Medication Dose Adjuster for Smokers
How This Tool Works
This calculator estimates medication dose adjustments based on smoking status and known metabolic changes. It is for educational purposes only and not medical advice. Always consult your doctor before changing any medication dose.
Enter your information to see dose recommendations
When you smoke, your body doesn’t just absorb nicotine-it changes how your liver processes almost every medication you take. This isn’t a minor side effect. It’s a powerful, measurable shift in drug levels that can turn a safe dose into a dangerous one-or make your medicine completely ineffective. If you smoke and take medications like theophylline, clozapine, or even diabetes drugs, your body is working differently than a non-smoker’s. And if you quit smoking, those changes don’t vanish overnight. They reverse. Slowly. And that’s when things get risky.
How Smoking Changes Your Body’s Drug Processing
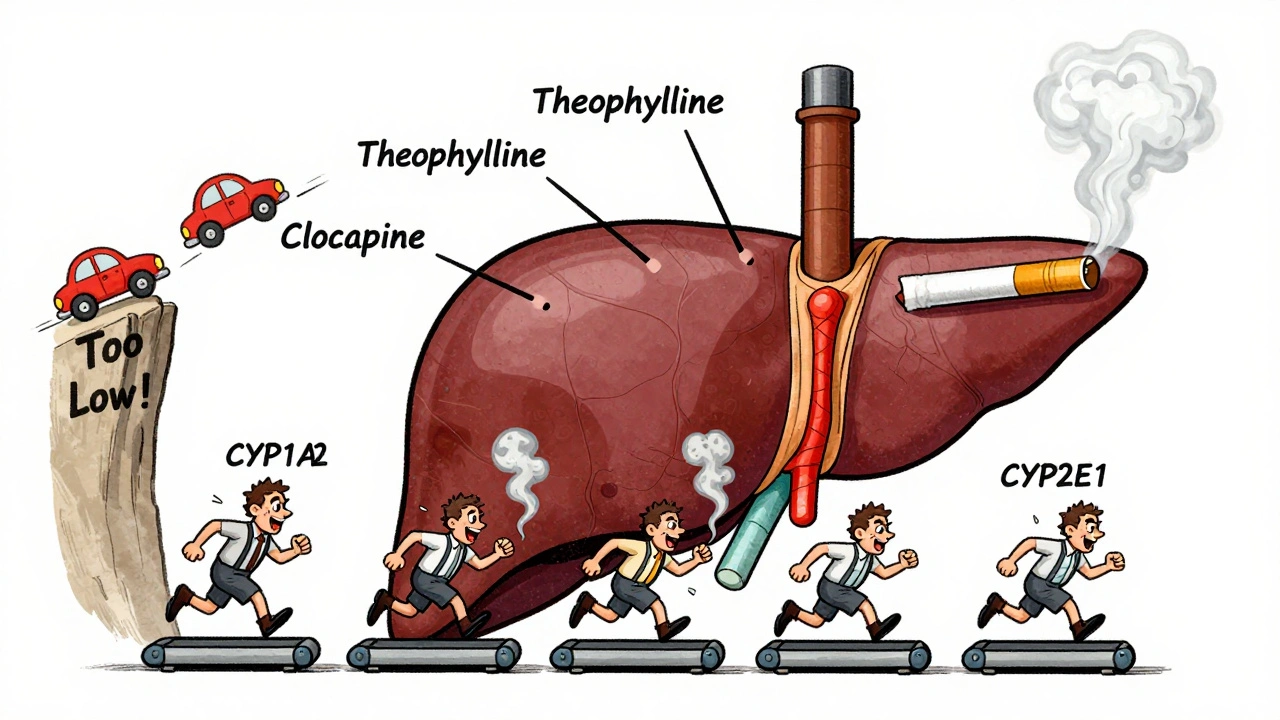
Tobacco smoke contains chemicals called polycyclic aromatic hydrocarbons (PAHs). These aren’t just toxins-they’re signals. When they enter your bloodstream, they trigger a switch in your liver: turn on more of certain enzymes. Specifically, CYP1A2, CYP1A1, CYP2E1, and some UGT enzymes. These are the same enzymes your body uses to break down drugs. When they’re turned up, your liver works faster. That means drugs get cleared out of your system more quickly. The result? Lower drug levels in your blood. For some medications, that’s not a big deal. But for others, even a 20% drop can mean your treatment stops working. Take theophylline, a drug used for asthma and COPD. In smokers, it’s cleared up to 100% faster. That means a dose that works perfectly for a non-smoker might be useless for someone who smokes. Studies show smokers often need 50-100% higher doses just to reach the same blood levels. This isn’t theoretical. It’s been documented since the 1970s. The World Health Organization flagged it as a major clinical issue back in 1985. Today, the American Society of Health-System Pharmacists says smoking is one of the most important factors to consider when prescribing medication.Which Medications Are Most Affected?
