Vaginal Burning Symptom Checker
This tool helps identify potential causes of vaginal burning related to diaphragm use based on your symptoms. Note: This is not a medical diagnosis tool. Always consult a healthcare provider for proper medical advice.
When does the burning sensation typically occur?
What type of discharge do you notice?
Do you experience other symptoms?
What type of diaphragm do you use?
Do you use spermicide with your diaphragm?
Possible Cause
Recommended Actions
Quick Takeaways
- Diaphragms can trap moisture and alter vaginal pH, leading to irritation.
- Common culprits include bacterial vaginosis, yeast infection, and chemical irritants from spermicide.
- Gentle hygiene, breathable materials, and proper fitting reduce risk.
- Seek medical advice if burning persists for more than a few days or is accompanied by discharge or fever.
- Alternative contraceptives may be a better fit if you experience recurring symptoms.
When the sensation of vaginal burning shows up while you’re using a diaphragm, it can feel confusing and uncomfortable. This guide walks you through why it happens, how to tell what’s causing it, and what steps you can take right now to feel better.
What Is Vaginal Burning?
Vaginal burning is a sharp, tingling or painful sensation that may occur on the vulva, inside the vaginal canal, or both. It’s often accompanied by itching, redness, or unusual discharge. The feeling can be fleeting-lasting minutes after intercourse-or chronic, persisting day after day.
Because the vagina maintains a delicate balance of moisture, temperature, and pH (normally around 3.8‑4.5), any disruption can trigger the nerves in the area, producing that burning feeling.
Why Diaphragms Matter
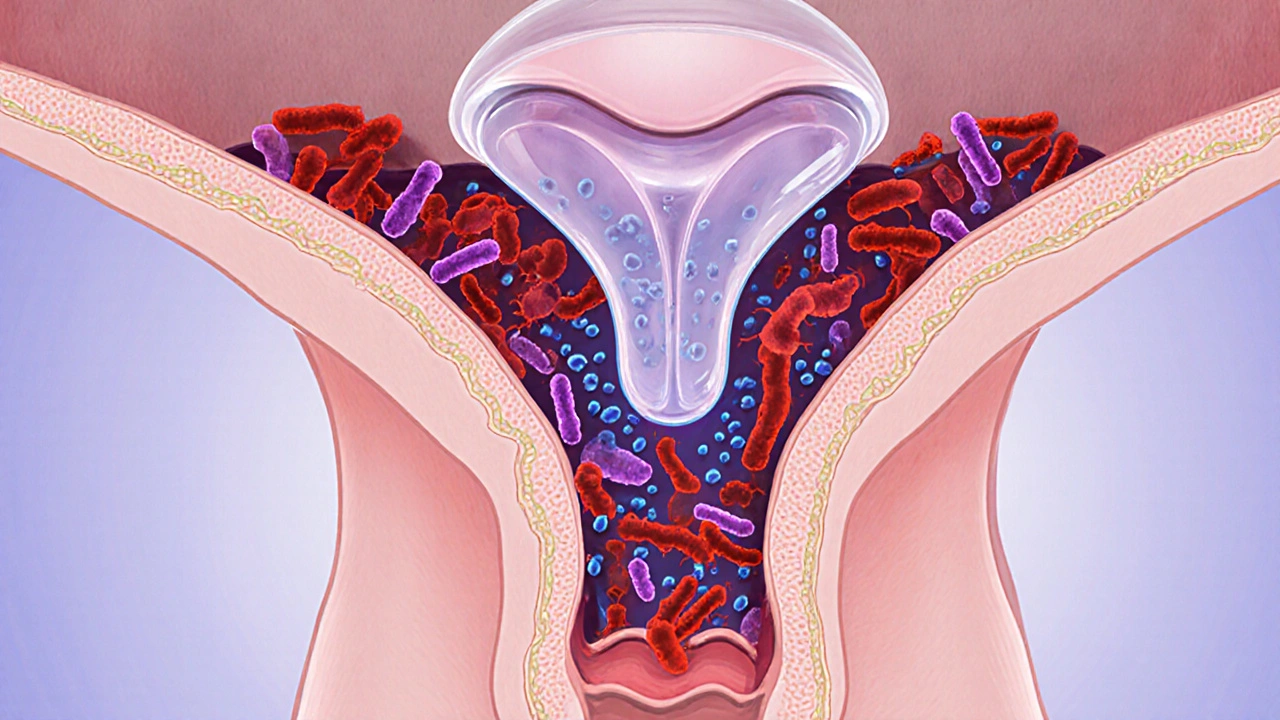
Diaphragm contraceptive is a flexible, dome‑shaped silicone or latex barrier that sits over the cervix. It must be used with a spermicide-typically a nonoxynol‑9 gel-to block sperm.
While diaphragms are praised for being hormone‑free and reusable, they also create a sealed environment that can trap heat, moisture, and chemicals. Over time, that sealed pocket may shift the vaginal pH, encouraging the growth of harmful microbes.
