Imagine you’re prescribed a medication your doctor says you need - but your pharmacy says they can’t fill it. Not because it’s out of stock, but because your insurance hasn’t approved it yet. This is prior authorization, and it’s more common than most people realize. It’s not a glitch. It’s a system. And if you’re on prescription meds, especially expensive or specialty drugs, you’re likely to run into it.
What Is Prior Authorization?
Prior authorization - sometimes called pre-authorization or pre-certification - is when your health insurance company requires your doctor to get approval before they’ll pay for certain medications. It’s not about doubting your doctor. It’s about controlling costs and making sure the right drug is used for the right reason. Under Medicare Part D, this is officially called a coverage determination. The goal? To make sure you’re getting a drug that’s safe, effective, and cost-appropriate. Insurance companies use it to steer patients away from expensive brand-name drugs when a cheaper generic works just as well. They also use it to prevent risky combinations or off-label uses that aren’t proven to work. For example, if your doctor prescribes a $500-a-month brand-name drug for high blood pressure, but there’s a $20 generic version that’s equally effective, your insurer will likely require prior authorization before covering the expensive one. Your doctor must prove why the cheaper option won’t work for you.Which Medications Need Prior Authorization?
Not every drug needs approval. But certain types almost always do:- Brand-name drugs with generic alternatives - If a generic exists, insurers will push for it unless there’s a clear medical reason not to.
- High-cost medications - Think cancer treatments, rheumatoid arthritis biologics, or rare disease therapies that cost thousands per month.
- Drugs with strict usage rules - Some meds are only approved if you’ve tried and failed other treatments first. This is called “step therapy.”
- Drugs with safety risks - Medications that can cause liver damage, interact badly with other drugs, or have abuse potential (like certain painkillers or ADHD meds) often require extra scrutiny.
- Off-label uses - If your doctor prescribes a drug for a condition it’s not officially approved to treat (like using a diabetes drug for weight loss), they’ll need to provide strong evidence to justify it.
How Does the Process Work?
The process starts with your doctor. They’re the one who has to jump through the hoops - not you. Here’s how it typically unfolds:- Your doctor decides you need a medication that requires prior authorization.
- They check your insurance’s formulary (the list of covered drugs) to confirm the requirement.
- They fill out a form - either online, by fax, or through an electronic system - explaining why you need this specific drug. They include your diagnosis, medical history, and why other options won’t work.
- The form goes to your insurance company. They review it, sometimes with a pharmacist or medical director.
- They either approve, deny, or ask for more info.
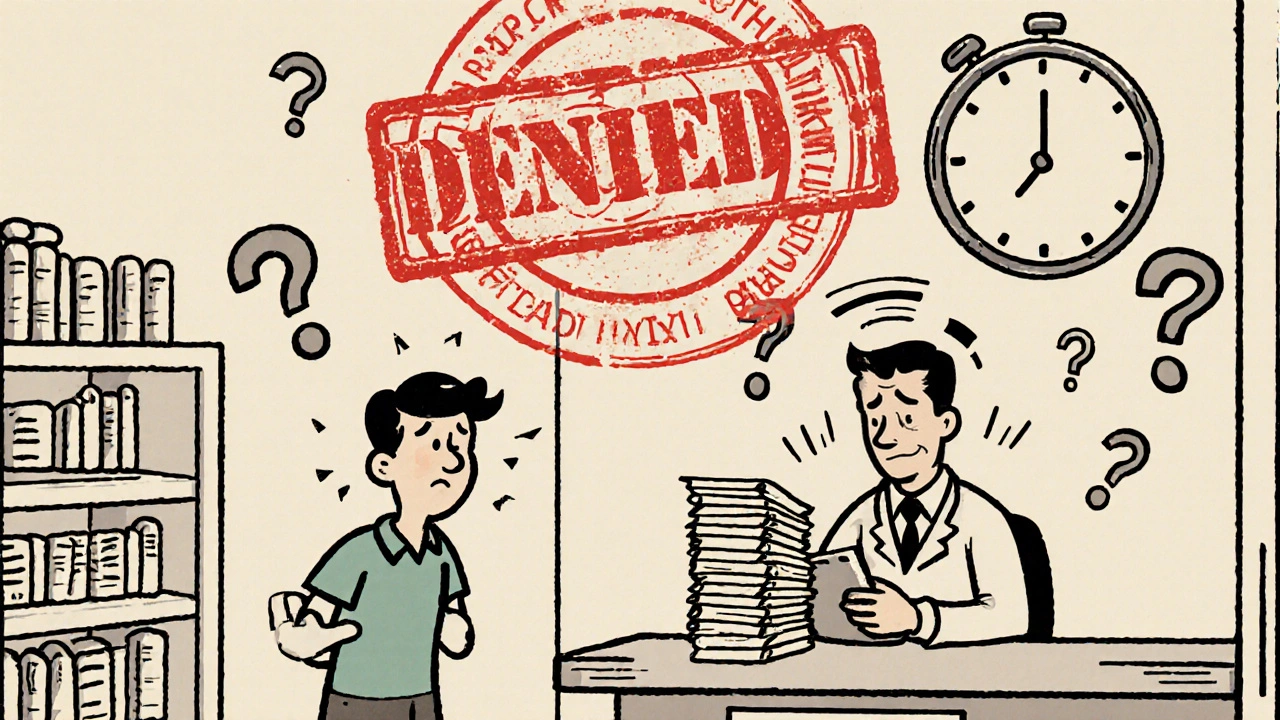
What Happens If It’s Denied?
