Urticaria - commonly called hives - isn’t just a rash. It’s a sudden, itchy, raised welt that can appear anywhere on your skin, vanish in hours, and come back the next day. For some, it’s a one-time annoyance. For others, it’s a daily battle that disrupts sleep, work, and life. If you’ve ever woken up covered in angry red bumps that burn and itch, you know how frustrating it can be. The good news? Most cases respond well to simple treatments. The tricky part? Figuring out what’s causing it - and when to go beyond the pharmacy shelf.
What Exactly Are Hives?
Hives are not an infection. They’re not contagious. They’re your body’s overreaction. When something triggers your immune system - even if it’s not truly harmful - your mast cells release histamine. That chemical makes tiny blood vessels leak fluid into your skin, creating those raised, red, itchy welts. They can be as small as a pinhead or as big as a dinner plate. They often look like nettle stings, which is why hives are sometimes called nettle rash. The key thing to remember: hives that last less than 24 hours in the same spot are usually acute. If they keep coming back for more than six weeks, it’s chronic. About 20% of people will get hives at least once in their life. Women are 1.5 to 2 times more likely to experience them than men, especially between ages 30 and 50.What Triggers Hives? Not Always What You Think
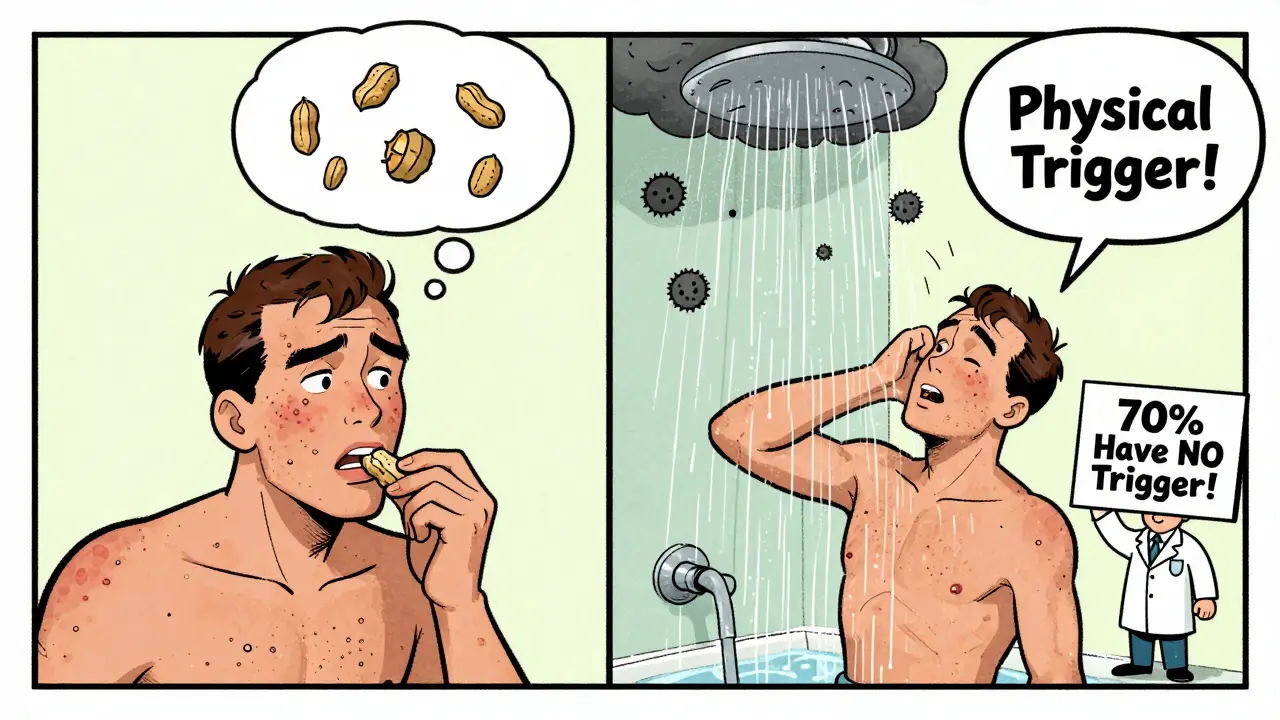
People assume food allergies are the main cause - peanuts, shellfish, eggs. And yes, those can trigger hives. But in chronic cases, food is rarely the culprit. In fact, 70 to 80% of chronic spontaneous urticaria has no clear trigger at all. That’s frustrating, but normal. Common triggers include:- Physical stimuli: Pressure from tight clothes, heat, cold, sweat, or sunlight. If you get hives after a hot shower or wearing a backpack, you might have physical urticaria.
