Most people with chronic kidney disease (CKD) don’t know they have it-until it’s too late. By the time symptoms like fatigue, swelling, or foamy urine show up, the kidneys have already lost half their function. And yet, chronic kidney disease can be caught early, slowed down, and sometimes even stopped-before it leads to dialysis or transplant. The problem isn’t lack of knowledge. It’s lack of testing.
What Chronic Kidney Disease Really Means
Chronic kidney disease isn’t just about high creatinine or a single blood test. It’s a long-term condition where the kidneys slowly lose their ability to filter waste and fluid from the blood. To be diagnosed with CKD, two things must be true: kidney damage must be present for at least three months, and that damage must show up in one of two ways-either through reduced kidney function (measured by eGFR) or through signs of injury like protein in the urine. The key word here is both. For years, doctors relied mostly on serum creatinine to estimate kidney function. But creatinine levels vary wildly based on age, muscle mass, race, and even what you ate for dinner. That’s why so many cases slipped through the cracks. In 2012, global guidelines from KDIGO and KDOQI changed that. Now, diagnosis requires two tests: eGFR and uACR. One measures how well your kidneys are filtering. The other checks for tiny leaks of protein-early damage you can’t feel.The Two Tests That Save Kidneys
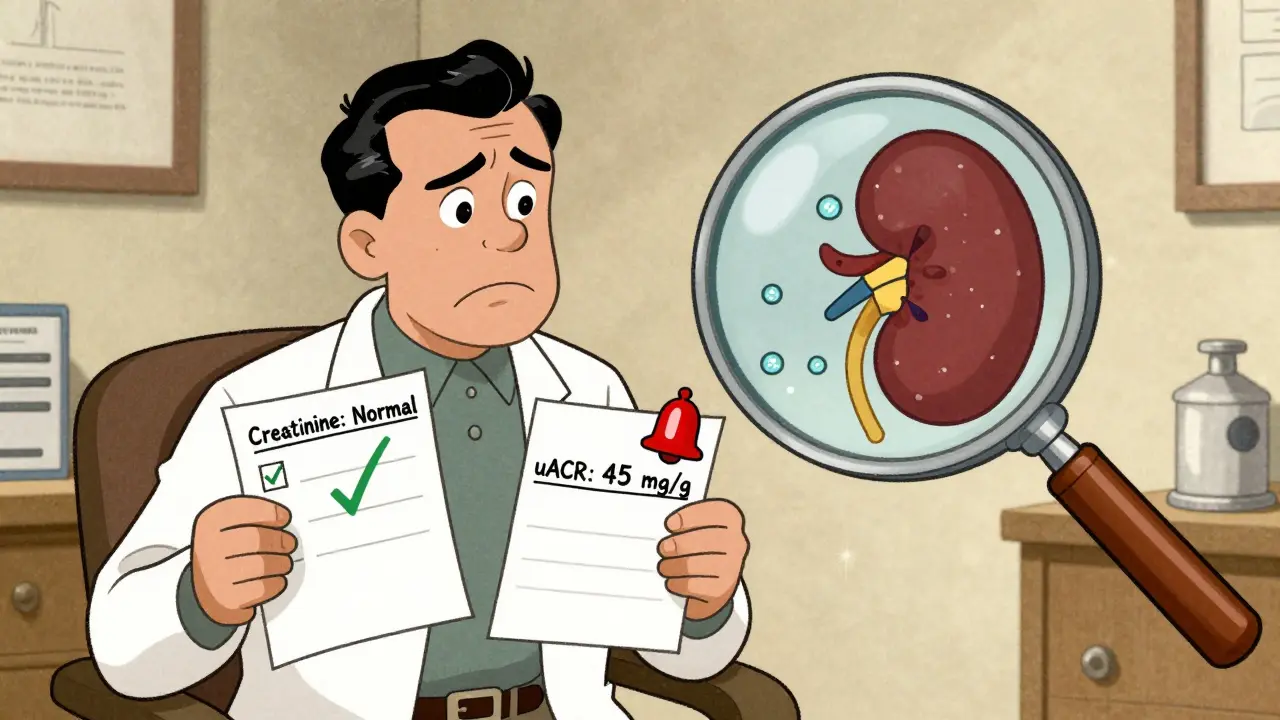
eGFR stands for estimated glomerular filtration rate. It’s not measured directly. It’s calculated using your blood creatinine level, age, sex, and race. The current standard is the CKD-EPI equation, which replaced older formulas because it’s more accurate, especially for people with mild kidney problems. But here’s the catch: if your eGFR is between 45 and 59, and you have no other risk factors, your doctor should consider checking your cystatin C-a different blood marker that’s less affected by muscle mass. This catches cases creatinine misses. uACR-urine albumin-to-creatinine ratio-is even more important for early detection. It’s a simple urine test. You pee in a cup, and the lab measures how much albumin (a type of protein) is leaking out compared to creatinine. A result of 30 mg/g or higher means your kidneys are leaking protein. That’s not normal. Even if your eGFR is still in the normal range (90+), having uACR ≥30 means you have stage 1 CKD. And that’s your warning sign. Many people think if their creatinine is normal, their kidneys are fine. That’s wrong. A 2018 national survey showed that up to 40% of early CKD cases were missed because doctors only checked creatinine. You need both tests. Always.Stages of CKD: Why Knowing Your Number Matters
CKD is divided into five stages based on eGFR and the presence of kidney damage:- Stage 1: eGFR ≥90, but uACR ≥30 → kidneys are working fine, but damage is already happening.
