And 30-40% of them drink alcohol regularly. That’s millions of people walking a tightrope between preventing a stroke and risking a bleed. This isn’t about fear. It’s about control. You can drink. But you have to do it with eyes wide open. Your INR doesn’t lie. And if you ignore the signals, your body will pay the price.Can I have one glass of wine with warfarin?
Yes - if it’s just one glass and you don’t drink often. A single 175ml glass of wine (about 2 units) is unlikely to cause problems if you’re consistent and your INR is stable. But don’t make it a daily habit. Even small amounts can add up over time, especially if you have genetic factors that make you sensitive. Always tell your doctor if you start drinking regularly.
Does beer affect warfarin differently than wine or spirits?
No. It’s not the type of alcohol - it’s the amount of ethanol. One pint of beer, one glass of wine, and one shot of spirits all contain about the same amount of alcohol (roughly 1.5-2 units). What matters is how much you drink and how often. Binge drinking any kind of alcohol is dangerous. Consistent, moderate intake is safer than occasional heavy use.
How long after drinking should I wait before checking my INR?
Wait at least 48 hours after your last drink. Alcohol can affect your INR for up to two days, especially if you drank heavily. Testing too soon might show a false reading. If you had a binge, wait until you’re completely sober and then get tested. Your doctor may want to test you sooner if you’ve had previous issues.
Can I drink alcohol if I’m on a DOAC like apixaban?
You can, but it’s not risk-free. DOACs don’t interact with alcohol the same way warfarin does, but alcohol still increases your risk of stomach bleeding and falls. If you drink regularly, talk to your doctor. They may suggest reducing alcohol, especially if you’re over 65, have kidney problems, or take other medications like aspirin. Moderation is still key.
What should I do if my INR is too high after drinking?
If your INR is above 5.0, call your doctor immediately. Do not stop your warfarin unless instructed. For INR above 9, you may need plasma transfusion - vitamin K or skipping a dose won’t work fast enough. In the hospital, doctors may use plasma to reverse the effect within hours. At home, your doctor might reduce your dose and schedule a follow-up test in 2-3 days. Never ignore a high INR, even if you feel fine.





9 Comments
Man, I never realized how wild warfarin and alcohol can get. Back home in India, everyone just sips beer with dinner like it’s nothing. But this? This is like walking through a minefield blindfolded. I’ve got an uncle on warfarin - he drinks two beers every Friday. No one told him about INR swings. Scary stuff.
As a board-certified clinical pharmacist with over 18 years managing anticoagulation clinics, I can confirm: alcohol-induced INR variability is one of the most preventable causes of hospitalization in patients on warfarin. The liver’s CYP2C9 enzyme saturation kinetics are non-linear and highly dose-dependent. Even moderate consumption disrupts steady-state pharmacokinetics. Patients must be educated that 'one glass' is not a free pass - it’s a pharmacodynamic wildcard. Documented cases show 48-hour INR spikes exceeding 5.0 after just 2 standard drinks in genetically susceptible individuals. This isn't opinion. It's evidence-based practice.
Let’s be real - we’re all just atoms in a quantum soup of biochemical chaos. Warfarin? It’s not a drug. It’s a metaphysical negotiation between your liver and your destiny. Alcohol? It’s the universe’s way of whispering, 'What if you stopped controlling everything?' The INR doesn’t lie - but neither does your soul when it craves that one glass of red. Are we treating a condition… or suppressing a cry for freedom? I’ve seen men on warfarin who quit drinking… and then lost their will to live. Is stability worth that cost? I don’t know. But I know this: the liver doesn’t forgive. It just waits.
There is a fundamental flaw in the assumption that 'moderation' is safe. The literature is unequivocal: there is no safe threshold for alcohol consumption in patients with CYP2C9*2 or *3 polymorphisms, which constitute nearly one-third of the Caucasian population. Furthermore, the concept of 'spread out' drinking is biologically misleading - cumulative exposure over 7 days still induces hepatic enzyme suppression. The UK guidelines are outdated and based on population averages, not individual pharmacogenomics. Any recommendation that permits alcohol use in warfarin patients is clinically irresponsible. Period.
just read this and cried a little. my mom’s on warfarin and she drinks wine every night. i’ve been scared to say anything. now i know why her inr was 6.2 last month. thanks for this. i’m gonna talk to her.
Yeah right, alcohol messes with warfarin. Next you’ll say oxygen causes blood thinning. Wake up. It’s all fearmongering. My buddy’s been drinking whiskey daily for 10 years on warfarin. INR’s always 2.5. Coincidence? Nah. You’re just scared of fun.
Okay but let’s be honest - the whole '14 units a week' thing is a joke. That’s like saying 'drive under 70mph' in a school zone while you’re on a highway. Who even measures units? And why does everyone act like alcohol is the villain when NSAIDs are way worse? I’ve seen people take ibuprofen daily and never get an INR check. Meanwhile, someone has a glass of wine and suddenly it’s 'ALCOHOL IS KILLING YOU'. It’s selective outrage. Also, DOACs aren’t safer - they’re just more expensive and you can’t reverse them. So now you’re stuck bleeding out with no way to fix it. Thanks, Big Pharma. And don’t even get me started on 'telehealth alcohol counseling' - that’s just therapy for people who don’t know how to say no to happy hour.
This is exactly the kind of clear, compassionate info we need. So many people think 'I’m fine, I only drink on weekends' - but it’s the inconsistency that kills. I work with elderly patients in Delhi, and many don’t even know what INR means. Sharing this with my clinic tomorrow. Let’s stop treating patients like they’re failing - and start giving them real tools. One glass, spread out, logged, and checked. That’s the path. Not fear. Not shame. Just clarity.
Frankly, the entire article is a reductive pharmacological narrative that ignores the epistemological limitations of INR as a biomarker. The CYP2C9 polymorphism data is statistically significant but clinically overinterpreted. Moreover, the conflation of ethanol metabolism with warfarin pharmacokinetics assumes a monolithic hepatic pathway - when in reality, the enterohepatic recirculation and gut microbiome modulation of vitamin K are grossly underrepresented in current guidelines. The real issue? Medical paternalism disguised as patient safety. Let adults make informed choices. Or better yet - stop prescribing warfarin entirely and let DOACs dominate. But don’t moralize about beer.
Write a comment