Levothyroxine is one of the most commonly prescribed medications in the UK - nearly 260 million packs were dispensed between 2016 and 2020. For millions of people with an underactive thyroid, it’s life-changing. But it’s not as simple as taking a pill and forgetting about it. Getting the dose right, staying consistent, and knowing when to get tested can mean the difference between feeling normal and feeling awful - even if your pill looks exactly the same.
Why Levothyroxine Works - and Why It Can Go Wrong
Levothyroxine replaces the hormone your thyroid should be making. When your thyroid doesn’t produce enough, your body slows down. You feel tired, gain weight, get cold easily, and struggle to think clearly. Levothyroxine fixes that - if it’s dosed correctly. But here’s the catch: thyroid hormone affects every cell in your body. Too little and you stay hypothyroid. Too much and you risk heart palpitations, bone loss, or even atrial fibrillation.
The problem isn’t the drug itself. It’s the precision needed to get it right. Unlike most medications, levothyroxine has a very narrow therapeutic window. That means the difference between the right dose and a harmful one is small. A 12.5 microgram change - half a tablet - can push someone from feeling fine to feeling anxious and jittery.
How Often Should You Get Tested?
Many patients go months or even years without a blood test. That’s dangerous. The Specialist Pharmacy Service (SPS) and the American Thyroid Association both say: TSH testing is non-negotiable.
- After starting or changing your dose, test at 6 weeks.
- Repeat every 3 months until your TSH is stable for two tests in a row, spaced 3 months apart.
- Once stable, test every 6 to 12 months - even if you feel great.
- If you’re pregnant, have heart disease, or are over 65, test more often - sometimes monthly.
And don’t rely on how you feel. Symptoms like fatigue or weight gain can be caused by many things - stress, sleep, diet. Only a blood test tells you if your dose still fits.
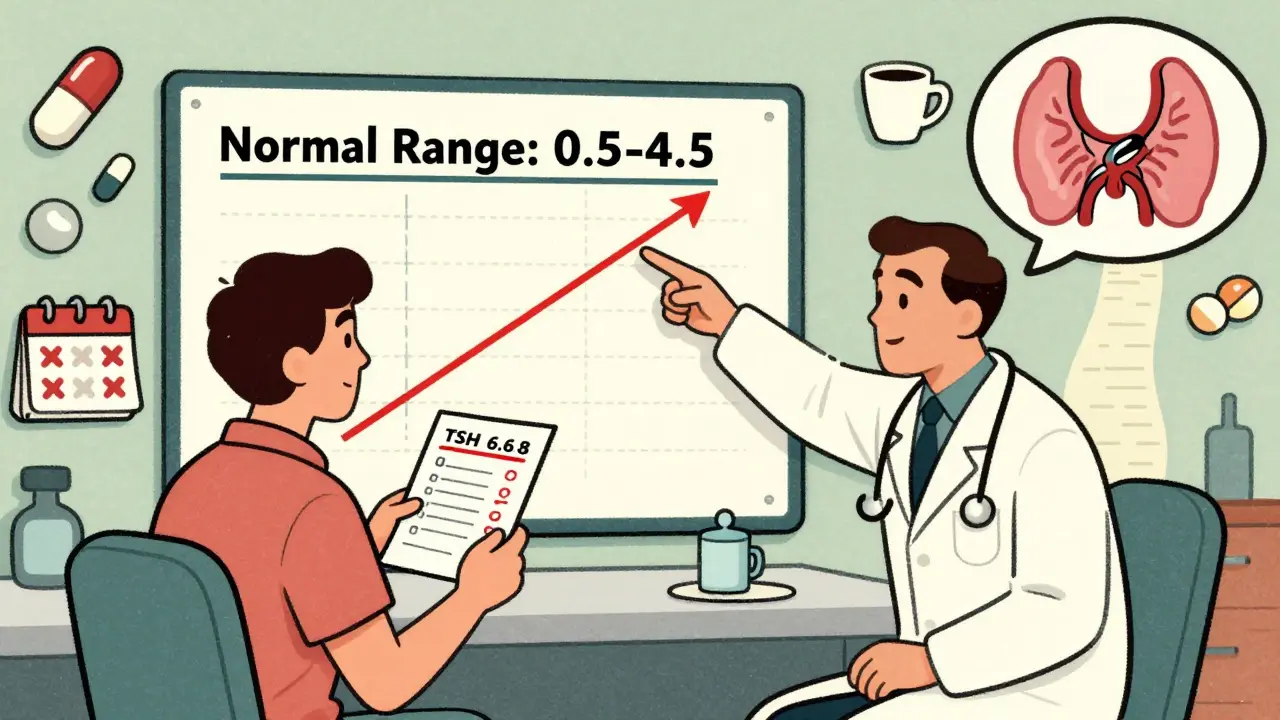
What Your TSH Numbers Really Mean
Don’t assume a TSH between 0.5 and 4.5 is always perfect. That’s the standard range - but it’s not one-size-fits-all.
