Antidepressant Sexual Side Effect Comparison Tool
Select Your Antidepressant
If you're taking an antidepressant and noticing your sex drive has vanished, or sex has become harder, slower, or just... flat-you're not alone. In fact, up to 70% of people on SSRIs like sertraline or fluoxetine report some kind of sexual side effect. And many of them stop taking their meds because of it. The problem isn't just physical. It’s emotional. It’s relational. It’s the quiet shame of feeling broken when you thought you were finally getting better.
Why Do Antidepressants Kill Your Sex Drive?
It’s not about being "weak" or "not attracted anymore." It’s chemistry. Antidepressants like SSRIs (sertraline, fluoxetine, paroxetine) work by increasing serotonin in your brain. That helps lift your mood. But serotonin doesn’t just affect sadness-it also shuts down the dopamine and norepinephrine pathways that drive sexual desire, arousal, and orgasm. Think of it like turning down the volume on your entire sexual response system. It’s not broken. It’s just muted. Men commonly report trouble getting or keeping an erection (58%), delayed or absent ejaculation (53%), and low desire (64%). Women often experience dryness (52%), inability to climax (49%), and loss of interest (61%). These aren’t rare side effects. They’re the norm for many drugs in this class. And here’s the twist: depression itself can cause the same symptoms. About 35-50% of people with untreated major depression already have low libido or sexual dysfunction. So when you start an antidepressant and your sex life doesn’t improve, is it the medication? Or is it the depression still hanging on? That’s why doctors need to track your sexual health-not just your mood.Not All Antidepressants Are Created Equal
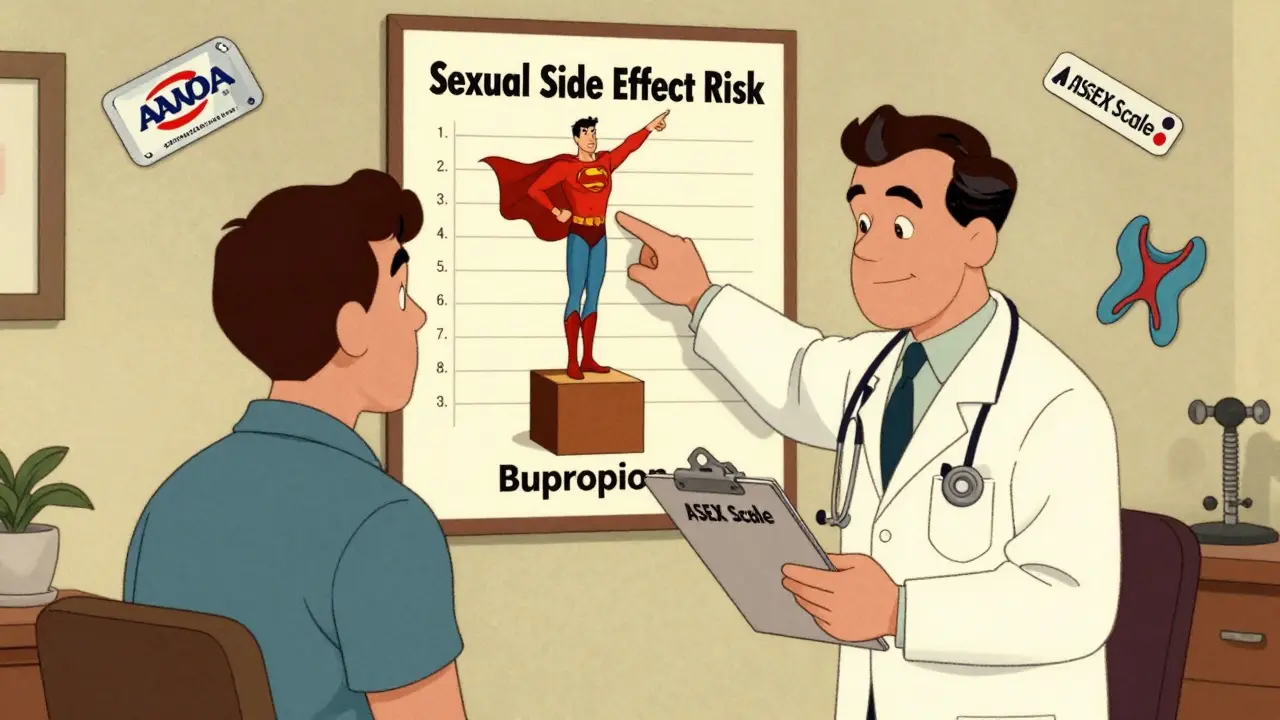
The risk isn’t the same across the board. Some drugs are far more likely to wreck your sex life than others. Paroxetine (Paxil) has the highest risk. For every 2-5 people taking it, one will develop sexual dysfunction that didn’t exist before. Sertraline (Zoloft) and citalopram (Celexa) aren’t far behind. Fluoxetine (Prozac) is a bit better, but still problematic for many. Now compare that to bupropion (Wellbutrin). It works differently-it boosts dopamine and norepinephrine, not serotonin. And guess what? It doesn’t kill your libido. In fact, studies show it causes less sexual dysfunction than SSRIs. One trial found 68% of women who switched from an SSRI to bupropion saw their sexual function improve. That’s not a fluke. That’s science. Other low-risk options include:- Mirtazapine (Remeron): Often used for sleep and appetite, it has minimal sexual side effects.
