In 2023, Medicaid prescriptions for generic drugs saved patients and taxpayers over $53 billion-enough to cover healthcare for millions of Americans. The key to these savings lies in Medicaid generics-generic drugs covered under Medicaid. These medications make up 90-91% of all Medicaid prescriptions but account for only 17.5-18.2% of spending. How does this work for low-income patients? Let’s look at the facts.
Medicaid is a joint federal and state program established in 1965 under Title XIX of the Social Security Act. It provides health coverage for low-income individuals and families, covering essential services like hospital stays, doctor visits, and prescription drugs. Without Medicaid, many people couldn’t afford necessary treatments. Generics play a huge role here because they work just like brand-name drugs but cost far less.
Why Generics Are So Important for Medicaid
Medicaid covers over 80 million Americans. For prescription drugs, generic drugs are identical to brand-name medications in dosage, safety, and effectiveness but cost significantly less. They become available after a brand-name drug’s patent expires, allowing manufacturers to produce them at lower prices. In 2023, 90-91% of all Medicaid prescriptions were for generics. Yet these generics only made up 17.5-18.2% of total Medicaid drug spending. That’s because generics cost so much less than brand-name drugs.
Take copays as an example. Medicaid and CHIP Payment and Access Commission (MACPAC) is a federal agency that provides analysis and recommendations on Medicaid and CHIP programs. Their data shows the average copay for generic drugs under Medicaid is $6.16, while brand-name drugs cost $56.12-nearly nine times higher. For someone on a tight budget, that difference matters. A $6 copay is manageable; $56 might mean skipping doses or going without medication.
| Drug Type | Average Copay |
|---|---|
| Generic Drugs | $6.16 |
| Brand-Name Drugs | $56.12 |
How Medicaid Gets Such Low Prices
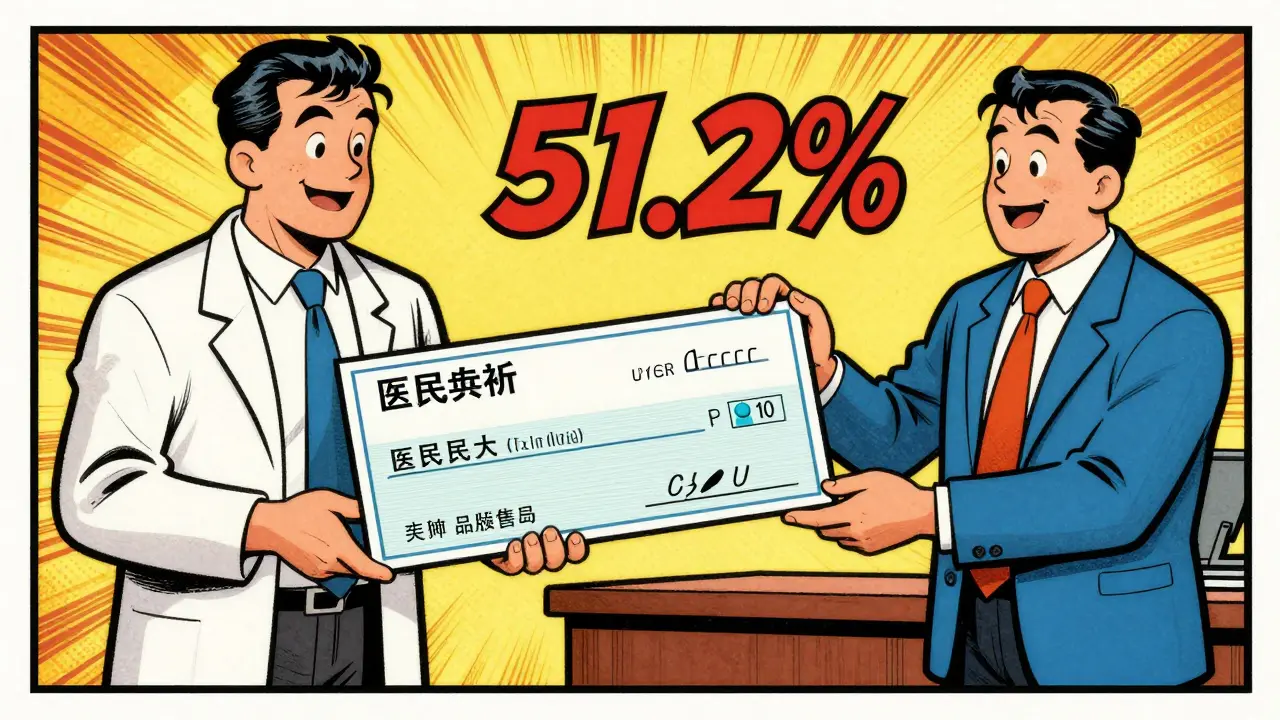
The Medicaid Drug Rebate Program (MDRP) was established by the Omnibus Budget Reconciliation Act of 1990. It requires drug manufacturers to provide rebates to Medicaid in exchange for having their drugs covered, ensuring lower prices for the program. For non-specialty generic drugs, Medicaid gets rebates equal to 86% of the retail price. In 2023, these rebates reduced overall gross Medicaid drug spending by 51.2%-or $53.7 billion. That means for every $100 spent on drugs, Medicaid only pays about $48.80 after rebates.