- Stage 2: eGFR 60-89, uACR ≥30 → mild decline, still early.
- Stage 3a: eGFR 45-59 → mild to moderate loss.
- Stage 3b: eGFR 30-44 → moderate to severe loss.
- Stage 4: eGFR 15-29 → severe loss.
- Stage 5: eGFR <15 → kidney failure.
Who Should Be Tested-and How Often
You don’t need to be sick to need this test. If you have any of these, you’re at risk:- Diabetes (type 1 or 2)
- High blood pressure
- Heart disease
- Family history of kidney failure
- Obesity
- Age over 60
- African American, Native American, or Hispanic heritage
How Early Detection Slows or Stops Progression
Finding CKD early isn’t just about knowing your number. It’s about acting on it. And the science is clear: early action saves kidneys. Medications: SGLT2 inhibitors (like dapagliflozin and empagliflozin), originally developed for diabetes, now have FDA approval for CKD-even in people without diabetes. The CREDENCE trial showed they reduce progression to kidney failure by 32% in people with albuminuria. Blood pressure control: Keeping your blood pressure below 130/80 mmHg (not 140/90) cuts the risk of kidney decline by 27%. ACE inhibitors or ARBs are often used because they also reduce protein in the urine. Diet and lifestyle: A 2022 meta-analysis found that people who got structured counseling-on salt, protein, and fluid intake-slowed their eGFR decline from 3.5 mL/min/year to just 1.2 mL/min/year. That’s a 66% reduction in the rate of damage. One patient in Exeter, diagnosed at stage 2 after a routine check-up, started on an SGLT2 inhibitor, cut her salt intake, and checked her blood pressure daily. Five years later, her eGFR is unchanged. She’s still working full-time. She didn’t need dialysis. She didn’t need a transplant. She just acted early.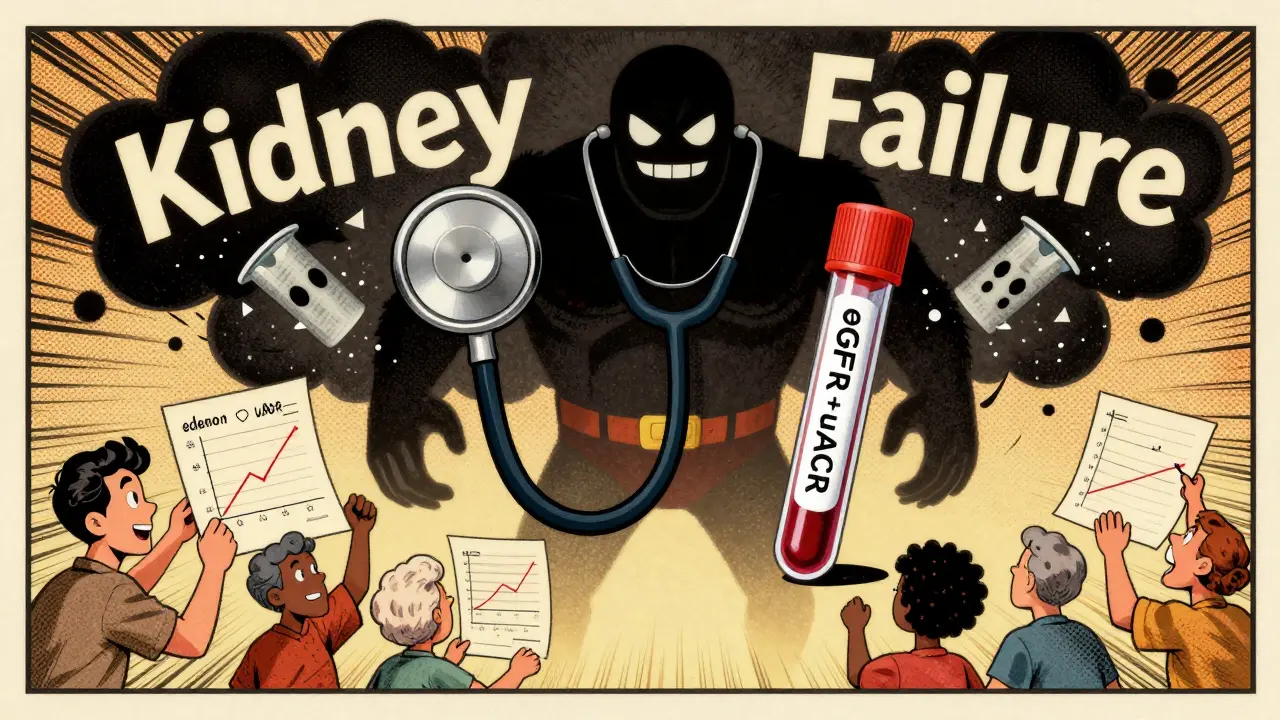
Why So Many Cases Are Still Missed
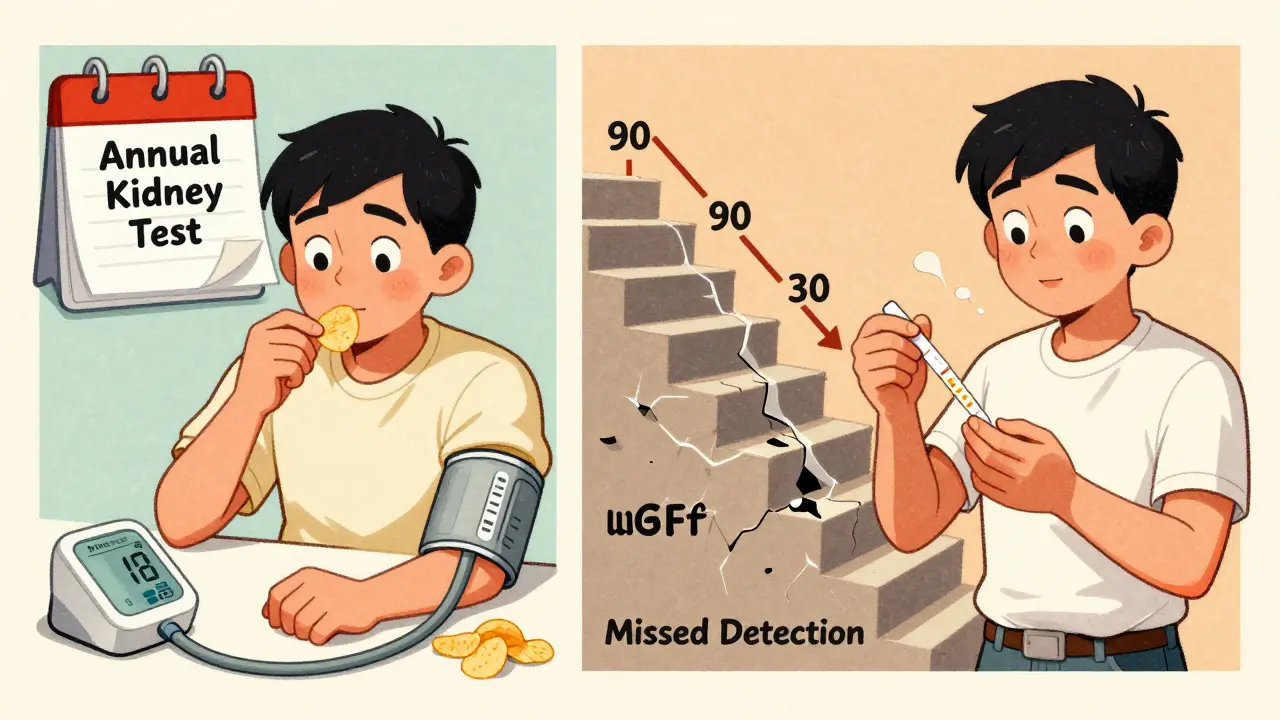
Despite the guidelines, most primary care doctors don’t order both tests. A 2022 study found only 53% of providers consistently ordered eGFR and uACR together. In rural clinics, that number dropped to 32%. Why? Electronic health records often don’t prompt for both. Doctors think “normal creatinine = normal kidneys.” Patients don’t ask. Insurance doesn’t always cover both tests unless there’s a clear reason. One Reddit