When a drug’s patent runs out, prices don’t just drop-they crash. For patients, that could mean paying 80% less for the same medicine. For hospitals and insurers, it’s a chance to save millions. But none of this happens automatically. If you’re on a long-term medication-or manage care for others-you need to start planning patent expiry at least two years before it happens. Waiting means confusion, disruptions, and higher costs.
Why Patent Expiry Isn’t Just a Business Problem
Most people think patent expiry is something that happens in boardrooms. But it hits real people. Take someone on Humira for rheumatoid arthritis. In 2023, Humira’s patent expired in the U.S., but because of complex patent thickets and legal delays, generic versions didn’t arrive until 2024. Even then, many patients were switched to a biosimilar without understanding the difference. Some reported new side effects. Others couldn’t get the same dosage form. That’s not rare. A 2022 Kaiser Family Foundation survey found 37% of patients on chronic meds had adverse reactions after switching to generics-even though they met FDA bioequivalence standards. The truth is, patent expiry isn’t just about cost. It’s about stability. When a brand-name drug loses exclusivity, multiple generic versions flood the market. Some are identical. Others have different inactive ingredients-fillers, dyes, coatings-that can affect how your body absorbs the drug. If you’re on a narrow-therapeutic-index drug like warfarin or levothyroxine, even small changes can be dangerous.What Happens When a Patent Expires?
The clock starts ticking when a drug is first filed for patent protection. That’s usually years before it hits shelves. By the time it’s approved by the FDA, only 7 to 10 years of market exclusivity remain. That’s why companies use tricks to stretch that time: new formulations, combo pills, micro-dosing, or even changing the delivery method (like switching from a pill to an injection). These are called “evergreening” tactics. Nearly 80% of the top 100 selling drugs have over a dozen secondary patents, according to Evernorth’s 2023 analysis. When the main patent finally falls, generic manufacturers can step in. But they don’t always rush. For small-molecule drugs-like statins or blood pressure pills-generics typically appear within months. Prices drop 70-90% in the first year. But for complex drugs like biologics (used in cancer, autoimmune diseases), it’s different. Biosimilars take years to develop. They’re not exact copies. They’re similar, but harder to make. Only 38% of biologic prescriptions switch to biosimilars within two years, even after patent expiry. And here’s the catch: even when generics arrive, the price you pay doesn’t always drop. In the U.S., rebates, pharmacy benefit manager deals, and formulary restrictions mean you might still be stuck paying high prices-even if the drug now costs $5 a pill wholesale.What Patients Should Do
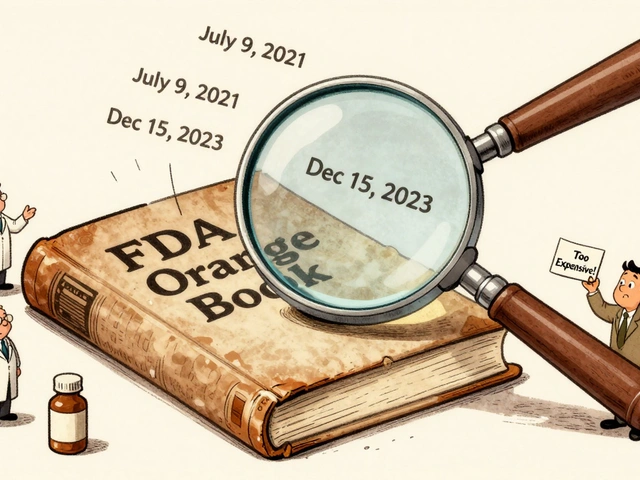
If you’re taking a medication that’s due to lose patent protection, here’s what to do now:- Find out when your drug’s patent expires. Use the FDA’s Orange Book or ask your pharmacist. Many drugs have public expiry dates listed on sites like GoodRx or Drugs.com.
- Ask if a generic or biosimilar is available. Don’t assume your doctor or pharmacy will bring it up. Bring it up yourself. Say: “Is there a lower-cost version coming soon?”
- Know your options if you’re switched. If your insurer switches you to a generic, ask: “Is this the same as my current drug?” and “Can I stay on the brand if I need to?” Some generics have different dosing or delivery systems.
- Monitor for side effects. If you feel different after switching-more fatigue, nausea, or mood changes-tell your doctor immediately. It’s not “all in your head.” Bioequivalence doesn’t mean identical experience.
- Check your out-of-pocket costs. Sometimes, the generic is cheaper, but your copay stays the same because of how your plan tiers drugs. Ask your insurer for the net cost after rebates.

What Healthcare Systems Must Do
Hospitals, insurers, and clinics can’t wait until the last minute. The most successful ones start planning 24 months ahead. Here’s how:- Build a patent expiry task force. Include pharmacists, clinicians, finance staff, and contract managers. Track every drug with an upcoming expiry-there are over 1,400 in the U.S. each year.
- Forecast the impact. Not all drugs are equal. Cardiovascular drugs see 90% generic adoption. Immune drugs? Less than 50%. Prioritize high-cost, high-volume medications first.
