When you pick up a prescription at the pharmacy and see a generic version of your brand-name drug, you’re seeing the result of one of the most efficient regulatory systems in modern medicine. The FDA’s approval process for generic drugs isn’t just paperwork-it’s a precise, science-driven pathway that saves patients billions each year. But how does it actually work? If you’ve ever wondered why a generic pill costs 80% less than the brand-name version, or how the FDA makes sure it’s just as safe and effective, here’s the full, real-world breakdown.
What Is an ANDA, and Why Does It Exist?
The Abbreviated New Drug Application, or ANDA, is the legal pathway the FDA uses to approve generic drugs. It’s called "abbreviated" because it doesn’t require the same long, expensive clinical trials that brand-name drugs go through. Instead, generic manufacturers prove their product is the same as an already-approved drug-called the Reference Listed Drug, or RLD.
This system was created by the Hatch-Waxman Act of 1984. Before that, generics couldn’t enter the market until patents expired, and even then, there was no clear way to prove they worked the same. Hatch-Waxman changed everything. It gave brand-name companies a limited time of market exclusivity (usually 20 years from patent filing), but also created a fast track for generics to follow once that window opened.
Today, 90% of all prescriptions filled in the U.S. are for generic drugs. They make up just 23% of total drug spending. That’s because the ANDA process cuts development costs from billions to millions. A brand-name drug can cost $2.6 billion and take 10-15 years to get approved. A generic? Around $1-5 million and 3-4 years.
Step 1: Identify the Reference Listed Drug (RLD)
Before you even start writing an ANDA, you need to pick the right brand-name drug to copy. Not every brand has a generic version, and not every generic can copy just any brand. The FDA publishes the Orange Book-a public list of all approved drugs with their therapeutic equivalence ratings. This is where you find your RLD.
You can’t pick just any brand. The RLD must be the one the FDA has officially designated as the standard for comparison. For example, if you want to make a generic version of Lipitor (atorvastatin), you must use the FDA-approved Lipitor as your RLD. You can’t use a different formulation or a version sold in another country.
Once you pick the RLD, you’re locked in. Everything in your ANDA-strength, dosage form, route of administration-must match it exactly. No exceptions.
Step 2: Prove Pharmaceutical Equivalence
Pharmaceutical equivalence means your generic has the same active ingredient, in the same amount, in the same form, and given the same way as the brand.
So if the brand is a 20mg tablet taken by mouth, your generic must be a 20mg tablet taken by mouth. Same active ingredient-atorvastatin calcium. Same strength. Same shape. Same coating.
Inactive ingredients? Those can be different. Fillers, dyes, binders-those are allowed to vary. But they still have to be safe. The FDA checks that none of these excipients cause harm, especially in sensitive populations like kids or people with allergies.
This part sounds simple, but it’s where many applications fail. If your tablet has a different binder that affects how quickly the drug dissolves, you’re not pharmaceutically equivalent. And if you’re not equivalent here, you don’t even get to the next step.
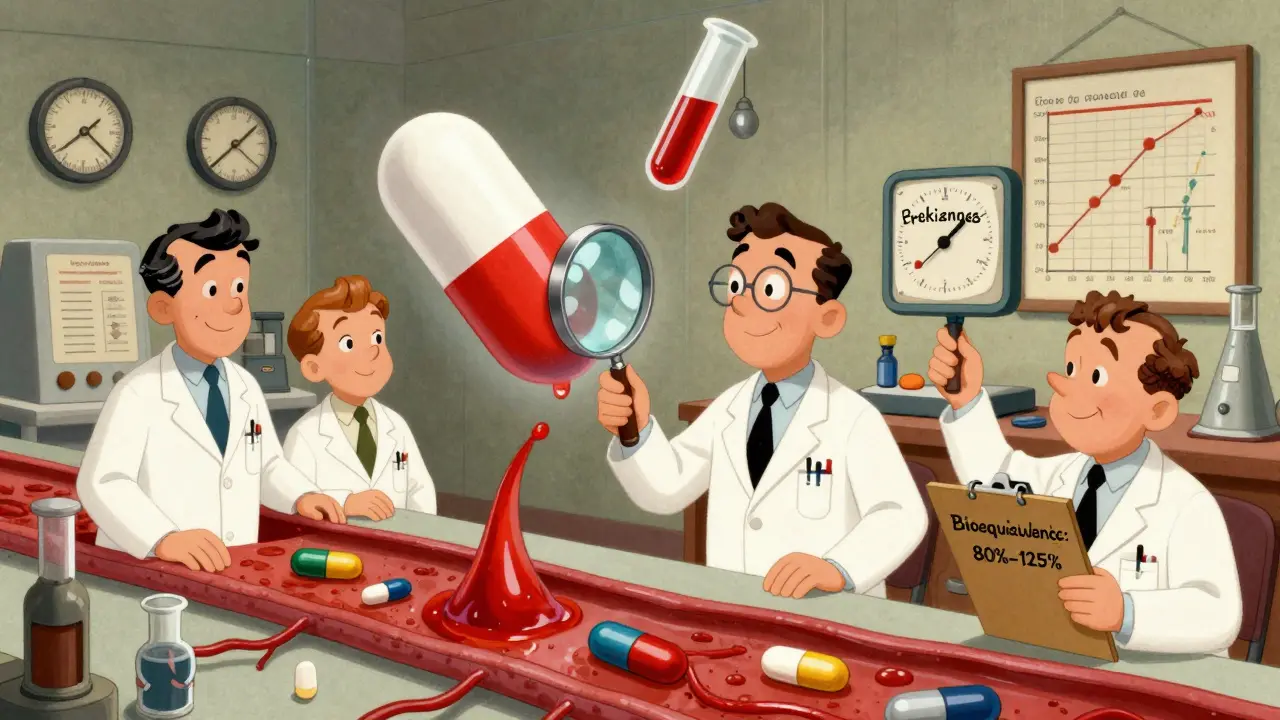
Step 3: Prove Bioequivalence
This is the heart of the ANDA. Bioequivalence means your drug gets into the bloodstream at the same rate and in the same amount as the brand. It’s not enough for the pill to look and taste the same. It has to work the same inside the body.