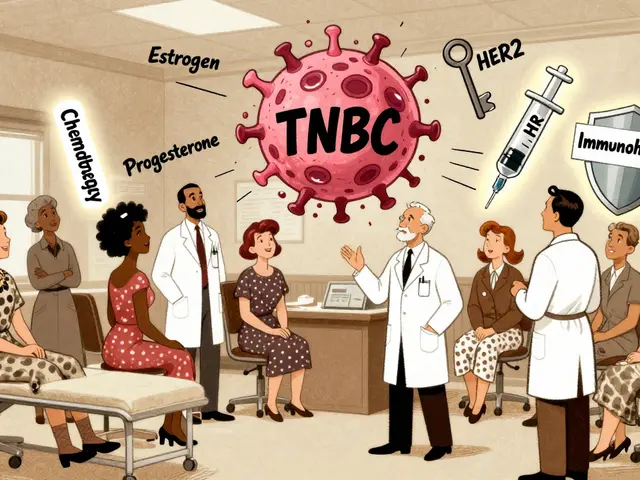
Not all drugs are impacted equally. The big winners-meaning the ones most affected-are those broken down primarily by CYP1A2. Here’s what you need to know:- Clozapine (an antipsychotic): Smokers need up to 50% higher doses. If they quit smoking, levels can spike dangerously high-leading to seizures, heart rhythm problems, or even death. Over 140 FDA reports link clozapine toxicity to smoking cessation.
- Theophylline: Clearance increases by 58-100%. Smokers may need double the dose. After quitting, levels can rise to toxic levels within days.
- Olanzapine: Smokers clear it 98% faster. Serum levels drop by 12%. Dose adjustments are often needed.
- Duloxetine (an antidepressant): CYP1A2 is its main metabolic pathway. Smokers may need higher doses to feel the effect.
- Pioglitazone (a diabetes drug): Smokers may need 20-30% higher doses. After quitting, blood sugar can crash unexpectedly.
- Mexiletine (an antiarrhythmic): Clearance increases by 25%. Half-life drops by 36%.
- Acetaminophen (Tylenol): CYP2E1 is one of its metabolic routes. Smokers may process it faster, but this also increases the risk of liver damage if high doses are taken.
Drugs metabolized by CYP2D6-like many SSRIs (fluoxetine, sertraline)-show little to no change. That’s good news for some, but it means you can’t assume all medications are safe just because one isn’t affected.
What Happens When You Quit Smoking?
This is where things get dangerous-and often overlooked. When you stop smoking, your enzyme levels don’t stay high. They begin to drop. Within 72 hours, CYP1A2 activity starts returning to normal. By day 7, it’s down by 30-40%. By 2-4 weeks, it’s back to baseline. That means drugs you were taking at a higher dose because you smoked? Now they’re building up in your system. A pharmacist in Ohio recently shared a case on Reddit: a patient was hospitalized for theophylline toxicity just 10 days after quitting smoking. His dose hadn’t changed. His body had. The same thing happens with clozapine. A 2023 study in Pharmacotherapy found that 89% of clozapine toxicity cases after smoking cessation occurred within the first 14 days. Doctors often don’t adjust the dose because they don’t realize smoking was the reason the dose was high in the first place. Even diabetes medications can cause problems. One patient on DiabetesDaily.com wrote: “My A1C dropped from 7.8% to 5.9% two weeks after quitting smoking-even though I didn’t change my meds. My doctor didn’t warn me this could happen.” That’s hypoglycemia. That’s dangerous.
Why Most Doctors Miss This
A 2022 survey found that only 37% of primary care doctors routinely ask about smoking status when prescribing theophylline. That’s not just negligence-it’s systemic. The problem? Medical training doesn’t emphasize this. Drug labels often mention smoking as a footnote. Electronic health records rarely prompt doctors to check smoking status before prescribing. And patients? Most don’t know to mention it. But the data doesn’t lie. The FDA has required tobacco interaction labeling on new drugs since 2015. The European Medicines Agency now requires smoking status to be studied for all new antipsychotics. The American Pharmacists Association says failure to address this is the most common preventable cause of medication-related hospitalizations among smokers.What You Should Do If You Smoke (or Quit)
This isn’t about scare tactics. It’s about safety. Here’s what you need to do:- If you smoke: Tell every doctor and pharmacist you see. Don’t assume they’ll ask. Bring a list of all your medications, including over-the-counter and supplements.