user wrote: “My doctor only checked creatinine for 10 years. By the time they did uACR, I was stage 3.” That’s not rare. It’s routine. Another problem: overtesting in older adults. Someone over 85 with an eGFR of 50 but no proteinuria might not need aggressive treatment. Their kidneys may just be aging. But without proper context, doctors may over-treat, causing more harm than good.The Future Is Here-But Not Everywhere
New tools are changing the game. In May 2023, the FDA cleared the first AI-powered tool, NephroSight, that analyzes 32 clinical factors to predict CKD risk before eGFR drops. It’s being rolled out in VA hospitals and large health systems. The Biden administration is investing $150 million to require dual testing in all Federally Qualified Health Centers by 2026. That’s 1.2 million people who could be diagnosed early. Point-of-care uACR devices-machines that give results in 10 minutes-are coming. By 2025, you might get your kidney test result while you’re still sitting in the exam room. And the biggest shift? Removing race from eGFR calculations. For years, formulas added a “race correction” for Black patients, making their kidney function look better than it was. New data shows that removing this bias could increase early detection in African Americans by 12.3%. It’s not just fair-it’s more accurate.What You Can Do Right Now
If you’re at risk:- Ask your doctor for both eGFR and uACR-don’t settle for one.
- If you have diabetes or high blood pressure, get tested every year-no exceptions.
- If your results are borderline (eGFR 60-89, uACR 20-30), ask for a repeat test in 3 months. One abnormal result isn’t enough.
- Get a copy of your results. Know your numbers. Write them down.
- Use visual charts from the National Kidney Foundation. Patients who saw their stage on a simple graphic were 28% more likely to follow their treatment plan.
Can chronic kidney disease be reversed?
Early-stage CKD (stages 1-2) can often be stabilized or even improved with proper treatment. Medications like SGLT2 inhibitors, blood pressure control, and dietary changes can slow or stop damage. But once significant scarring occurs (stage 3 and beyond), the damage is usually permanent. The goal shifts from reversal to slowing progression.