Common Causes of Burning Linked to Diaphragm Use
- Bacterial vaginosis - an overgrowth of anaerobic bacteria that thrives in a higher pH. Symptoms include a thin, grayish discharge and a fishy odor, often paired with mild burning.
- Yeast infection - caused by Candida albicans. The yeast loves warm, moist environments, so a diaphragm that isn’t cleaned properly can feed it. Look for thick, white “cheese‑curd” discharge and intense itching.
- Irritant dermatitis - chemical irritation from spermicide (especially nonoxynol‑9), latex allergies, or scented lubricants. The result is redness, swelling, and a burning sting.
- pH imbalance - the diaphragm can raise vaginal pH, making it less acidic and more hospitable to pathogens.
- Improper fit - a diaphragm that’s too tight can compress tissue, reducing blood flow and causing friction‑related burning.
How to Diagnose the Source
Self‑assessment can point you in the right direction, but a quick visit to a clinician confirms the diagnosis.
- Note the timing: Does burning appear right after you insert or remove the diaphragm? Or does it develop hours later?
- Check discharge: Color, consistency, and odor are key clues for bacterial vaginosis or yeast infection.
- Inspect the diaphragm: Look for tears, discoloration, or a strong chemical smell that might indicate spermicide degradation.
- Consider recent changes: New lubricants, a switch to a different brand of spermicide, or a recent soap change can all be culprits.
- Schedule a pelvic exam: A healthcare provider can take a swab for microscopic analysis and test the pH directly.
Immediate Relief Strategies
- Cool compress: Apply a clean, cool washcloth to the outer vulva for 5‑10 minutes. It soothes nerve endings without disrupting the internal environment.
- Gentle cleansing: Use warm water only-no soaps, douches, or scented wipes. Pat dry with a soft towel.
- Avoid irritants: Switch to a fragrance‑free, silicone‑based lubricant if you need extra moisture. Avoid spermicides that contain nonoxynol‑9; consider a spermicide‑free diaphragm if your doctor says it’s safe.
- Probiotic support: Daily oral probiotic strains such as Lactobacillus rhamnosus can help restore healthy vaginal flora.
- OTC creams: Over‑the‑counter antifungal creams (e.g., clotrimazole) are effective for confirmed yeast infections. For bacterial vaginosis, a prescription of metronidazole is usually required.

Long‑Term Prevention
Portion of prevention is about habits; the other part is choosing the right contraceptive method for your body.
- Fit check: Have a healthcare professional measure your cervical diameter annually. An ill‑fitting diaphragm is a frequent source of irritation.
- Clean properly: After each use, rinse the diaphragm with warm water, wash with mild soap, and air‑dry it completely before storage.
- Replace regularly: Most diaphragms last 1‑2 years. Look for signs of wear-tiny holes, stiffness, or discoloration.
- Consider alternatives: If burning recurs despite good care, explore hormone‑free options like a copper IUD, or barrier methods such as condoms paired with a spermicide‑free lubricant.
- Track symptoms: Keep a short diary of when burning occurs, what you ate, any new products, and menstrual cycle phase. Patterns often emerge that point to triggers.
Comparison of Common Contraceptives and Their Irritation Risks
| Method | Typical Use Failure Rate | Potential Irritation Causes | Best For |
|---|---|---|---|
| Diaphragm + spermicide | 12% | pH shift, chemical irritation, fit issues | Hormone‑free users who can fit diaphragm correctly |
| Birth‑control pill | 7% | Systemic hormonal changes (rarely cause burning) | Those wanting regular menstrual regulation |
| Copper IUD | 0.8% | Initial spotting, rare allergic reaction to copper | Long‑term, hormone‑free users |
| Male condom | 13% | Latex allergy, friction, scented lubricants | Couples needing STI protection |
| Female condom | 21% | Material sensitivity, insertion discomfort | Those preferring female‑controlled barrier |
When to See a Healthcare Provider
If any of the following apply, schedule an appointment promptly:
- The burning lasts longer than 48 hours despite home care.
- You notice a foul‑smelling, grayish discharge (sign of bacterial vaginosis).
- There’s thick, white discharge with intense itching (possible yeast infection).
- You develop fever, pelvic pain, or pain during urination-these could signal a more serious infection.
- You suspect an allergic reaction to latex or spermicide.
Early treatment prevents complications like pelvic inflammatory disease (PID) and helps you get back to feeling comfortable.
Frequently Asked Questions
Can I still use a diaphragm if I have a latex allergy?
Yes-many manufacturers offer silicone‑based diaphragms that are latex‑free. Make sure the product is explicitly labeled “latex‑free” and get a professional fit.
Is nonoxynol‑9 spermicide the main cause of irritation?