Denials happen. Sometimes it’s because the paperwork was incomplete. Other times, the insurer just says, “We don’t think this is medically necessary.” You don’t have to accept that. You have the right to appeal. Your doctor can submit additional medical records, lab results, or even peer-reviewed studies to support your case. If the appeal fails, you can request an external review by an independent third party - especially if you’re on Medicare. In the meantime, you can:- Ask your doctor for an alternative drug that’s already covered.
- Pay out-of-pocket if the cost is manageable.
- Use a discount service like GoodRx to find lower cash prices.
- Pay upfront and submit a claim later - if you’re approved after the fact, you may get reimbursed.
How to Avoid Delays
You can’t control the insurance company - but you can help your doctor help you:- Ask early - Don’t wait until you’re at the pharmacy. Ask your doctor right after the prescription is written: “Does this need prior authorization?”
- Check your formulary - Log into your insurer’s website. Look up the drug name. If it says “Prior Auth Required,” you’ll know what’s coming.
- Use tools like Price Check My Rx - Blue Shield of California and others offer online tools that show you coverage status, copays, and cheaper alternatives.
- Keep records - Save the name of the drug, the date your doctor submitted the request, and who you spoke with at the insurance company.
- Follow up - If it’s been more than 3 business days and you haven’t heard anything, call your doctor’s office. Ask if the request was submitted and if they’ve heard back.
What About Emergencies?
If you’re having a medical emergency, prior authorization doesn’t apply. You can get the medication you need right away. Your insurance will cover it - as long as it’s medically necessary and you’re in-network. But here’s the catch: if you’re not in an emergency, but you’re in a hurry (like you’re running out of medication and your prior auth is still pending), you’re on your own. No insurance company will pay retroactively unless you’ve already been approved.
Why Does This System Exist?
Critics say prior authorization is bureaucratic, frustrating, and slows down care. And they’re not wrong. A 2023 survey by the American Medical Association found that physicians spend an average of 13 hours per week just dealing with prior auth requests. But insurers argue it’s necessary. Without it, costs would spiral. A single specialty drug can cost over $100,000 a year. If every patient got it without review, premiums would jump for everyone. The truth? It’s a balancing act. Insurance companies want to control spending. Patients want timely access. Doctors want to treat without red tape. Prior authorization tries to meet all three - and often fails.What Can You Do?
You’re not powerless in this system. Here’s what works:- Be proactive - Don’t assume your insurance will cover it. Ask before you leave the doctor’s office.
- Know your options - If your drug is denied, ask your doctor: “What else works?” There’s often another covered drug that’s just as effective.
- Use patient assistance programs - Many drug manufacturers offer free or discounted meds to people who can’t afford them. Ask your pharmacist or doctor.
- Appeal if needed - If you believe you’re being denied unfairly, fight back. Your doctor’s support is key.
Final Thoughts
Prior authorization isn’t perfect. It’s slow. It’s confusing. It can feel like a barrier to care. But it’s here to stay - and it’s not going away anytime soon. Your best move? Stay informed. Ask questions. Keep records. And don’t be afraid to push back when something doesn’t make sense. You’re not just a patient - you’re your own best advocate.What is prior authorization for medications?
Prior authorization is a process where your health insurance company requires your doctor to get approval before covering certain medications. It ensures the drug is medically necessary, safe, and cost-effective - often by checking if a cheaper alternative would work just as well.
How long does prior authorization take?