Is a kidney biopsy always needed to diagnose CKD?
No. Most cases are diagnosed with just eGFR and uACR. A biopsy is only done in about 1-2% of cases-usually when the cause isn’t clear, like unexplained proteinuria without diabetes or high blood pressure, or when rapid decline happens. It’s not routine.
Does drinking more water help kidney function?
For most people with early CKD, drinking extra water doesn’t improve kidney function. In fact, forcing fluids can be harmful if you have heart or kidney failure. The key is staying normally hydrated-not overhydrating. Avoid sugary drinks and excessive salt. Focus on blood pressure, blood sugar, and protein in urine instead.
Why does my doctor care if I’m African American?
Historically, eGFR formulas included a race adjustment that assumed Black patients had higher muscle mass, leading to falsely higher kidney function estimates. This meant many cases were missed. Newer formulas remove race, and current guidelines recommend using cystatin C or direct measurement if the creatinine-based result seems off. Your race doesn’t cause kidney disease-but outdated math did.
Can I check my kidney health at home?
Not reliably. Home urine strips can detect protein, but they’re not accurate enough for diagnosis. They can give false positives or negatives. The only reliable way is a lab test for uACR and a blood test for eGFR. Some new point-of-care devices are coming, but they’re still in clinics-not pharmacies.
If I have CKD, do I need to see a kidney specialist?
Not always. Many people with stage 1 or 2 CKD can be managed by their primary care doctor, especially if their condition is stable and they’re following treatment. But if your eGFR drops below 45, your proteinuria increases, or you have other complications like anemia or bone disease, you should be referred to a nephrologist.




2 Comments
Just got my uACR back last week-32 mg/g. eGFR was 88. My doctor said, 'Eh, you're fine.' I pushed. They did cystatin C. Turned out my real eGFR was 56. I'm stage 3a now. Don't let them skip the second test. I almost died because they trusted creatinine alone.
My dad’s been on dialysis for 4 years. He didn’t know he had CKD until his legs swelled up like balloons. If someone had just told him to get the two tests when he turned 60…
Write a comment