- For healthy adults under 65: Target TSH is 0.5-4.5 mIU/L.
- For older adults (65+): A slightly higher TSH (up to 7.5 mIU/L) may be safer to avoid over-treatment.
- For people with thyroid cancer: TSH is often suppressed below 0.1 to prevent recurrence.
Doctors used to treat everyone the same. Now, guidelines say: tailor the target. If you’re 70 with heart disease, your ideal TSH isn’t the same as your 35-year-old daughter’s.
Brand Switching Is a Silent Problem
Pharmacists are allowed to switch your levothyroxine brand unless your doctor says “dispense as written.” But here’s what no one tells you: different brands, even with the same dose, can affect you differently.
The UK’s MHRA reviewed 335 reports of problems between 2015 and 2019. Of those, 47 came from healthcare professionals. Symptoms? Fatigue (78%), headaches (65%), anxiety (47%), and weight gain (33%). Only 27 of those cases had thyroid tests done - meaning most people were being blamed for “not trying hard enough” when their body was reacting to a new pill.
Thyroid UK surveyed 1,245 people. 68% said they had symptoms after switching brands. One woman wrote: “I was on the same dose. Same pill size. But I started having panic attacks. My doctor said it was stress. I switched back to my old brand - and within two weeks, I was myself again.”
If you’ve ever felt worse after a pharmacy refill - even if the label says the same thing - tell your doctor. Ask them to specify the brand on your prescription. You’re not being difficult. You’re being smart.
How to Take It Right - And What to Avoid
Levothyroxine isn’t like a vitamin you can swallow with coffee. It needs an empty stomach. Take it at least 30-60 minutes before breakfast. Don’t take it with:
- Calcium supplements
- Iron tablets
- Antacids (like Tums or Gaviscon)
- Cholesterol drugs (like cholestyramine)
- Soy milk or high-fiber meals
These can block absorption. Even a cup of coffee can reduce uptake by 30%. Wait at least 4 hours after taking levothyroxine before taking any of these. If you’re on multiple supplements, talk to your pharmacist. They can help you build a schedule that works.
Who Needs Extra Care?
Some people need specialist input - not just a GP. You should be referred to an endocrinologist if you’re:
- Under 16
- Pregnant or recently had a baby
- Have heart disease, especially if you’ve had a heart attack
- Take amiodarone or lithium
- Have pituitary or adrenal gland problems
Pregnant women need TSH checked every 4 weeks in the first half of pregnancy. Hormone needs jump by 30-50%. If you’re planning pregnancy, get tested before you conceive. Many women don’t realize their dose needs to change - and end up with complications.

What If You Still Don’t Feel Right?
90% of people feel better once their dose is right. But 10-15% still have symptoms like brain fog, muscle pain, or depression - even with normal TSH.
That doesn’t mean you’re imagining it. Research shows some people don’t convert T4 to T3 (the active hormone) efficiently. Your doctor might consider adding liothyronine (T3) - but only after ruling out other causes like vitamin D deficiency, sleep apnea, or depression.
Don’t push for T3 unless your doctor agrees. It’s not a magic fix. It’s a tool - and it comes with risks. But if you’ve tried everything else and still feel awful, ask for a referral to an endocrinologist who specializes in thyroid disorders.
The Big Picture: You’re Not Alone - But You Need to Advocate
One in 20 adults in the UK has hypothyroidism. That’s over 2.5 million people. Yet NHS data shows only 58% of practices follow the recommended monitoring schedule. One in three patients goes more than 18 months without a TSH test.
You don’t need to be a medical expert to manage this. But you do need to be your own best advocate. Keep a log: when you took your pill, when you had your blood test, what your dose was, and how you felt. Bring it to appointments. Ask: “Is my TSH in the right range for me?” “Could my brand be causing this?” “When should I test next?”
Levothyroxine is safe. But safety isn’t automatic. It’s earned - through testing, consistency, and communication.
What to Do If You Suspect a Problem
If you notice new or worsening symptoms after a refill - fatigue, heart racing, unexplained weight changes - don’t wait. Take action:
- Check your pill. Is it a different color, shape, or name? Write it down.
- Book a TSH test immediately. Don’t wait for your next appointment.
- Ask your GP to specify the brand on your prescription: “Dispense as written.”
- If symptoms persist, request a referral to an endocrinologist.
- Report it to the MHRA’s Yellow Card scheme. Your report helps others.
There’s no shame in needing help. This isn’t about being difficult. It’s about staying healthy.





12 Comments
Levothyroxine isn't magic. It's a hormone replacement that requires lab work like any other endocrine therapy. If you're not getting tested every 6 months, you're just guessing. And no, 'feeling fine' doesn't mean your TSH is optimal - it means you're lucky. Most GPs don't get it. They treat TSH like a light switch, not a dial.