- If you’re starting a new medication: Ask: “Does smoking affect how this works?” If the answer is unclear, ask for a blood level test (like for theophylline or clozapine).
- If you quit smoking: Contact your doctor immediately. Tell them you’ve stopped. Ask if your doses need to be lowered. Don’t wait for symptoms. The most dangerous window is days 3-14 after quitting.
- Monitor for symptoms: For antidepressants or antipsychotics: dizziness, confusion, rapid heartbeat, tremors. For diabetes meds: sweating, shaking, fainting. For theophylline: nausea, vomiting, irregular heartbeat. These aren’t normal. They’re warning signs.
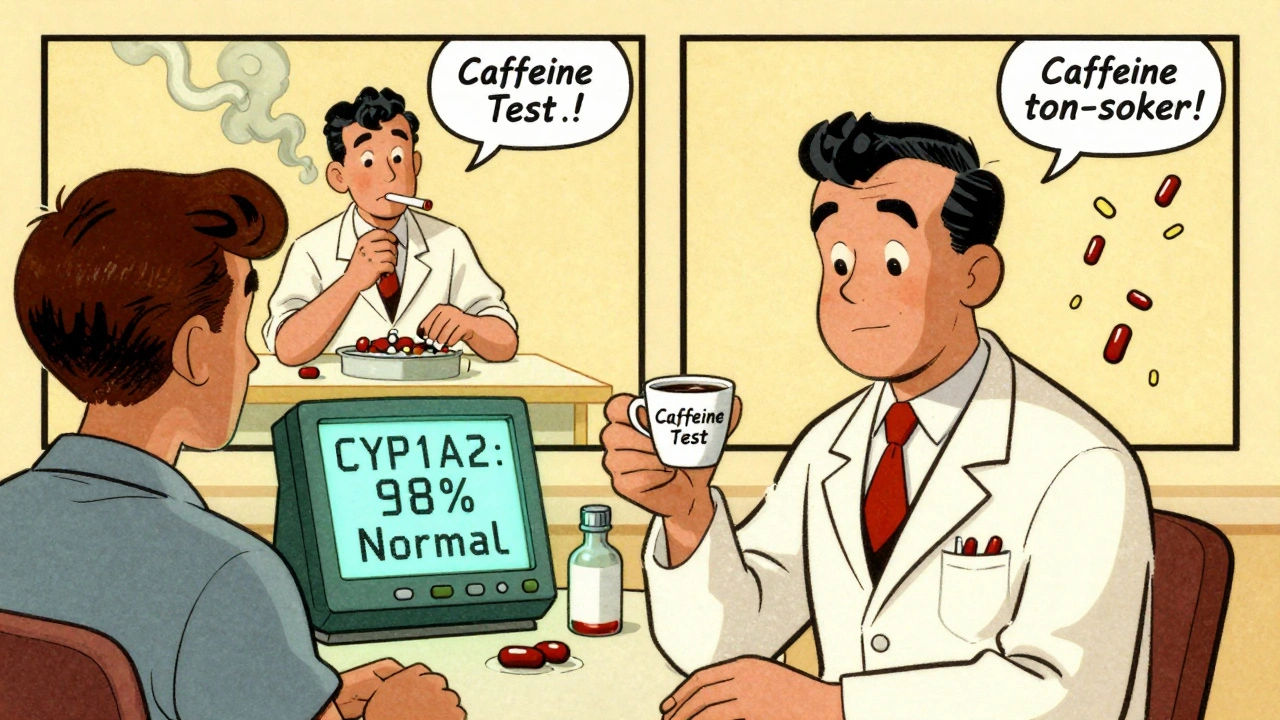
There’s even a new tool now called SmokeMetrix®, a simple test that measures how fast your body metabolizes caffeine-a direct marker of CYP1A2 activity. It’s FDA-approved and available in some clinics. It can tell you your enzyme level without guessing.