Compare this to other programs. A Congressional Budget Office study from 2021 found Medicaid gets better prices than the Department of Veterans Affairs. Medicaid’s average rebate for brand-name drugs is 77% of retail price, while the VA gets 70%. For specialty drugs, Medicaid’s rebates are 60% versus the VA’s 55%. This makes Medicaid the best deal for taxpayers and patients alike.
Challenges in the System
Despite these savings, there are hurdles. Pharmacy Benefit Managers (PBMs) are intermediaries that negotiate drug prices and manage prescription drug benefits. However, their fees can reduce the savings intended for Medicaid patients. For example, Ohio’s 2025 report found PBMs took 31% fees on $208 million in generic drug costs in one year. That’s money that could’ve gone directly to patients.
Another issue is specialty drugs. These high-cost medications-like those for cancer or rare diseases-make up less than 2% of Medicaid prescriptions but over half of the program’s spending. In 2021, Medicaid spent $80.6 billion on prescriptions but collected $42.5 billion in rebates, leaving net spending at $38.1 billion. By 2024, net spending rose to $60 billion-a $10 billion jump from 2022. This growth is mostly due to specialty drugs, not generics.
What’s Being Done to Fix This
To address rising costs, the Centers for Medicare & Medicaid Services (CMS) launched the GENEROUS Model in 2024. It focuses on reducing drug spending through better formulary management and cost-saving strategies. The goal is to curb the $10 billion increase in net drug spending from 2022 to 2024. This initiative includes encouraging the use of lower-cost alternatives and streamlining prior authorization processes.
Experts also point to biosimilars as future savings. Biosimilars are biologic drugs that mimic existing biologics but cost less. The Association for Accessible Medicines projects biosimilars could save $100 billion annually by 2027 as more biologic drugs lose patent protection. This could help Medicaid manage costs for high-priced treatments.

What Low-Income Patients Need to Know
Most Medicaid beneficiaries get generics automatically at the pharmacy. But there are things to watch for. For example, some states have higher copays for certain generics. Reddit discussions in r/Medicaid (July 2024) show users like "MedicaidMom2023" share experiences: "My daughter’s asthma inhaler was switched to generic and my copay dropped from $25 to $3, but getting approval took 3 weeks and multiple calls."
Here’s what to do: States manage Medicaid differently-48 use managed care organizations for pharmacy benefits. Know your state’s rules to avoid surprises. The average copay for generic drugs under Medicaid is $6.16, while brand-name drugs cost $56.12. This means generics are nearly nine times cheaper for patients. In 2023, Medicaid prescriptions for generics saved $53.7 billion in overall spending. Generics make up 90-91% of all Medicaid prescriptions but only 17.5-18.2% of spending. This is because they’re just as effective as brand-name drugs but cost far less. Without generics, Medicaid drug costs would be much higher, making it harder to cover all eligible patients. The Medicaid Drug Rebate Program (MDRP) requires drug manufacturers to give rebates to Medicaid in exchange for having their drugs covered. In 2023, these rebates reduced gross spending by 51.2%-saving $53.7 billion. For non-specialty generics, Medicaid gets rebates equal to 86% of the retail price. No. Each state manages its own Medicaid program, so coverage varies. Some states may require prior authorization for certain generics or have different copay tiers. Check your state’s Medicaid website or contact your local office for details on covered drugs. PBMs negotiate drug prices and manage prescription benefits, but their fees can reduce savings. For example, Ohio’s 2025 report found PBMs took 31% fees on $208 million in generic drug costs in one year. This means less money reaches patients, even when generics are cheaper overall. The GENEROUS Model is a CMS initiative launched in 2024 to address rising Medicaid drug costs. It focuses on reducing spending through better formulary design and cost-saving strategies. The goal is to curb the $10 billion increase in net drug spending from 2022 to 2024, especially for high-cost specialty drugs.
Frequently Asked Questions
How much do generics cost under Medicaid compared to brand-name drugs?
Why does Medicaid rely so heavily on generic drugs?
What is the Medicaid Drug Rebate Program?
Do all Medicaid programs cover the same generics?
How do Pharmacy Benefit Managers (PBMs) affect generic drug costs?
What is the GENEROUS Model?