Approval can take anywhere from 24 hours to two weeks. Urgent cases may be processed faster. If your doctor submits incomplete paperwork, it can take longer. Always follow up if you haven’t heard back after 3 business days.
Can I get a medication without prior authorization?
Only if the drug doesn’t require it - or if you’re in an emergency. Otherwise, your pharmacy won’t be able to fill the prescription under your insurance plan. You can pay out-of-pocket, but you won’t get coverage until approval is granted.
What if my prior authorization is denied?
You can appeal the decision. Your doctor can submit more medical evidence, like test results or studies supporting the need for the drug. If the appeal is denied, you can request an external review by an independent reviewer - especially if you’re on Medicare.
Who starts the prior authorization process?
Your doctor or their office staff starts the process. They submit a request to your insurance company with details about your condition and why the medication is needed. You don’t have to do it yourself - but you should follow up to make sure it’s been sent.
Can I use GoodRx if my medication needs prior authorization?
Yes. GoodRx can show you cash prices for your medication, even if it requires prior authorization. If the cash price is lower than your copay after approval, you can pay out-of-pocket and skip the wait. You can also pay upfront and submit a claim later for reimbursement if approval comes through.
Do all insurance plans use prior authorization?
Most major insurers - including Medicare Part D, Blue Shield, Cigna, and UnitedHealthcare - use prior authorization for high-cost or specialty drugs. The exact list of drugs requiring it varies by plan, so always check your formulary before filling a prescription.
How do I check if my drug needs prior authorization?
Log into your insurance company’s website and look up the drug in their formulary or use their “Price Check My Rx” tool. You can also call customer service using the number on your insurance card. Your doctor’s office can also check for you.




9 Comments
Man, I’ve been through this with my dad’s arthritis meds-two weeks just to get a simple script approved. The pharmacy called me twice, the doctor’s office was silent, and we almost ran out. Prior auth isn’t just bureaucracy-it’s a waiting game where your health hangs in the balance.
EVERYTHING is controlled by Big Pharma and insurance oligarchs. They don’t care if you die waiting-they just want you to take the $5 generic that’s been clinically proven to cause kidney failure in 12% of cases. They’re hiding the real data. I’ve seen the leaked internal memos. You think this is about cost? Nah. It’s about profit. And they’re laughing all the way to the bank while you choke on your pills.
I just want to say… I totally get it. Like, I’ve been there. I’ve had to call my doctor’s office like, 5 times, and they’re always so nice, but the insurance system is just… broken. I mean, why does it take 10 forms just to get a drug that’s been on the market for 15 years?? It’s not like they’re inventing it. And then when it’s denied… ugh. I just cry a little inside. 😭
One must question the very epistemological foundations of pharmaceutical gatekeeping. The notion that a bureaucrat, armed with a formulary and zero clinical training, can adjudicate medical necessity… it’s a grotesque parody of rational healthcare. The system doesn’t care for outcomes-it cares for actuarial tables. How quaint. How tragic. How… 1998.
Prior authorization is a necessary safeguard in a system where drug costs are unsustainable. While delays are frustrating, they prevent reckless prescribing and protect patients from unnecessary financial and medical risk. The burden on providers is real, but the alternative-unrestricted access to $10,000/month drugs-is worse for everyone.
you know what's wild? this whole thing feels like we're all just trying to survive a machine that was never built for humans. doctors write scripts, pharmacies wait, patients suffer. nobody wins. but we keep going. maybe that's the real medicine. just showing up.
From a clinical pharmacology standpoint, prior authorization aligns with therapeutic guidelines and formulary stewardship. Step therapy protocols are evidence-based interventions designed to optimize cost-effectiveness while maintaining non-inferior efficacy. The real issue lies in the administrative latency-manual workflows, fragmented EHR integrations, and lack of real-time adjudication. We need AI-driven prior auth engines with HL7/FHIR interoperability, not more fax machines.
we’re all just pawns in a game where the board was drawn by lawyers and the pieces are people’s lives. 🤡💊 the system isn’t broken-it’s working exactly as intended. and honestly? i’m not mad. i’m just… disappointed. like, i thought we evolved past this. turns out we just got better at pretending.
My uncle died waiting for his cancer drug to get approved. They said ‘it’s just paperwork.’ JUST PAPERWORK?!?!? You want to talk about American healthcare? This is it. This is the face of greed. I don’t care if it saves money-I care that people are dying because some suit in a cubicle thinks a $20 pill is ‘good enough.’
Write a comment