The Bigger Picture
About 34 million adults in the U.S. smoke. One in four people with schizophrenia smoke. One in five diabetics smoke. These aren’t just people who like cigarettes-they’re people on complex drug regimens that are being quietly undermined by their smoking. The cost? The U.S. healthcare system spends $2.3 billion a year treating preventable drug reactions linked to smoking. That’s not just money. It’s hospital stays. Emergency visits. Lost work. Families scared. The science is clear. The guidelines exist. The tools are here. What’s missing is awareness. If you smoke and take medication, this isn’t something to ignore. It’s something to act on. If you quit, this isn’t a victory you celebrate alone. It’s a medical event that needs planning.Frequently Asked Questions
Does smoking affect all medications?
No. Only medications broken down by specific liver enzymes-mainly CYP1A2, CYP2E1, and some UGTs-are affected. Common drugs like statins, most antibiotics, and many blood pressure pills aren’t impacted. But key ones like clozapine, theophylline, olanzapine, duloxetine, and pioglitazone are. Always ask your pharmacist: "Is this drug metabolized by CYP1A2?"
How long does it take for enzyme levels to return to normal after quitting smoking?
Enzyme activity starts dropping within 72 hours. By day 7, it’s down by about 30-40%. Full normalization usually takes 2-4 weeks. The most dangerous time is between days 3 and 14 after quitting, when enzyme levels are falling but drug doses haven’t been adjusted yet. That’s when toxicity risks peak.
Can I just stop my medication if I quit smoking?
No. Stopping medication abruptly can be dangerous. Instead, contact your doctor as soon as you quit. They may need to reduce your dose by 25-50%, depending on the drug. Never adjust your dose on your own-even if you feel fine.
Do nicotine patches or gum affect drug metabolism like smoking does?
No. Nicotine replacement therapies (patches, gum, lozenges) don’t contain the polycyclic aromatic hydrocarbons that trigger enzyme induction. Only tobacco smoke does. So if you’re using nicotine patches to quit smoking, your enzyme levels will still return to normal. You still need to adjust your medications, but not because of the patch-because you stopped smoking.
Is there a test to check if smoking is affecting my drug levels?
Yes. The most common is a caffeine metabolism test. Since caffeine is broken down almost entirely by CYP1A2, measuring how quickly your body clears it gives a direct readout of enzyme activity. A new FDA-approved test called SmokeMetrix® uses this method and is now available in some clinics. Blood tests for drug levels (like theophylline or clozapine) are also used routinely in hospitals.




10 Comments
Smoking while on meds is just lazy self-sabotage. You want the drug to work? Stop smoking. Simple.
The biochemical implications of polycyclic aromatic hydrocarbon-induced cytochrome P450 upregulation represent a paradigmatic case of pharmacokinetic interference, wherein the hepatic metabolism of therapeutics is disproportionately accelerated, thereby compromising therapeutic efficacy and precipitating iatrogenic harm. This is not merely a clinical footnote-it is a systemic failure of pharmacovigilance.
Okay but like… have you HEARD about SmokeMetrix®? It’s literally magic. My friend used it after quitting and her clozapine levels went from ‘danger zone’ to ‘perfect’ in two weeks. I’m obsessed. This is the future of personalized medicine and I’m here for it 🥹💊
It’s wild how we treat smoking like a moral failing instead of a physiological variable. Your liver doesn’t care if you’re ‘strong’ or ‘weak’-it just reacts to what’s in your blood. Maybe we need to stop shaming and start measuring.
So you’re telling me my grandma’s 20% dose reduction after quitting smoking wasn’t just ‘getting better’… it was her body finally not trying to kill her? Wow. I feel like a moron for not knowing this.
I quit last month. Took my diabetes med like normal. Woke up dizzy at 3am. Thought I was dying. Called my doc. They were like ‘oh lol yeah that’s normal’. I almost had a seizure because no one told me. Please tell everyone.
i never knew smokin affected meds like that. i thought it was just lungs and heart. turns out your liver’s just a worker bee that gets overworked by smoke. kinda sad. kinda scary. i’ll tell my doc tomorrow.
This article is dangerously oversimplified. The WHO flagged this in 1985. Why are we still having this conversation in 2025? The answer is incompetence. Not ignorance. Incompetence.
we’re all just chemicals in a bag of water trying to survive capitalism and cigarettes and bad prescriptions. maybe the real drug is the system that lets this happen
I’m crying. My brother died from clozapine toxicity after quitting. No one warned him. No one warned us. This is murder by neglect. 🥺💔 I’m sharing this everywhere. If you smoke and take meds… STOP. And if you quit… TELL YOUR DOCTOR. I’m begging you.
Write a comment