- Negotiate with suppliers early. Generic manufacturers often offer deep discounts before launch. Lock in those prices before the market floods.
- Update clinical guidelines. Don’t let doctors guess what to prescribe. Create clear protocols for switching patients. Include when to avoid substitution (e.g., epilepsy, transplant meds).
- Train staff and educate patients. Create simple handouts. Host Q&A sessions. Use your patient portal to send alerts. People need to understand why the change is happening-and that it’s safe.
The Big Gap: Biosimilars Are Slowing Down Savings
The biggest missed opportunity? Biosimilars. Drugs like Enbrel, Remicade, and Rituxan are losing patents now. These are biologics-expensive, complex, injectable drugs used for cancer, Crohn’s, and psoriasis. They cost $20,000-$50,000 a year. Biosimilars should cut that by 50%. But they haven’t. Why? Because manufacturers use tactics to block them: exclusive contracts with pharmacies, rebates that make biosimilars look more expensive, and even paying insurers to keep the brand on top. Only 27% of biologic prescriptions have switched to biosimilars in the U.S.-compared to over 90% for simple generics. Europe does better. Countries with reference pricing (where all similar drugs are grouped and priced together) see 85% biosimilar use within a year. The U.S. doesn’t have that system. So change has to come from within hospitals and insurers pushing for biosimilar adoption.
What’s Changing in 2026 and Beyond
The Inflation Reduction Act of 2022 gave Medicare the power to negotiate drug prices-but only for drugs that have been on the market for at least 9 years. That means the first round of negotiated prices kicks in for drugs losing patent protection in 2026. That’s happening right now. Also, the FDA’s new GDUFA III rules are speeding up approvals for complex generics. Some drugs that used to take 18 months to get generics after patent expiry will now get them in 12. And the CREATES Act is cracking down on “product hopping”-where companies tweak a drug just to reset the patent clock. AI tools are helping too. Health systems using AI to predict patent expirations are now forecasting with 89% accuracy-up from 65%. That means fewer surprises.Don’t Wait for the Crash
Patent expiry isn’t a future problem. It’s happening now. In 2025-2029, over $90 billion in U.S. drug sales will lose patent protection. That’s enough to cover free prescriptions for millions. But only if we plan. Patients: Don’t assume your drug will stay the same. Ask questions. Track your meds. Know your rights. Systems: Start planning now. Build teams. Track expirations. Educate. Negotiate. The savings aren’t theoretical-they’re real. One health system saved $4.7 million per drug by starting 24 months early. Those who waited saved less-and lost patients to confusion. The patent cliff isn’t coming. It’s here. The question isn’t whether you’ll be affected. It’s whether you’re ready.What does patent expiry mean for my prescription drug?
When a drug’s patent expires, other companies can legally make and sell generic or biosimilar versions. These are usually much cheaper-often 80% less than the brand-name version. But you might be switched automatically, and not all generics are identical. Some have different fillers or delivery methods that can affect how you feel.
Can I stay on my brand-name drug after the patent expires?
Yes, but it may cost more. Insurance plans often shift coverage to generics after patent expiry. If you want to keep the brand, you might have to pay the full price out-of-pocket or get a prior authorization from your doctor. Talk to your pharmacist or insurer before the switch happens.
Why do some generics make me feel worse than the brand?
Generics must be bioequivalent-meaning they deliver the same amount of active ingredient. But they can have different inactive ingredients like dyes, preservatives, or coatings. For some people, especially those with sensitivities or chronic conditions, those differences can cause side effects. If you notice changes after switching, report them to your doctor.
What’s the difference between a generic and a biosimilar?
Generics are exact copies of small-molecule drugs, like pills for blood pressure or cholesterol. Biosimilars are similar-but not identical-to complex biologic drugs, like injectables for arthritis or cancer. They’re harder to make, take longer to approve, and cost more than generics. They’re not interchangeable unless specifically approved by the FDA.
How far in advance should I plan for patent expiry?
Patients should start asking questions 6-12 months before the patent expires. Healthcare systems need to begin planning 24 months ahead. That’s when they can lock in pricing, update guidelines, train staff, and prepare patient materials. Waiting until the last minute leads to disruptions and higher costs.
Are there tools to track when my drug’s patent expires?
Yes. The FDA’s Orange Book lists patent expiry dates for approved drugs. Websites like GoodRx, Drugs.com, and Lexicomp also track this. Health systems use specialized software like Symphony Health’s PatentSight to monitor hundreds of expirations at once.
Why don’t all countries have the same drug prices after patent expiry?
Countries like Germany and the UK use reference pricing, where all similar drugs are grouped and priced together. That forces generics and biosimilars to compete on price. The U.S. doesn’t have that system. Instead, rebates and pharmacy benefit managers control pricing, which often keeps prices higher longer-even after generics arrive.
Will the Inflation Reduction Act lower my drug prices after patent expiry?
Starting in 2026, Medicare will begin negotiating prices for a small number of high-cost drugs that have been on the market for at least 9 years. These are mostly drugs losing patent protection around that time. It won’t affect all drugs, but it will lower prices for some of the most expensive ones, especially biologics.