To prove this, you run a bioequivalence study. Usually, this involves 24 to 36 healthy volunteers. They take your generic version and the brand-name drug on different days, with a washout period in between. Blood samples are taken over 24-72 hours to measure how much of the drug enters the bloodstream and how fast.
The FDA requires the average amount of drug absorbed (AUC) and the peak concentration (Cmax) of your generic to fall within 80% to 125% of the brand’s values. That’s the legal bioequivalence range. If your numbers are outside that, your application gets rejected.
Some drugs are tricky. For example, extended-release pills, inhalers, or topical creams don’t behave like regular tablets. The FDA has special guidelines for these complex products. In 2023, about 15% of ANDAs were for these harder-to-copy drugs, and they take longer to review.
Step 4: Submit Chemistry, Manufacturing, and Controls (CMC) Data
Generic drugs aren’t just copies of pills-they’re copies of manufacturing processes. The FDA needs to know exactly how you make your drug, from raw materials to the final package.
Your CMC section includes:
- Details on the active pharmaceutical ingredient (API) source and purity
- Descriptions of manufacturing equipment and procedures
- Specifications for each step of production
- Stability data showing the drug won’t degrade over time
- Proof your facility follows Current Good Manufacturing Practices (cGMP)
These aren’t suggestions. They’re requirements. The FDA inspects every manufacturing site-whether it’s in the U.S., India, or China. If your facility fails inspection, your ANDA is delayed or denied. In 2023, 22% of ANDA deficiencies came from manufacturing issues.
Every batch must be consistent. One pill from batch #123 must perform exactly like batch #456. That’s why the FDA looks at your quality control data so closely.
Step 5: Labeling and Packaging
Your generic’s label must match the brand’s label in content-dosage instructions, warnings, side effects, contraindications. The only differences allowed are in the manufacturer’s name, logo, and inactive ingredients.
Why? Because patients and doctors need to know exactly what they’re taking. If the label says “take with food” and your version doesn’t, that’s a problem. If the warning about liver damage is missing, that’s a safety risk.
And packaging? It must protect the drug from moisture, light, and contamination. Blister packs, bottles, child-resistant caps-all must meet FDA standards. You can’t just slap a label on a random bottle.
Step 6: Submit in eCTD Format
You can’t email a PDF or send a binder. The FDA requires all ANDAs to be submitted in the electronic Common Technical Document (eCTD) format. This is a strict, standardized structure with five modules:
- Module 1: Administrative info (country-specific forms)
- Module 2: Summaries of quality, nonclinical, and clinical data
- Module 3: Chemistry and manufacturing details
- Module 4: Nonclinical study reports
- Module 5: Clinical study reports and labeling
Each section has exact formatting rules. If your file structure is wrong, the FDA won’t even accept your application. They’ll send a “not filed” letter. You’ve wasted months of work.
Most companies hire specialized regulatory consultants to handle eCTD submission. It’s not something you learn overnight. Regulatory affairs professionals typically spend 18-24 months training before they can handle an ANDA alone.
Step 7: FDA Review and Possible Requests
Once submitted, the FDA has 60 days to decide if your ANDA is “complete.” That means all required documents are there, in the right format. If not, they reject it before even starting the review.
If it’s complete, the clock starts. Under GDUFA IV (2023-2027), the FDA aims to review 90% of ANDAs within 10 months. The goal is to get the median review time down to 8 months.
During review, the FDA might send you an Information Request (IR). This isn’t a rejection-it’s a request for more data. Maybe they need clarification on your bioequivalence study, or they want additional stability data. You usually have 30 days to respond.
Some applications get a Complete Response Letter (CRL). That means major issues. Maybe your manufacturing site failed inspection, or your bioequivalence data was flawed. About 25% of ANDAs get a CRL on first review. Some companies spend millions and years trying to fix these issues.
Step 8: Facility Inspection
The FDA doesn’t just read papers-they show up. Most ANDAs trigger a pre-approval inspection of your manufacturing, packaging, or testing site. These inspections are unannounced and can last days.