- Medications: NSAIDs like ibuprofen or aspirin, antibiotics like penicillin, and even some blood pressure meds can cause reactions.
- Infections: Viral infections like colds or hepatitis can spark hives, especially in kids.
- Stress: Emotional stress doesn’t cause hives directly, but it can make them worse or trigger flare-ups in people already prone to them.
- Autoimmune issues: In about 30 to 40% of chronic cases, your immune system mistakenly attacks your own mast cells. This isn’t an allergy - it’s your body turning on itself.
Antihistamines: The First Line of Defense
If you have hives, the first thing you should try is an antihistamine. These drugs block histamine from binding to receptors in your skin, which stops the itching and swelling. There are two types:- First-generation: Diphenhydramine (Benadryl), chlorpheniramine. These work fast but make most people drowsy - up to 70% of users feel sleepy. They’re okay for occasional use at night, but not for daily long-term management.
- Second-generation: Cetirizine (Zyrtec), loratadine (Claritin), fexofenadine (Allegra). These are non-sedating for most people. They last 24 hours and are the gold standard for daily use.
When Antihistamines Aren’t Enough
If you’re on the highest safe dose of antihistamines for four to six weeks and still breaking out, it’s time to talk to an allergist. There are other options - but they’re not all created equal.- Omalizumab (Xolair): This is an injectable biologic approved since 2014. It targets IgE, the antibody involved in allergic reactions. In clinical trials, 65% of patients who didn’t respond to antihistamines saw complete or near-complete relief within 4 to 12 weeks. It’s given as a shot every four weeks. Cost? Around $1,500 per dose in the U.S. Many insurance plans cover it for chronic hives, but prior authorization is often required.
- Dupilumab (Dupixent): Approved for chronic hives in September 2023. Originally for eczema and asthma, it showed 55% of patients had complete symptom control in trials - compared to just 15% on placebo. It’s also an injection, given every two weeks.
- Remibrutinib: The newest player. Approved in January 2024, it’s the first oral tyrosine kinase inhibitor for hives. In trials, 45% of patients had complete symptom control with 50mg twice daily. The big advantage? It’s a pill. No injections. Patient adherence was 85% compared to 70% for injections.
- Corticosteroids (like prednisone): These work fast - sometimes in hours. But they’re dangerous if used longer than 3 to 5 days. Side effects include high blood sugar (35% of users), insomnia (25%), mood swings (20%), and weight gain. They’re a bridge, not a solution.
- Cyclosporine: An immunosuppressant used off-label. Works for about 60% of tough cases, but carries risks: kidney damage in 15-20% of users, high blood pressure in 25-30%. Reserved for when nothing else works.
What Works Best? A Quick Comparison
| Treatment | Form | Time to Effect | Response Rate | Key Risks |
|---|---|---|---|---|
| Second-gen antihistamines (e.g., cetirizine) | Oral | 1-4 hours | 50-60% | Headache, dry mouth |
| High-dose antihistamines (up to 4x) | Oral | 1-4 hours | 70-80% | Still minimal if within limits |
| Omalizumab (Xolair) | Injection | 2-8 weeks | 65% | Injection site reactions, rare anaphylaxis |
| Dupilumab (Dupixent) | Injection | 2-6 weeks | 55% | Conjunctivitis, sore throat |
| Remibrutinib | Oral | 2-6 weeks | 45% | Headache, nausea |
| Prednisone | Oral | Hours | 80% | High blood sugar, insomnia, mood changes |
Real People, Real Experiences
Online communities like Reddit’s r/ChronicHives have over 15,000 members. A 2023 survey of 1,245 people there found:- 68% said hives disrupted their sleep - many waking 2-3 times a night.
- 42% avoided social events because they feared breaking out.
- Those on omalizumab reported 72% satisfaction - many saying they’d “gotten their life back.”
- Those on prednisone said: “I felt like a different person - anxious, wired, unable to sleep.”
