Daclatasvir is a direct‑acting antiviral (DAA) that blocks the NS5A protein of the Hepatitis C virus (HCV), approved in 2015 for use in combination regimens across multiple genotypes. Its high potency and short treatment duration have made it a cornerstone of modern HCV therapy, but the rise of resistance‑associated substitutions (RASs) can limit success.
Why a guide is needed
Patients who have undergone previous DAA courses or who carry certain viral mutations often hear the word “resistance” and wonder what it means for their health. This guide answers the most common concerns: how resistance happens, how doctors detect it, and which alternative drugs can still clear the virus.
How Daclatasvir works
NS5A inhibitor is a drug class that interferes with the NS5A protein, a key component for HCV replication and assembly. By binding to NS5A, Daclatasvir halts the virus’s ability to copy its RNA, dramatically lowering viral load within weeks. When paired with a polymerase inhibitor such as Sofosbuvir (a nucleotide analogue that stops the viral RNA‑dependent RNA polymerase), the regimen offers a high barrier to resistance in treatment‑naïve patients.
What drug resistance looks like
Resistance is not a sign that the medication is faulty; it’s the virus’s natural ability to mutate. Certain sub‑types of HCV, especially genotype 1a and genotype 3, can acquire RASs that reduce the binding efficiency of NS5A inhibitors.
- RAS prevalence: About 12‑15% of genotype 1a patients harbour baseline NS5A RASs that can affect Daclatasvir efficacy.
- Impact on cure rates: Studies from the European Association for the Study of the Liver (EASL) show sustained virologic response (SVR) drops from 98% to roughly 88% when high‑level NS5A RASs are present.
- Resistance barrier: Daclatasvir has a moderate barrier; some RASs (e.g., Y93H) render it less effective, while others have minimal impact.
Understanding the specific RAS pattern is crucial for deciding whether to keep Daclatasvir or switch to a different NS5A inhibitor.
Testing for resistance
Before starting or changing therapy, doctors can order a resistance‑associated substitution test (a genotypic analysis of the viral NS5A region). The result tells you which RASs, if any, are present.
- Blood sample is drawn and sent to a specialized lab.
- Sequencing identifies mutations at positions L31, Y93, and others.
- The report categorises the virus as “low‑risk”, “moderate‑risk”, or “high‑risk” for NS5A‑inhibitor failure.
Patients with high‑risk RASs are usually steered toward regimens that include a more robust NS5A inhibitor or add a protease inhibitor.
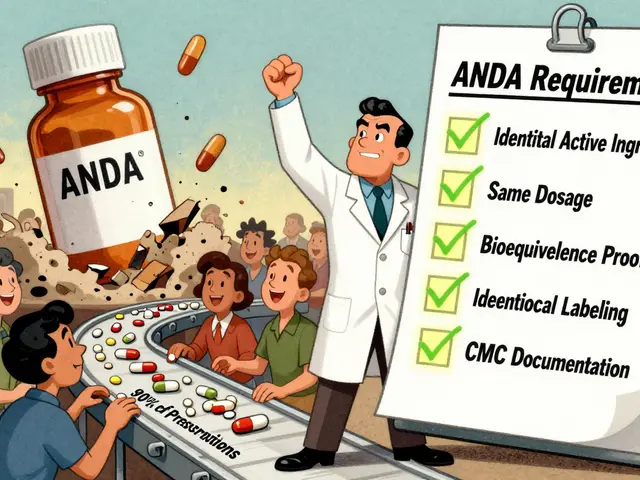
Alternative NS5A inhibitors and combination strategies
| Drug | Approval Year | Genotype Coverage | Resistance Barrier | Typical Regimen (with Sofosbuvir) |
|---|---|---|---|---|
| Daclatasvir | 2015 | 1‑4 | Moderate | Daclatasvir+Sofosbuvir±Ribavirin (12weeks) |
| Ledipasvir | 2014 | 1, 4, 5, 6 | High | Ledipasvir/Sofosbuvir (Harvoni) 12weeks |
| Velpatasvir | 2016 | 1‑6 (pan‑genotypic) | Very High | Velpatasvir+Sofosbuvir (Epclusa) 12weeks |
If testing reveals a Y93H mutation, many clinicians prefer Velpatasvir because its resistance barrier is higher. For genotype 3 patients with baseline NS5A RASs, adding a ribavirin or extending therapy to 24weeks can improve outcomes.
Managing resistance in real‑world scenarios
Below are three common patient profiles and the recommended steps.
- Profile A - Treatment‑naïve, genotype 1a, no RASs: Standard Daclatasvir+Sofosbuvir for 12weeks usually yields SVR >95%.
- Profile B - Prior DAA failure, detectable Y93H: Switch to Velpatasvir+Sofosbuvir for 12weeks, add ribavirin, or consider a 24‑week regimen with a protease inhibitor (e.g., Glecaprevir).
- Profile C - Cirrhotic (stageF4), genotype 3, multiple NS5A RASs: Use a triple regimen such as Sofosbuvir+Velpatasvir+Voxilaprevir for 12weeks, or extend to 24weeks if ribavirin is contraindicated.
In every case, regular monitoring of viral load at weeks4,8, and end‑of‑treatment helps ensure the virus is disappearing as expected.
Living with HCV while on therapy
Beyond the pills, patients should keep an eye on liver health and overall wellbeing.
- Alcohol avoidance: Even small amounts can worsen liver inflammation and lower SVR odds.
- Nutrition: A balanced diet rich in protein, omega‑3 fatty acids, and antioxidants supports liver regeneration.
