Bipolar Disorder Treatment: What Works and How to Start
If you or someone you know lives with bipolar disorder, the first step is figuring out what helps keep the highs and lows from taking over daily life. Below you’ll find the most common meds, therapy choices, and everyday habits that actually make a difference.
Medication Options
The backbone of most treatment plans is medication. Mood stabilizers like lithium, valproate, and carbamazepine are the go‑to drugs for many doctors. They smooth out extreme mood swings and lower the risk of relapse.
Second‑generation antipsychotics such as quetiapine, lurasidone, and olanzapine are often added when mania or depression stay strong despite a mood stabilizer. They work fast and can be a good bridge while waiting for the main drug to kick in.
Antidepressants are a tricky part of the puzzle. They can lift depressive symptoms, but they sometimes trigger mania if used alone. Most clinicians pair them with a mood stabilizer to keep things safe.
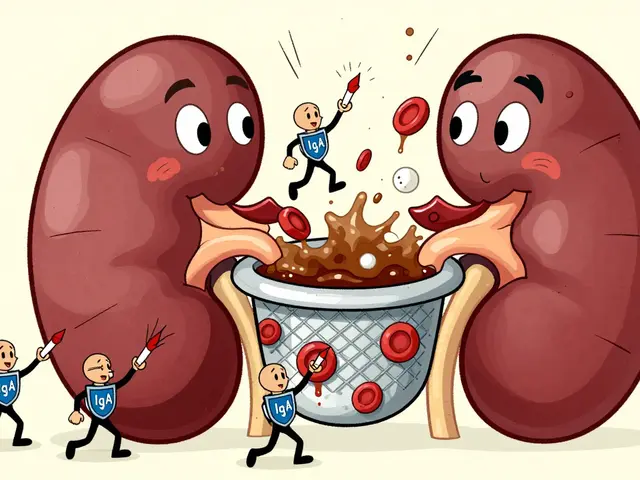
Every drug has side‑effects. Lithium can affect kidney function, valproate may cause weight gain, and antipsychotics can raise blood sugar. Regular blood tests and check‑ups keep you ahead of any problems.
Non‑Medication Strategies
Medication isn’t the whole story. Cognitive‑behavioral therapy (CBT) helps you notice early warning signs and change harmful thinking patterns. A structured CBT program can cut relapse rates by up to 40%.
Interpersonal and Social Rhythm Therapy (IPSRT) focuses on keeping daily routines steady—same wake‑up time, meals, and sleep schedule. Consistency makes the brain’s internal clock less likely to spark mood spikes.
Support groups give you a safe place to share experiences. Hearing how others manage triggers, meds, and side‑effects can save you a lot of trial and error.
Exercise isn’t a cure, but regular activity lifts mood, improves sleep, and reduces anxiety. Even a brisk 20‑minute walk three times a week shows measurable benefits.
Nutrition matters, too. Reducing sugary drinks, staying hydrated, and eating balanced meals with protein and healthy fats can smooth energy swings. Some people find omega‑3 supplements helpful, though the evidence is mixed.
Sleep hygiene is critical. Aim for 7‑9 hours, keep the bedroom dark, and avoid screens an hour before bed. If insomnia pops up, talk to your doctor before using over‑the‑counter sleep aids.
Stress management tools—mindfulness, deep breathing, or short meditation sessions—lower the chance of a manic or depressive episode. Start with five minutes a day and build up.
Lastly, keep a mood journal. Write down how you feel, what you ate, how much you slept, and any stressful events. Over weeks, patterns emerge that help you and your clinician fine‑tune treatment.
Putting all these pieces together—meds that fit, therapy that teaches coping, and daily habits that stabilize—creates a solid foundation for living with bipolar disorder. Talk with your doctor about which combination feels right for you, and remember that adjustments are normal as you find what works best.

Divalproex Dosage Guide: How to Find Your Right Dose
- By : Tamsin Riverton
- Date : Aug 11 2025
Learn how to determine the correct Divalproex dosage for epilepsy, bipolar disorder, or migraine, with clear dosing ranges, safety tips, and monitoring guidelines.