Inspectors look for:
- Proper documentation of every batch
- Validated equipment
- Trained staff
- Controlled environments
- Accurate record-keeping
If they find serious violations-like falsified data or unsafe conditions-the ANDA is denied. No second chances.
Many companies now hire third-party auditors to prep for these inspections. It’s not optional anymore. One bad inspection can delay approval by over a year.

Step 9: Approval and Market Entry
If you pass review and inspection, the FDA approves your ANDA. You get a letter saying your generic drug is approved for sale in the U.S.
But here’s the catch: you can’t start selling right away. You have to wait until the brand-name drug’s patents and exclusivity periods expire. That’s why many generic companies file ANDAs years before the patent runs out-they’re just waiting for the green light.
There’s one big incentive: the first generic company to file an ANDA challenging a patent can get 180 days of market exclusivity. During that time, no other generics can enter. That’s why companies like Teva and Mylan race to be first. The first generic version of Humira made over $1.2 billion in sales during its exclusivity window.
Why Some Generic Drugs Fail
Not every ANDA gets approved. The most common reasons:
- 32%: Incomplete or unclear CMC data
- 28%: Flawed bioequivalence study design
- 22%: Manufacturing site issues
- 18%: Labeling mismatches
And it’s not just about mistakes. Some drugs are just harder to copy. Inhalers, injectables, and complex topical products require advanced science and testing. The FDA has a special initiative for these, but approval times are longer.
There are also quality concerns. A 2019 JAMA study found that while most generics are fine, some narrow therapeutic index drugs-like warfarin or levothyroxine-can show small differences in blood levels between brands. That’s why doctors sometimes stick with the brand for these.
What’s Next for Generic Drugs?
The FDA is pushing for faster reviews. Under GDUFA IV, they’re using AI to sort through documents faster, aiming to cut administrative time by 25% by 2025.
Biosimilars-generic versions of biologic drugs-are growing fast. In 2023, the FDA approved 7 biosimilars. By 2026, that number could hit 15 per year.
The goal? More competition. Lower prices. Better access. In 2023 alone, generic drugs saved the U.S. healthcare system $373 billion.
The ANDA process isn’t perfect. It’s complex, expensive, and sometimes slow. But it works. It’s the reason you can buy a month’s supply of metformin for $4 instead of $400. And that’s not just regulation-it’s public health.
How long does the FDA generic drug approval process take?
Under current FDA goals (GDUFA IV), the review timeline for a complete ANDA is 10 months. The median time for first-cycle approval is now around 8 months. However, this doesn’t include the time it takes to prepare the application, which can take 11-19 months. If the FDA issues a Complete Response Letter (CRL), the process can stretch to 2-3 years.
Can a generic drug be different from the brand-name version?
Yes, but only in non-critical ways. Generics must have the same active ingredient, strength, dosage form, and route of administration. They can use different inactive ingredients like fillers or dyes, as long as they’re safe. The pill might look different, but it must deliver the same amount of medicine into your bloodstream at the same rate. That’s what bioequivalence ensures.
Are generic drugs as safe as brand-name drugs?
Yes. The FDA requires generics to meet the same quality, safety, and effectiveness standards as brand-name drugs. They’re held to the same manufacturing rules (cGMP), and every facility is inspected. While rare cases of variation have been reported-especially with narrow therapeutic index drugs-over 99% of generics perform identically in clinical use. The FDA monitors adverse events for both brand and generic drugs equally.
Why do some generic drugs cost more than others?
Price differences come from competition, not quality. When only one generic is on the market, it may cost more. Once multiple generics enter, prices drop sharply-often by 90%. Some companies also produce higher-cost versions with special packaging or extended-release formulas. But the active ingredient and effectiveness are identical across all approved generics.
What happens if the FDA rejects my ANDA?
If the FDA rejects your ANDA, you’ll receive a Complete Response Letter (CRL) listing all deficiencies. You can respond with additional data, fix manufacturing issues, or resubmit the application. Many companies do this multiple times. Each CRL adds months or years to the timeline and can cost millions in extra testing. Some applications never get approved.
Do I need to be a U.S. company to get FDA generic approval?
No. Many generic drugs approved by the FDA are manufactured overseas-in India, China, or other countries. But all manufacturing sites, regardless of location, must pass FDA inspections and comply with U.S. cGMP standards. The FDA inspects foreign facilities just as rigorously as U.S. ones.
What to Do Next
If you’re a patient: trust your pharmacist. Generic drugs are safe, effective, and save you money. Ask if a generic is available for your prescription.
If you’re in the pharmaceutical industry: start with the Orange Book. Know your RLD. Hire experts. Don’t cut corners on CMC or bioequivalence. The FDA doesn’t play games.
If you’re a student or researcher: study the ANDA process. It’s one of the most successful examples of regulatory science balancing innovation, competition, and public health.
Generic drugs aren’t second-rate. They’re the backbone of affordable healthcare. And the FDA’s approval process? It’s the quiet engine that makes it all possible.