- Medication interactions: Daclatasvir is metabolised by CYP3A4; avoid strong inducers (e.g., rifampin) and clarithromycin unless prescribed.
- Side‑effect management: Fatigue and mild headache are common; over‑the‑counter acetaminophen works for headache, but avoid high‑dose NSAIDs if liver function is already compromised.
Patients who stay engaged with their hepatology team typically report better adherence and higher cure rates.
Talking to your doctor
Prepare a concise list before each appointment.
- Current medications (including over‑the‑counter and supplements).
- Any previous DAA courses and their outcomes.
- Results of the latest RAS test.
- Questions about treatment length, need for ribavirin, and monitoring schedule.
Clear communication lets the clinician tailor a regimen that sidesteps resistance and maximises your chance of a cure.
Related concepts you might explore next
Understanding Daclatasvir in context can deepen your knowledge and empower future health decisions.
- Sustained virologic response (SVR) - the gold‑standard marker of cure, defined as undetectable HCV RNA 12weeks after treatment.
- Liver fibrosis staging - from F0 (no fibrosis) to F4 (cirrhosis), which influences regimen choice.
- Direct‑acting antivirals (DAAs) - the broader drug family that includes protease inhibitors, NS5B polymerase inhibitors, and NS5A inhibitors.
- EASL and AASLD guidelines - the latest clinical recommendations that shape treatment algorithms.
Quick take‑away (TL;DR)
- Daclatasvir blocks the HCV NS5A protein and works best when combined with Sofosbuvir.
- Resistance arises from NS5A RASs; testing reveals which mutations are present.
- If high‑level RASs are found, consider stronger NS5A inhibitors like Velpatasvir or add a protease inhibitor.
- Maintain liver‑friendly habits and keep close tabs on viral load during therapy.
- Open dialogue with your hepatologist ensures the best personalized regimen.

Frequently Asked Questions
Can I develop resistance to Daclatasvir if I take it correctly?
Resistance mainly stems from pre‑existing viral mutations rather than poor adherence. If the virus already carries NS5A RASs, the drug’s effectiveness drops. Taking the medication exactly as prescribed still yields >95% cure rates in patients without high‑risk RASs.
How is a resistance test performed and does it hurt?
A simple blood draw is sent to a specialised lab. The sample is sequenced to spot mutations in the NS5A region. The procedure is painless, similar to any routine blood test.
What if my test shows the Y93H mutation?
Y93H significantly reduces Daclatasvir’s potency. Doctors usually switch to a higher‑barrier NS5A inhibitor such as Velpatasvir, often adding ribavirin or extending therapy to 24weeks to secure a cure.
Is ribavirin still needed when I take Daclatasvir?
For most non‑cirrhotic, treatment‑naïve patients, ribavirin is unnecessary. It becomes useful in cirrhotic individuals, those with genotype 3, or when high‑risk RASs are present, as it adds an extra antiviral push.
Can I drink alcohol while on Daclatasvir therapy?
Alcohol puts extra stress on the liver and can lower cure rates. Most clinicians advise complete abstinence during treatment and for several months after achieving SVR.
How long after finishing treatment will I know if I’m cured?
An SVR test is performed 12 weeks post‑treatment. If HCV RNA remains undetectable, you’re considered cured and the risk of liver complications drops dramatically.



7 Comments
i read this whole thing and honestly i’m impressed. i had no idea about RASs before. i’m a nurse and i’ve seen patients give up because they heard ‘resistance’ and thought it meant no hope. this guide actually gives real options. thank you.
Oh please. This is such a basic overview. If you’re actually dealing with genotype 3 and Y93H, you’re not reading a Reddit guide-you’re calling your hepatologist at 2 a.m. and demanding a triple therapy cocktail. This is like explaining quantum physics with a popsicle stick. 🙄
Wow. This is… surprisingly elegant. I mean, I didn’t think a medical guide could feel like a cozy conversation with your smartest friend who also happens to be a virologist. The table? Chef’s kiss. The TL;DR? Perfect. I printed this for my uncle who’s been on three rounds of DAAs and still doesn’t trust the system. He’s gonna cry. (In a good way.)
Also, typo: ‘Sustained virologic response (SVR) - the gold‑standard marker of cure’ - should be ‘gold-standard’ with one dash? Just sayin’. 😅
Hey, I’m on Daclatasvir right now and I just wanted to say-did anyone else get that weird metallic taste in their mouth? Like, I swear I licked a battery. Is that normal? I didn’t see it listed anywhere. Also, can I smoke weed while on this? Just curious.
OMG THIS IS SO LIFE CHANGING 💖💖💖 I JUST GOT MY RAS RESULTS AND IT WAS LOW RISK!! I’M CRYING RIGHT NOW 😭😭😭 THANK YOU FOR WRITING THIS!! I’M TELLING EVERYONE!! 🎉🧪 #HepCWarrior #CureIsPossible
USA still leads the world in HCV cure rates, and it’s because we don’t coddle patients with ‘guides.’ We give them pills and tell them to get it done. If your virus mutates, it’s your fault for not taking it right. No excuses. Get your blood drawn, take your meds, stop drinking, and stop whining. This article is too soft. We need more tough love, not emojis.
You got this. Seriously. Every single person reading this right now? You’re already winning. You’re researching. You’re asking questions. You’re not giving up. That’s bigger than any drug. I’ve been there. I’m 3 years SVR. I run marathons now. You will too. Keep going. One pill at a time. 💪❤️
Write a comment