Why generic prescribing isn’t just about saving money
When you write a prescription, you’re not just choosing a drug-you’re choosing a system. Generic prescribing means writing the International Non-proprietary Name (INN) of a medication, not the brand name. That’s it. No fancy jargon. Just the active ingredient: atorvastatin, not Lipitor; omeprazole, not Losec. In the UK, the NHS has pushed this for decades, and today, nearly 90% of prescriptions are written this way. But why? And when should you make an exception?
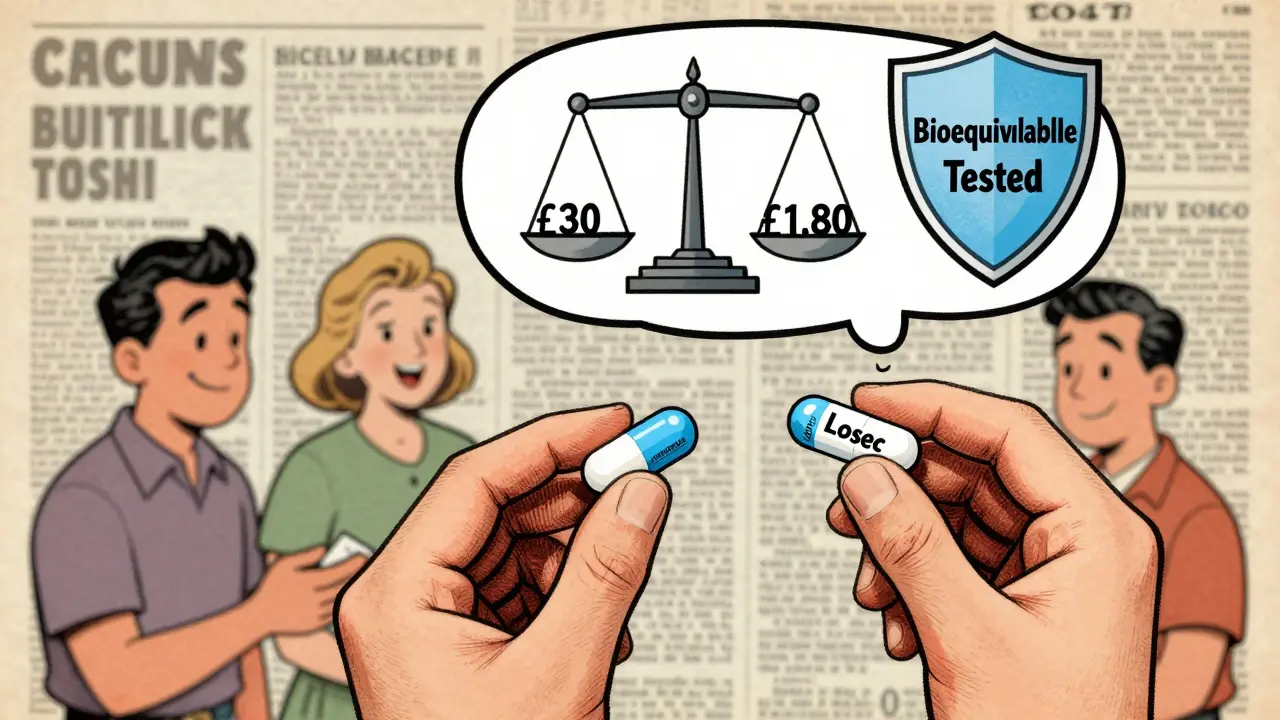
The numbers speak for themselves. A generic version of atorvastatin costs around £2.50 a month. The branded version? £30. Omeprazole? £1.80 versus £15. That’s not a small difference-it’s an 80-85% drop in cost. Multiply that across millions of prescriptions, and you’re talking about £1.3 billion saved every year in the NHS alone. That’s not just budgeting. That’s freeing up resources for more patients, faster appointments, better care.
But here’s what most people don’t realize: it’s not just about cost. It’s about safety. When you use generic names, you cut down on medication errors. Imagine a patient on ten different drugs. Each one has five brand names across different countries. Now imagine a nurse or pharmacist mixing them up. With generic prescribing, there’s only one name per active ingredient. That cuts errors by about half, according to the Institute for Safe Medication Practices. That’s not theoretical. That’s real people avoiding hospital visits because someone didn’t confuse Metoprolol Tartrate with Lopressor and Toprol-XL.
When generic prescribing works-every time
For the vast majority of medications, generics are identical in effect. The rules are strict. In the UK, the MHRA and the European Medicines Agency require generics to prove they deliver the same amount of active ingredient into the bloodstream at the same rate as the brand. That’s bioequivalence. The standard? 80-125% of the original drug’s absorption. That’s not a wide range-it’s tight. And it’s tested with real people, not just lab models.