Also, brand switching? That's a silent epidemic. I've seen patients crash after a pharmacy swap. No one checks free T4 or reverse T3. Just TSH. Pathetic.
I switched brands last year and got panic attacks for weeks. My doctor said it was anxiety. I switched back. Two weeks later, I slept through the night for the first time in years.
They don't tell you this, but levothyroxine is basically a slow poison if you're not monitored. You think you're fixed until your bones start crumbling or your heart starts fluttering like a trapped bird. And then they blame your diet, your stress, your 'lifestyle choices'.
I've been on it for 12 years. I've had four different brands. Each one felt like a different person living in my skin. I stopped trusting doctors after the third time they told me I was 'overreacting'.
There's something deeply human about needing a tiny pill to keep your body from shutting down. Levothyroxine doesn't just replace a hormone - it restores dignity. It lets you wake up without feeling like you're dragging cement through your veins.
But the system treats it like aspirin. You get a script, you take it, and you're expected to be fine. No questions asked. No follow-up required. As if your thyroid were a broken lightbulb you just swap out.
It's not. It's a symphony. And if one instrument is out of tune - even slightly - the whole piece falls apart. And we're not even talking about T3 conversion, or adrenal fatigue, or vitamin D deficiency masquerading as 'resistant hypothyroidism'.
We're talking about a medical culture that reduces complex physiology to a single number on a page. And then wonders why people still feel awful.
Maybe the problem isn't the patient. Maybe it's the paradigm.
Let’s be clear: if your GP isn’t ordering TSH every 6–12 months, they’re negligent. The guidelines are clear. The evidence is overwhelming. And yet, 1 in 3 patients go over 18 months without testing? That’s not incompetence - it’s systemic abandonment.
Brand switching is equally criminal. The MHRA data is damning. 68% of patients report symptoms after a switch. Yet pharmacists are still allowed to swap brands unless explicitly told not to. That’s not efficiency - it’s patient exploitation disguised as cost-saving.
And coffee? Yes, coffee reduces absorption by 30%. I’ve seen patients on the same dose, same brand, same schedule - but they drink their pill with their morning latte. Of course they’re symptomatic. It’s not the drug. It’s the ritual.
While I appreciate the anecdotal nature of this post, I must emphasize that the statistical reliability of self-reported symptom changes following brand substitution is methodologically unsound. Without controlled, double-blind, crossover trials with serum biomarker correlation, these narratives constitute confirmation bias at best and therapeutic nihilism at worst.
Furthermore, the assertion that TSH targets should be individualized lacks robust longitudinal validation across diverse populations. The 0.5–4.5 mIU/L range remains the standard for good reason: it minimizes population-level risk.
Patients who report persistent symptoms despite euthyroid TSH levels should be evaluated for somatoform disorders, not biochemical reconfiguration.
I’ve been on levothyroxine for 8 years. I take it at 6 a.m., no coffee for an hour, no calcium, no soy. I get tested every 6 months. I feel great. But I know people who don’t. And I don’t judge them. I just wish more doctors would listen.
One friend switched brands and started crying for no reason. Her doctor said she was ‘just depressed.’ She switched back. Cried stopped. TSH was normal both times. That’s not depression. That’s pharmacology.
My mom’s been on this for 15 years. She’s 72. Her TSH is 6.8. Her doctor says it’s fine because she’s older. She still feels like a zombie. I asked if they’d tried lowering it. They said ‘no need.’
I just wish people would stop assuming age = less need. She’s active, walks 5 miles a day, reads books. She shouldn’t feel like she’s running on batteries half-dead.
Big Pharma doesn't want you to know this, but levothyroxine is a gateway drug to lifelong dependency. They make you think you need it forever, then charge you $400 a year for it. Meanwhile, the real cure? Fasting. Cold exposure. Healing your gut. But nope - take the pill. Keep paying.
And don't get me started on TSH. That number is manipulated. The 'normal range' was expanded in the 90s so more people could be diagnosed. More pills. More profits.
My cousin went off it cold turkey and now she's 'reclaimed her energy.' Coincidence? I think not.
thyroid is not just tsh bro. u need ft3 ft4 also. most docz are lazy. they see tsh 2.5 and say u good. but if ft3 is low u still tired. its not about tsh alone. its about conversion. its about mitochondria. its about the soul.
People who complain about brand switching are just lazy. If you can’t remember to take your pill properly, don’t blame the pharmacy. And if you’re still tired after 6 months on levothyroxine, maybe you’re just depressed. Or fat. Or sleep-deprived. Or all three.
Stop looking for external causes. Take responsibility. Your thyroid isn’t broken - your discipline is.
Levothyroxine is the most overprescribed drug in modern medicine. 90% of people on it don’t even need it. They were misdiagnosed because their doctor didn’t check for Hashimoto’s antibodies or vitamin deficiencies.
And now we’ve created a generation of people who think they can’t function without a synthetic hormone. Pathetic. Just eat more eggs. Sleep more. Stop drinking soy milk.
Write a comment