- Agomelatine (Valdoxan): Used in Europe, it targets melatonin receptors and has a clean sexual side effect profile.
- Nefazodone (Serzone): Effective but rarely used due to rare liver risks.
What If You Don’t Want to Switch?
Maybe you’re happy with your current drug. Maybe it’s the only thing keeping you afloat. You don’t have to quit. There are ways to fix the problem without ditching the antidepressant. 1. Lower the dose. Sometimes, just reducing the amount helps. About 20-30% of people regain some sexual function with a lower dose. But be careful-go too low, and your depression might come back. 2. Try a "drug holiday." Skip your pill for 24-48 hours before planned sexual activity. Works best with longer-acting drugs like fluoxetine. Not safe with paroxetine-it leaves your system too fast and can trigger withdrawal symptoms like dizziness or brain zaps. 3. Add something on. This is where things get powerful.- Sildenafil (Viagra) helps men on SSRIs. Studies show 65-70% of men saw better erections compared to 25% on placebo.
- Bupropion as an add-on (150mg daily) helped 58% of women on SSRIs regain sexual function in a 2019 trial.
- Cyproheptadine (an old antihistamine) at 4mg nightly helped 52% of people with SSRI-induced anorgasmia in a 2021 study-double the placebo rate.

What About Post-SSRI Sexual Dysfunction (PSSD)?
This is the scary part. A small number of people-0.5-1.2%-report sexual problems that don’t go away after stopping the drug. Symptoms include persistent low libido, genital numbness, and inability to orgasm. It can last months or even years. It’s rare, but it’s real. Since 2010, 28 peer-reviewed case reports have documented it. The FDA now requires stronger warnings on antidepressant labels because of these reports. If you’ve been off your medication for more than six months and still feel "off" down there, you’re not imagining it. Talk to a specialist. There’s no cure yet, but some people find relief with cognitive behavioral therapy, pelvic floor physical therapy, or time.How to Talk to Your Doctor About This
Most doctors don’t bring it up. So you have to. Here’s how:- Use simple language: "I’ve noticed my sex drive has dropped since starting this med. Is this common?"
- Ask about screening tools: The Australia Sexual Experience Scale (ASEX) is a quick 5-question tool doctors can use to measure dysfunction.
- Request alternatives: "Can we look at bupropion or mirtazapine?"
- Ask about add-ons: "Would adding sildenafil or low-dose bupropion help?"
Real Numbers, Real Choices
Let’s say you’re on sertraline and struggling. Here’s what your options look like:| Drug | Sexual Side Effect Risk | Switch Success Rate | Monthly Cost (Generic) |
|---|---|---|---|
| Paroxetine (Paxil) | Very High (NNH: 2-4) | Low | $12 |
| Sertraline (Zoloft) | High (NNH: 3-5) | Medium | $58 |
| Bupropion (Wellbutrin XL) | Low (NNH: 17) | High (68% improve) | $16 |
| Mirtazapine (Remeron) | Low | Medium | $10 |
| Fluoxetine (Prozac) | Medium | Medium | $25 |
What About Newer Options?