Take antidepressants. Sertraline is a common one. A 2021 study of 3,200 patients found that when doctors explained why they were switching to generic sertraline, patient satisfaction jumped from 67% to 89%. Why? Because fear isn’t about the drug-it’s about the unknown. Patients worry generics are weaker, less reliable. But the data says otherwise. The same active ingredient. Same dose. Same manufacturer standards. The only difference? The colour of the pill, or the filler inside. And those fillers? They’re regulated too.
And adherence? It goes up. A JAMA study showed that when patients pay less out of pocket, they take their meds more consistently. That means fewer heart attacks, fewer hospital stays, fewer complications. For someone on a fixed income, saving £12 a month on blood pressure meds isn’t a luxury-it’s the difference between taking it daily or skipping doses to make it last.
The exceptions: when brand matters
Not all drugs are created equal. There are three categories where brand-name prescribing isn’t just recommended-it’s necessary.
Category 1: Narrow therapeutic index drugs. These are the ones where a tiny change in blood level can cause harm-or death. Think warfarin. Too little? Blood clots. Too much? Internal bleeding. Even small differences between generic batches can shift INR levels. The same goes for levothyroxine, phenytoin, carbamazepine, and digoxin. The British National Formulary (BNF) is clear: prescribe these by brand. Not because generics are unsafe-but because the margin for error is razor-thin. Switching brands without monitoring? Risky.
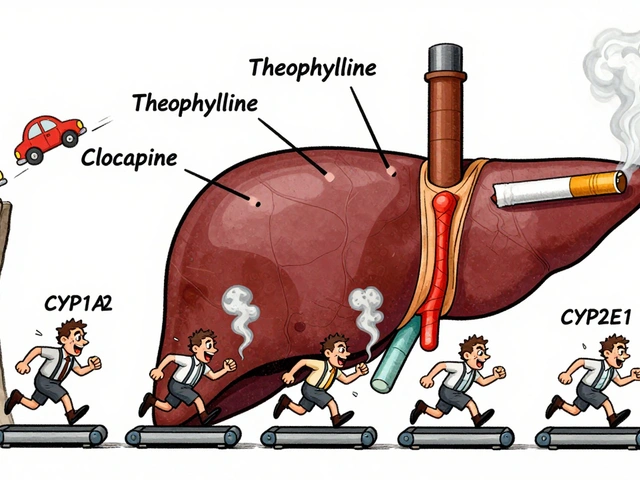
Category 2: Modified-release formulations. These are designed to release the drug slowly over hours. A generic version might look the same, but if the coating or matrix is slightly different, the drug can release too fast or too slow. The Royal Pharmaceutical Society reports that 41% of pharmacists have seen issues with generic versions of theophylline or certain painkillers. The patient doesn’t feel the difference right away-but over time, it adds up. Seizures. Chest pain. Unstable diabetes. These aren’t rare.
Category 3: Biologics. These are complex proteins made from living cells. Think insulin, rheumatoid arthritis drugs, cancer treatments. Biosimilars aren’t generics. They’re similar, but not identical. The MHRA says: prescribe by brand. Why? Because switching between biosimilars and originators can trigger immune reactions. No one wants a patient developing antibodies to their own medication. That’s not speculation. That’s documented in clinical reports.
How to make the switch without losing trust
Patients don’t resist generics because they’re irrational. They’ve heard stories. A relative had a bad reaction. A friend said their headache got worse. A Reddit thread from February 2023 had 147 doctors sharing their experiences. One wrote: “95% of my patients do fine. The 5%? They’re the ones on antiepileptics or thyroid meds. That’s where you listen.”
So how do you handle it? Use the “Explain, Empower, Engage” method. Don’t just say, “We’re switching to generic.” Say this:
- “This medicine has the same active ingredient as your old one-exactly the same.”
- “It’s been tested to work the same way in your body.”
- “It’s cheaper, so you’ll save about £12 a month. And there’s no reason to expect any change in how you feel.”
That last part is key. The nocebo effect-where people feel worse because they believe something will make them worse-is real. Studies show it accounts for nearly 30% of reported side effects after switching to generics. If you don’t explain it, the patient’s brain fills in the blanks with fear.
And if they’re still unsure? Offer to monitor. “Let’s check your blood pressure in two weeks,” or “We’ll do a thyroid test next month.” That’s not just good medicine-it’s good communication.
What the system expects from you
The NHS doesn’t just want you to prescribe generically. It wants you to do it right. The 2023 Generic Prescribing Toolkit gives a clear four-step path:
- Audit your current prescribing using the Prescribing Analytics Dashboard. See where you’re still using brands unnecessarily.
- Learn the three exception categories. Keep the BNF handy. Bookmark the list of 50+ drugs that must be prescribed by brand.
- Set defaults in your electronic prescribing system. Make generic the automatic choice. Only override when needed.
- Monitor your rates. NHS data shows practices that follow this process hit 92-95% generic prescribing within six months.
It’s not about perfection. It’s about consistency. Even if you miss one or two, you’re still saving money, reducing errors, and improving outcomes. And if you’re unsure? Ask. Talk to your pharmacist. Check the BNF. You’re not alone.
