When your heart stops getting enough blood, it doesn’t scream. It whispers. And too often, people ignore the whisper until it’s too late. A heart attack isn’t always the dramatic collapse you see in movies. More often, it’s a dull pressure in your chest, a strange ache in your jaw, or sudden exhaustion that won’t go away. In the UK, heart disease kills more people than cancer. But here’s the good news: if you know the signs and act fast, you can cut your chance of dying by half.
What a Heart Attack Really Feels Like
The classic image of a heart attack-clutching your chest, collapsing to the floor-is real, but it’s not the whole story. The most common sign is discomfort in the center of your chest. It’s not always sharp pain. It’s more like a heavy weight, a squeezing sensation, or a burning that lasts longer than a few minutes. It might come and go. You might think it’s indigestion, especially if it’s after a big meal.
But here’s what most people don’t know: the pain doesn’t always stay in your chest. About two in three people feel it elsewhere-your left arm, your back, your neck, your jaw, or even your stomach. I’ve spoken to women who thought they had the flu because their only symptom was nausea. Others woke up with jaw pain so bad they went to the dentist, only to find out their heart was in trouble.
Shortness of breath is another major red flag. You might feel winded climbing stairs, or suddenly gasping for air while sitting still. It can happen with chest pain-or without any chest pain at all. Cold sweats, dizziness, and a racing or fluttering heartbeat are also common. If you break out in a cold sweat for no reason, especially if you’re not hot or exercising, that’s your body’s alarm system.
Women Don’t Have the Same Symptoms as Men
Men are more likely to have the textbook chest pain. But women? They often don’t. Only about 64% of women feel chest discomfort during a heart attack. That’s nearly 1 in 3 who won’t have the warning sign most people are taught to look for.
Women are far more likely to have symptoms like:
- Unexplained fatigue-so tired you can’t get out of bed
- Nausea or vomiting
- Back or jaw pain without chest pain
- Overwhelming anxiety or a sense of doom
- Upset stomach that feels like heartburn
One woman I read about thought she had acid reflux for three days. She took antacids. She rested. She didn’t call an ambulance. By the time she got to the hospital, half her heart muscle was already dead. That’s not rare. Women are 50% more likely to be sent home from the ER with a heart attack misdiagnosed as anxiety or indigestion. And that delay kills.
Age makes it worse. If you’re over 75, you might have a “silent” heart attack-no chest pain at all. Just weakness, confusion, or trouble breathing. Many older people think it’s just getting older. It’s not.
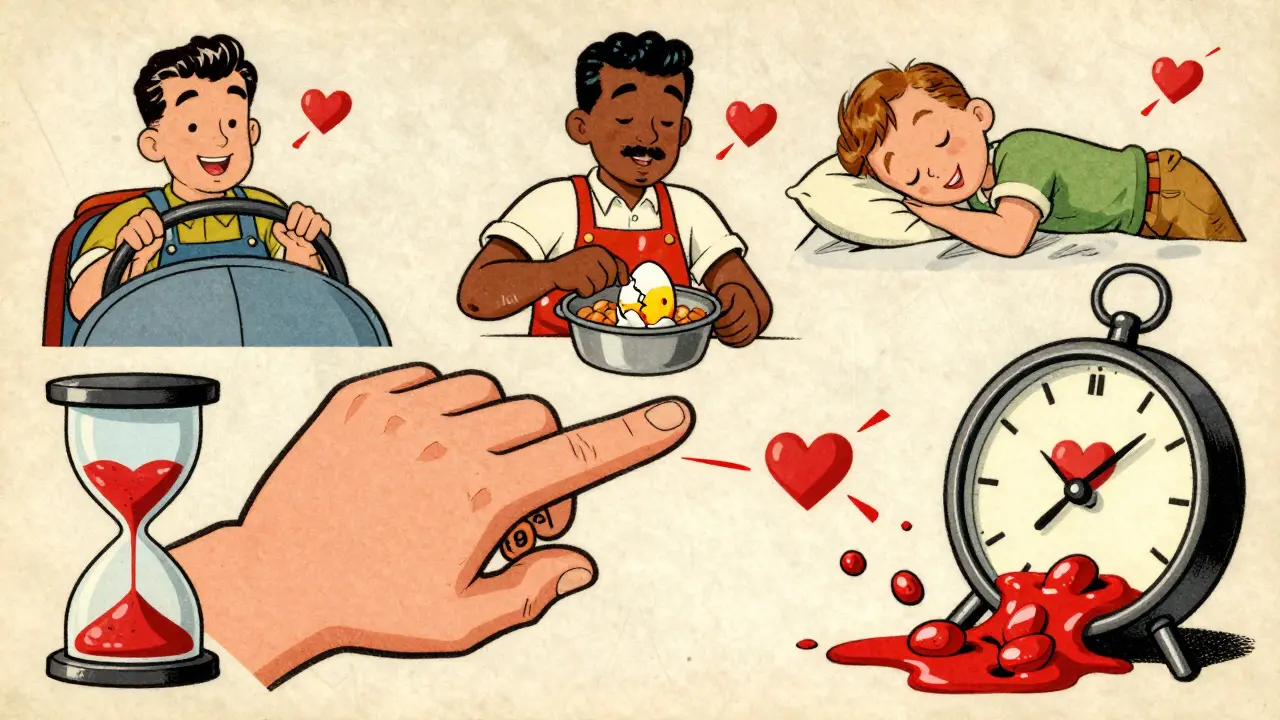
Warning Signs Can Start Weeks Before
Heart attacks don’t always come out of nowhere. Many people report unusual symptoms weeks or even a month before the event. These aren’t dramatic. They’re subtle:
- Unexplained tiredness that won’t go away
- Palpitations-your heart skipping or fluttering for no reason
- Swelling in your legs or ankles
- Difficulty sleeping
- Feeling off, but you can’t say why
These aren’t “maybe” signs. They’re early warnings. If you’ve been feeling off for more than a few days and nothing seems to help, don’t brush it off. Get checked.
What to Do the Moment You Suspect a Heart Attack
Time is muscle. Every minute you wait, 1.5 million heart cells die. The goal is to get help within 90 minutes of symptoms starting. But the average person waits three hours.
Here’s what you do:
- Call 999 immediately. Don’t call a friend. Don’t drive yourself. Ambulances have paramedics who can start treatment on the way. They can give you oxygen, aspirin, and monitor your heart before you even reach the hospital. You’ll get there 25% faster than if you drive.
- Chew one 300mg aspirin. Only if you’re not allergic and your doctor hasn’t told you to avoid it. Aspirin thins the blood and can help reduce damage. Don’t swallow it whole-chew it so it works faster.
- Stay calm and sit down. Don’t panic. Don’t try to walk around. Lie down if you can. Keep breathing slowly.
- Don’t wait to see if it gets better. If symptoms last more than 5 minutes, call 999. Even if they go away. Heart attacks can come and go.
People delay because they’re scared of being wrong. They don’t want to look silly. But here’s the truth: it’s better to be wrong five times than to be right once and die. Emergency staff see this every day. They’d rather you call and it’s nothing than wait and find out it was everything.
Why Delaying Kills
Studies show that people who wait more than two hours before calling for help have a 50% higher chance of dying. Women, older adults, and people with diabetes are especially at risk because their symptoms are less obvious. And if you’re in a rural area, emergency response times are longer-up to 27% longer than in cities. That’s why knowing the signs and acting fast isn’t just helpful-it’s life-saving.
One man in Exeter waited six hours because he thought it was just a bad stomach bug. He was 48. He survived, but his heart was permanently damaged. He told his story in a local support group: “I thought I was being dramatic. Turns out, I was just being dead wrong.”
What Helps: Training, Tech, and Awareness
Communities that teach CPR and heart attack awareness have 28% higher survival rates after cardiac arrests. The British Heart Foundation runs free training sessions across the UK. You don’t need to be a doctor. Just knowing how to do chest compressions can keep someone alive until help arrives.
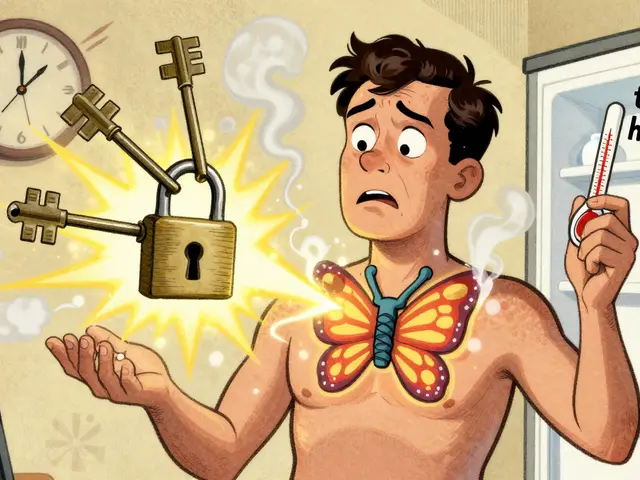
Technology is catching up too. Some smartwatches now detect irregular heart rhythms that can signal trouble before a heart attack. And new AI tools can spot early signs on an ECG-sometimes 30 minutes before symptoms start. But none of that matters if you don’t know what to look for.