Esketamine (Spravato), the nasal spray for treatment-resistant depression, has only a 3.2% rate of sexual side effects. But it costs $880 per dose and requires clinic visits. Not practical for most. In trials, a new drug called SEP-227162 (a serotonin receptor modulator) reduced sexual side effects by 87% compared to sertraline. It’s still in Phase II, but if it works, it could change everything.What Not to Do
Don’t quit cold turkey. Especially with paroxetine or sertraline. You risk withdrawal symptoms: brain zaps, nausea, anxiety, dizziness. Don’t rely on Reddit or YouTube. Yes, 78% of people on r/antidepressants say their relationships suffered. But anecdotal stories aren’t evidence. Some people improve on their own. Others need help. Don’t assume it’s "just in your head." This is a biological effect. You’re not broken. Your brain chemistry is just out of sync.Final Thoughts
You didn’t start antidepressants to lose your sex life. You started them to feel better. If the trade-off is too high, you have options. Switching meds. Adding something. Lowering the dose. These aren’t last resorts-they’re standard tools in psychiatric care. The goal isn’t just to survive depression. It’s to live. And that includes intimacy, connection, and pleasure. You deserve both.Do all antidepressants cause sexual side effects?
No. While SSRIs and SNRIs like sertraline and venlafaxine commonly cause sexual side effects, other antidepressants like bupropion, mirtazapine, and agomelatine have much lower rates. About 35-70% of people on SSRIs experience issues, but only 5-15% on bupropion do. The risk varies by drug class and individual biology.
Can sexual side effects go away on their own?
Sometimes, but rarely. Clinical trials show 30-40% of people improve after 6 months. But real-world patient reports show only 18% notice improvement over the same period. This gap suggests most people don’t adapt-especially if the drug dose stays high. Don’t wait for it to fix itself. Talk to your doctor.
Is bupropion safe for everyone?
Bupropion is generally safe but not for everyone. It can increase seizure risk in people with eating disorders or a history of seizures. It may also worsen anxiety or cause insomnia. It’s not recommended for those with bipolar disorder unless paired with a mood stabilizer. Always discuss your full medical history before switching.
How long does it take to see improvement after switching antidepressants?
It usually takes 2-4 weeks for a new antidepressant to reach full effect. Sexual side effects may improve sooner-some report changes in libido within 1-2 weeks after switching to bupropion. But full stabilization can take up to 6 weeks. A gradual cross-taper (slowly reducing the old drug while increasing the new one) helps avoid withdrawal and mood swings.
Can I use Viagra with my antidepressant?
Yes, sildenafil (Viagra) is safe and effective for men taking SSRIs. Studies show it improves erectile function in 65-70% of cases. It doesn’t interact dangerously with antidepressants. However, it won’t help with low desire or anorgasmia-only erection quality. Women may benefit from other options like bupropion add-ons or topical testosterone creams (off-label, under supervision).
What’s the best way to track sexual side effects?
Use the Arizona Sexual Experience Scale (ASEX). It’s a 5-question tool doctors use to measure desire, arousal, orgasm, satisfaction, and distress. You can ask your provider to use it at your next visit. Tracking your symptoms on paper or in a journal also helps-note changes in libido, timing of symptoms, and whether they worsen with dose increases.
Are there natural remedies that help?
There’s no strong evidence that herbs like ginseng, maca, or L-arginine reliably fix SSRI-induced sexual dysfunction. Some people report mild improvements, but these aren’t backed by controlled trials. The most effective solutions are medical: switching meds, adding bupropion or sildenafil, or adjusting dose. Don’t waste time or money on unproven supplements.
Can therapy help with sexual side effects?
Yes. Cognitive behavioral therapy (CBT) and sex therapy can help you cope with the emotional impact-reducing shame, improving communication with partners, and rebuilding intimacy even when desire is low. Therapy won’t fix the biology, but it can help you reconnect emotionally. Many people find this combination-medication adjustment plus therapy-works best.
How common is post-SSRI sexual dysfunction (PSSD)?
PSSD is rare-estimated at 0.5-1.2% of users. But it’s real and persistent. Symptoms include low libido, genital numbness, and inability to orgasm, lasting months or years after stopping the drug. While most people recover fully, a small group doesn’t. If you notice ongoing issues after discontinuing an SSRI, seek a specialist. Research is ongoing, and support groups exist for those affected.
Should I stop my antidepressant if I have sexual side effects?
Don’t stop without talking to your doctor. Stopping abruptly can cause withdrawal symptoms or trigger a return of depression. Instead, ask for alternatives: switching meds, lowering the dose, or adding an antidote like bupropion or sildenafil. You don’t have to choose between mental health and sexual health. There’s a middle path.



1 Comments
The pharmaceutical-industrial complex has engineered this exact outcome: depersonalized intimacy to ensure dependency. SSRIs are not medicine-they are social control disguised as treatment. You think you’re healing? You’re being optimized for compliance.
Write a comment