How to Get Started
If you’re dealing with hives, here’s what to do:- Start with an OTC antihistamine. Pick one non-drowsy one - cetirizine or fexofenadine. Take 10mg daily for at least 7 days. Don’t skip doses.
- Keep a symptom diary. Note what you ate, what you did, how you felt, and when the hives appeared. Don’t overthink it - just track for two weeks.
- If no improvement after 14 days, double the dose. Go to 20mg of cetirizine. Many doctors still don’t know this is safe. But the guidelines say you can go up to 4x the standard dose.
- If you’re still breaking out after 4-6 weeks on high-dose antihistamines, see an allergist. Don’t wait. Chronic hives aren’t just a skin issue - they’re linked to anxiety, depression, and reduced quality of life.

What You Shouldn’t Do
- Don’t assume it’s food. Unless you get hives within minutes of eating something specific, it’s probably not the culprit.
- Don’t rely on steroids long-term. They’re a band-aid, not a cure.
- Don’t ignore mental health. One in five chronic hives patients develops depression or anxiety. It’s not “all in your head.” It’s a real response to constant physical stress.
- Don’t stop taking your meds just because you feel better. Hives can return if you stop too soon.
The Future of Hives Treatment
The field is moving fast. In 2024, remibrutinib became the first oral drug approved specifically for chronic hives. More are coming. Linzagolix, expected for FDA review in late 2024, showed 52% complete response in early trials. Experts predict that within five years, genetic testing will help match patients to the right antihistamine - avoiding trial and error. Digital tools are already helping: apps like Urticaria Tracker let users log flare-ups, weather, stress, and diet, and share data with doctors. But access remains unequal. In high-income countries, 85% of chronic hives patients can get biologics. In low-income ones, it’s 30%. That’s not just a medical gap - it’s a justice issue.Final Thoughts
Hives are more common than you think. They’re not dangerous in most cases - but they’re exhausting. Antihistamines are the foundation. Most people don’t need fancy drugs. But if they’re not working, don’t accept it. There are better options now than ever before. The key is persistence, tracking, and knowing when to ask for help. You don’t have to live with daily itching. There’s a path forward - and you’re not alone.Can stress cause hives?
Stress doesn’t directly cause hives, but it can trigger flare-ups in people who already have chronic urticaria. When you’re under stress, your body releases chemicals that can activate mast cells - the same cells that cause hives. Many patients report worse outbreaks during high-stress periods like work deadlines, family crises, or sleep loss. Managing stress through sleep, exercise, or therapy won’t cure hives, but it can reduce how often they flare.
Are hives contagious?
No, hives are not contagious. You can’t catch them from someone else. They’re caused by your own immune system reacting to a trigger - whether it’s a medication, physical pressure, or an internal autoimmune process. Touching someone with hives won’t give you hives.
Why do hives come and go so fast?
Hives move because histamine causes temporary fluid leaks in the skin. Each welt lasts less than 24 hours in one spot because the fluid gets reabsorbed and new ones form elsewhere. If a welt lasts longer than 24 hours in the same place, it’s likely not hives - it could be another condition like vasculitis, which needs different treatment.
Can I take two different antihistamines at once?
Yes, under medical supervision. Some patients combine a non-sedating antihistamine during the day (like fexofenadine) with a sedating one at night (like hydroxyzine) to get 24-hour relief. This can improve sleep and reduce itching. But don’t do this on your own - mixing meds can increase side effects. Always talk to your doctor first.
Is there a cure for chronic hives?
There’s no guaranteed cure, but there is control. Most people with chronic hives find relief with medication. In about half of cases, symptoms fade on their own within 1 to 5 years. For others, long-term treatment with biologics like omalizumab or remibrutinib keeps symptoms away. The goal isn’t always to cure - it’s to live without daily itching and disruption.
Should I get allergy tested for hives?
For acute hives - yes, especially if you suspect food or insect stings. For chronic hives, allergy testing is rarely helpful. Most chronic cases aren’t triggered by allergies. Instead, doctors focus on ruling out autoimmune causes or physical triggers like pressure or heat. Blood tests for autoimmune markers are more useful than skin prick tests in chronic cases.
Can I outgrow chronic hives?
Many people do. About 50% of chronic hives cases resolve within a year, and 80% within five years. But it’s unpredictable. Some people have it for decades. The good news is that even if it doesn’t go away, modern treatments can control it almost completely. You don’t have to wait for it to “go away” to feel better.