Nonoxynol‑9 can disrupt the natural flora and lower the protective acidity, leading to both bacterial vaginosis and yeast infections. Switching to a spermicide‑free diaphragm (if your doctor approves) often eliminates the burning.
How often should I replace my diaphragm?
Typically every 1‑2 years, or sooner if you notice cracks, stiffness, or discoloration. Regular replacement maintains both effectiveness and comfort.
What home remedy can help restore vaginal pH?
A daily probiotic containing Lactobacillus strains, combined with plain unsweetened yogurt applied externally (not intravaginally), can help rebalance acidity. Always discuss with a clinician before starting any regimen.
Should I stop using a diaphragm completely if I experience burning?
Pause use until you identify the cause. If the burning is linked to spermicide or fit, switching to a different barrier method or a hormone‑free option like a copper IUD may be safer.
Understanding the link between diaphragms and vaginal burning puts you in control of your comfort and health. By checking fit, keeping the device clean, and knowing when to seek professional help, you can enjoy effective contraception without the unwanted sting.






10 Comments
It is imperative to recognize that the diaphragm, while a commendable hormone‑free contraceptive, can inadvertently disrupt the delicate vaginal ecosystem. The device creates a sealed micro‑environment which may elevate pH, fostering bacterial overgrowth. Moreover, the presence of nonoxynol‑9 spermicide introduces a chemical irritant that can compromise the mucosal barrier. An ill‑fitting diaphragm exerts undue pressure on the vulvar tissue, precipitating friction‑induced erythema and a burning sensation. Clinical guidelines advise a meticulous fit assessment annually, as cervical diameter may fluctuate with age and hormonal cycles. Rigorous cleansing after each intercourse-warm water, mild unscented soap, and thorough air‑drying-mitigates residual moisture that serves as a fungal substrate. Should symptoms persist beyond 48 hours, a pelvic examination with pH testing and microscopy is warranted to differentiate between candidiasis, bacterial vaginosis, or irritant dermatitis. Probiotic supplementation, particularly Lactobacillus rhamnosus, can assist in re‑establishing an acidic milieu, yet it should complement, not replace, professional evaluation. Lastly, patients experiencing recurrent burning are encouraged to explore alternative barriers, such as a silicone‑only diaphragm or a copper intrauterine device, to obviate the offending agents.
Philosophically, a barrier that burns undermines its purpose.
The article nails the basics but somehow skips the glaring fact that many users simply ignore the manufacturer’s cleaning instructions out of laziness, which is a primary driver of fungal proliferation. While the guide mentions probiotic use, it fails to emphasize that oral probiotics are not a substitute for proper hygiene. Also, the table comparing contraceptives lacks any mention of device lifespan, a critical omission for cost‑conscious readers. In short, the piece is informative yet overly polite about user negligence.
Hey, don’t worry – you’re not alone in missing a step or two. A quick rinse with warm water and letting the diaphragm dry fully can make a huge difference, and it’s never too late to start a simple daily habit.
Honestly, if you keep ignoring the fit guidelines and still blame the diaphragm for burning, you’re just looking for an excuse to avoid responsibility. A proper fit isn’t optional; it’s the foundation of comfort and safety.
What most people don’t realize is that the spermicide’s active ingredient, nonoxynol‑9, is deliberately engineered to compromise epithelial defenses, making the whole system vulnerable to opportunistic microbes – a fact the pharmaceutical industry conveniently downplays.
Let’s get proactive: grab a cool compress, give the area a gentle rinse, and schedule that doctor’s visit within the week. You’ve got the power to break the cycle and keep your health on track.
Ah yes, because a humble ice pack and a whispered “I’ll be fine” magically cure micro‑environmental imbalances – truly groundbreaking medical advice.
First, stop assuming every burning sensation means an infection; sometimes it’s simply friction from an over‑tight diaphragm then second, make sure you’re not using an expired spermicide because the preservative breakdown can irritate the mucosa because always inspect the device for tiny tears or discoloration before each use remember that the vaginal flora is resilient but can be thrown off by repeated moisture retention a quick rinse with warm water and a thorough air‑dry eliminates most fungal spores if you notice a grayish discharge with a fishy smell you’re likely dealing with bacterial vaginosis thick white clumpy discharge paired with itching points to candidiasis both conditions require targeted treatment – metronidazole for BV and clotrimazole for yeast don’t self‑diagnose long‑term symptoms; a pelvic exam with a pH test is the gold standard consider swapping to a silicone‑only diaphragm if latex or spermicide seems to be the trigger keep a symptom diary noting timing, diet, and product changes this pattern often reveals hidden irritants finally, if burning persists beyond two days despite these measures, seek professional care early intervention prevents complications like PID and ensures you stay comfortable and protected.
Wow-what an exhaustive checklist!; you’ve covered every angle and made it easy to follow; thanks for the thorough rundown; I’ll definitely keep a diary and check the fit next month; feeling more confident already!.
Write a comment