Heart attack awareness campaigns like Go Red for Women have reached millions. But awareness isn’t enough. Action is.
Final Thought: Don’t Wait for the Scream
Heart attacks don’t wait for perfect conditions. They don’t wait for you to have time, or for your doctor to be available, or for you to feel “sure enough.” They happen when you’re cooking dinner, driving home, or lying in bed.
If you feel something off-pressure, pain, shortness of breath, nausea, fatigue-don’t rationalize it. Don’t Google it. Don’t wait to see if it passes. Call 999. Say, “I think I’m having a heart attack.” Even if you’re wrong, you’ve done the right thing.
And if you’re with someone who’s showing signs-don’t ask if they’re sure. Don’t wait for them to decide. Call 999 yourself. You might just save their life.



12 Comments
Why are we still talking about this like it's 2005? Everyone knows chest pain means heart attack. The real problem is people who wait because they're too lazy to call 999. You think your stomach bug is serious? Go to the ER and get a CT. Stop being a coward.
While the article presents valuable clinical insights, it is imperative to acknowledge the systemic disparities in healthcare access that render such guidelines inequitable across socioeconomic strata. In many regions, emergency services remain inaccessible, rendering the advice to 'call 999' functionally irrelevant.
So let me get this straight - we're supposed to panic because a 75-year-old feels tired? Cool. I'm just glad I'm not the one who has to explain to my grandma why her 'just being old' is actually a cardiac emergency. Also, aspirin? Chew it? Like a gummy bear? I'm not chewing anything unless it's chocolate.
Chew aspirin. Not swallow. Got it. Next you'll tell me to rub garlic on my chest.
Okay but what if you're just really stressed? Or ate too much pizza? Or it's just your period? I had jaw pain for three days once and it turned out I was just mad at my boss. Also, why is everyone assuming women are dumb? We know our bodies. Maybe we just don't want to be scared into a hospital for no reason.
Cardiac pathology simplified for the masses. How quaint. The real issue is the commodification of preventative medicine by the NHS and its corporate partners. You're not saving lives-you're selling fear.
I'm a nurse and I see this every shift. People come in saying 'I think I'm fine' and then collapse five minutes later. Please. If you're even 10% unsure, call 999. I don't care if you're 22 and in the gym. If your heart feels weird, it's not 'just anxiety'. It's not 'just gas'. It's your body screaming. And I've seen too many people die because they didn't listen. You don't have to be a doctor. You just have to be brave enough to call. And if you're with someone who's off? Don't wait for them to say 'I'm okay'. Call it. Even if they yell at you. You'll thank yourself later.
This is such an important post. I lost my dad to a silent heart attack. He thought he was just tired. He was 68. No chest pain. Just… gone. I wish someone had told him what you just said. I’m sharing this with my whole family. Please, if you’re reading this, don’t wait. Even if it’s nothing, you’ll be glad you did.
Call 999? Lol. In rural Ohio, the ambulance takes 45 mins. Meanwhile, I’m sitting here with my dad who’s sweating bullets and I’m Googling 'is this a heart attack or just a panic attack'. And yeah I mispelled mispelling. I’m not a robot. And no I don’t care if you think I’m uneducated. I just want my pops to live.
STOP GASLIGHTING PEOPLE. Women don't have 'different' symptoms - you're just bad at diagnosing them. And don't give me that 'call 999' nonsense. The ER will just give you a Xanax and send you home. I've been there. You're not saving lives - you're just selling a narrative. 🤡
I’ve worked on the ambulance for 18 years. Seen it all. The ones who call right away? They walk out. The ones who wait? They come in on a stretcher, or not at all. I’ve held the hand of a woman who thought she had the flu. She was 52. Her husband didn’t believe her until she turned blue. Don’t be that guy. Don’t be that wife. Call it. Even if it’s just a whisper. We’ll hear it.
This is such a powerful message. I’ve shared this with my book club, my church group, and my neighbors. We’re organizing a free CPR workshop next month. If you’re reading this and you’re scared - you’re not alone. But you’re also not powerless. Knowledge is the first step. Action is the second. And together, we can turn whispers into shouts. Let’s save lives, one call at a time. 💪❤️
Write a comment