13 Comments
Been dealing with chronic hives for 3 years. Cetirizine 20mg daily saved my life. No more sleepless nights. No more avoiding social events. I used to think it was food but nope. Turns out it was just my immune system being a drama queen. High-dose antihistamines are underused. Doctors act like you’re going to die if you take more than 10mg. Lol. Just tell them the guidelines. They’ll shut up.
So glad this post exists. I’ve been telling people for years that hives aren’t just ‘allergies’ - they’re a whole system thing. Especially when it’s chronic. Stress doesn’t cause it, but it’s like pouring gasoline on a fire you didn’t even know was lit. I started tracking my sleep and stress levels and noticed patterns. No magic cure, but way less flares now.
In India, we have this weird thing where people think hives are caused by ‘bad blood’ or ‘heat in the body’ - so they take turmeric, neem, or even fasting for days. Meanwhile, the real solution? A 10mg pill you can buy at any pharmacy. I’ve seen friends waste months on Ayurvedic ‘detoxes’ while their hives got worse. Not saying traditional medicine is bad - but when science has a clear, safe, cheap fix, why gamble? Also, omalizumab is a game-changer. If your insurance covers it - fight for it.
It is imperative to underscore that the utilization of antihistamines at quadruple the standard dosage is not only pharmacologically sound, but also empirically validated by the latest clinical guidelines issued by the American Academy of Allergy, Asthma & Immunology in 2023. Furthermore, the assertion that stress is a trigger - rather than a causative agent - is both scientifically accurate and clinically significant. One must not conflate correlation with causation, especially in autoimmune conditions such as chronic urticaria.
Everyone’s just taking pills and ignoring the real problem: your soul is broken. Hives are your body screaming because you’re living wrong. You’re on your phone too much. You don’t breathe. You eat garbage. You’re scared of silence. Stop blaming your immune system. Fix your life. Then the hives will go. Simple.
Did you even read the part about prednisone? It says it causes insomnia, high blood sugar, mood swings. And you’re still recommending it? That’s like saying ‘if your car is on fire, just pour gasoline on it - it’ll stop burning faster.’ This article is dangerously misleading. You’re normalizing steroid abuse.
I’ve been on Xolair for 8 months. My life is different. I can wear a dress again. I can hug my niece without hiding my arms. I cried the first time I saw my skin clear for a whole week. If you’re still on antihistamines and not improving - don’t wait. Go see an allergist. It’s not a last resort. It’s the next step.
High-dose antihistamines work. No debate. I took 30mg of cetirizine for 6 months. Zero hives. No side effects. My doctor was shocked. But I read the guidelines. You should too. Stop letting outdated practices hold you back. This isn’t 2010 anymore. We know better now.
Just wanted to say - if you’re reading this and you’re scared or alone - you’re not. I used to hide in long sleeves in summer. Now I wear tank tops. It took time. It took meds. It took not giving up. You got this.
Remibrutinib is the future. Oral. No needles. 45% complete response. That’s huge. I’m waiting for my prescription. My dermatologist says it’s not covered yet - but I’m appealing. If you’re in the US and have insurance - push for it. It’s not just about hives. It’s about being able to live without constant itching.
They’re hiding something. Why is this only approved in the US and EU? Why is it so expensive? Big Pharma doesn’t want you cured. They want you on pills forever. I bet the real cure is in herbal medicine or water therapy - but they ban it because it doesn’t make money. Look at the numbers - 80% of chronic cases resolve on their own. They just want you to pay for injections.
Back home in Punjab, my grandma used to say hives meant someone was jealous of you. I thought she was crazy - until I noticed mine got worse during family fights. Stress is real. Not because it’s ‘in your head’ - because your body feels it. I started yoga and journaling. Not a cure. But it helped. And now I take my 20mg cetirizine with my morning chai. Simple. No drama.
Stop telling people to ‘just take more antihistamines.’ What about the ones who still break out? You’re ignoring the real issue - autoimmune dysfunction. If you’re not addressing the root cause, you’re just masking symptoms. I’m on dupilumab now. It’s not perfect - but it’s the first thing that actually worked after 5 years of failed treatments. Don’t settle for ‘better.’ Fight for ‘gone.’
Write a comment