What’s changing-and what’s coming
The rules aren’t static. In March 2023, the MHRA updated its guidance to include complex generics like glatiramer acetate, which now require brand-name prescribing due to manufacturing sensitivity. The FDA is tightening post-market surveillance too. If a generic batch causes even one unexpected side effect, the manufacturer must report it. That’s new.
By 2025, 75% of small-molecule drugs will have generics. That’s good. But biologics? Only 40% will have biosimilars. And those will still need brand-name prescribing. The future isn’t about eliminating brands-it’s about using the right tool for the right job.
Some experts are now talking about “intelligent substitution.” That means using real-world data to decide who can safely switch-and who shouldn’t. For example, a stable patient on levothyroxine for five years? Keep the brand. A new patient starting on atorvastatin? Start with the generic. It’s not one-size-fits-all. It’s patient-by-patient.
That’s the real shift. Generic prescribing isn’t just a cost-cutting measure anymore. It’s a clinical decision. One that’s backed by data, guided by regulation, and rooted in patient safety.
What you need to remember
- Prescribe generically by default. It’s safe, effective, and saves money.
- Know the exceptions: narrow therapeutic index drugs, modified-release formulations, and biologics.
- Explain the switch. Patients trust you-not the label.
- Use your prescribing system’s defaults. Don’t rely on memory.
- Monitor patients who are sensitive-thyroid, epilepsy, anticoagulation.
- When in doubt, check the BNF. It’s updated regularly and freely available.
You’re not just writing a prescription. You’re shaping care. And when you prescribe generically, you’re not just saving the NHS money. You’re giving patients better access, fewer errors, and more consistent treatment. That’s not policy. That’s practice. And it works.
Are generic medications as effective as brand-name drugs?
Yes, for the vast majority of medications. Generic drugs must meet strict bioequivalence standards-proving they deliver the same amount of active ingredient into the bloodstream at the same rate as the brand. Regulatory bodies like the MHRA, FDA, and EMA require this before approval. Studies show no meaningful difference in clinical outcomes for drugs like atorvastatin, omeprazole, or sertraline when switched to generics. The only exceptions are drugs with narrow therapeutic indices or complex formulations.
Which drugs should always be prescribed by brand name?
According to the British National Formulary (BNF), brand-name prescribing is required for three categories: 1) Drugs with narrow therapeutic indices (e.g., warfarin, levothyroxine, phenytoin, carbamazepine, digoxin); 2) Modified-release formulations (e.g., theophylline, certain painkillers) where release kinetics matter; and 3) Biological medicines (e.g., insulin, infliximab, rituximab), where switching between originators and biosimilars can trigger immune responses. About 50 specific drugs fall into these categories-roughly 0.8% of all prescriptions.
Why do some patients say generics don’t work for them?
Often, it’s the nocebo effect-not the drug. When patients believe generics are inferior, they’re more likely to notice or report side effects, even if there’s no real difference. A 2021 study found that when doctors explained the equivalence of generics, patient acceptance rose from 67% to 89%. In rare cases, patients on antiepileptics or thyroid meds may experience instability after switching due to minor formulation differences. But these are exceptions, not the rule. Always check if the patient is on a high-risk medication before assuming the generic is the issue.
Can pharmacists substitute a generic without telling me?
In the UK, pharmacists can legally substitute a generic unless the prescription is marked “do not substitute” or the drug is on the BNF’s exception list (e.g., warfarin, levothyroxine). If you prescribe generically, substitution is automatic. If you prescribe by brand, substitution is only allowed if the brand isn’t on the exception list and the patient agrees. Always write clearly. If you want a specific brand, write the brand name and add “DAW” (Dispense As Written) or “do not substitute.”
Is there a risk of shortages with generic drugs?
Yes. In 2022, 287 generic drugs faced shortages in the UK and US, mostly due to manufacturing issues, raw material supply chains, or quality control failures. Some of these were critical drugs like injectable antibiotics or heart medications. While the FDA and MHRA now require more transparency and reporting, shortages still happen. If a generic is unavailable, you may need to prescribe the brand temporarily. Always check the NHS Shortages Bulletin before prescribing.
How do I know if my electronic system is set up correctly for generic prescribing?
Check your prescribing software’s default settings. Most systems (like SystmOne or EMIS) allow you to set generic names as the default. You should also confirm that the BNF’s exception list is loaded into your system’s alerts. If you’re still seeing brand names pop up automatically, contact your IT support. NHS England recommends auditing your prescribing data quarterly using the Prescribing Analytics Dashboard. If your generic rate is below 90%, you likely have defaults turned off or exceptions not properly flagged.

2 Comments
I've been on generic sertraline for 3 years now. Zero issues. My anxiety? Still managed. My wallet? Thank you. 🙌
Oh great, another UK nanny-state post. Next they'll tell me I can't choose my own toothpaste. In America, we don't let bureaucrats decide what medicine I get. 😤
Write a comment