Fluoroquinolone Antibiotics – Quick Guide
Did you know fluoroquinolones are some of the strongest antibiotics on the market, yet they also spark the most safety debates? If you’ve been prescribed one or are just curious, this guide breaks down what they are, how they work, when they’re needed, and what to watch out for. No jargon, just the facts you need to feel confident about your treatment.
How fluoroquinolones work
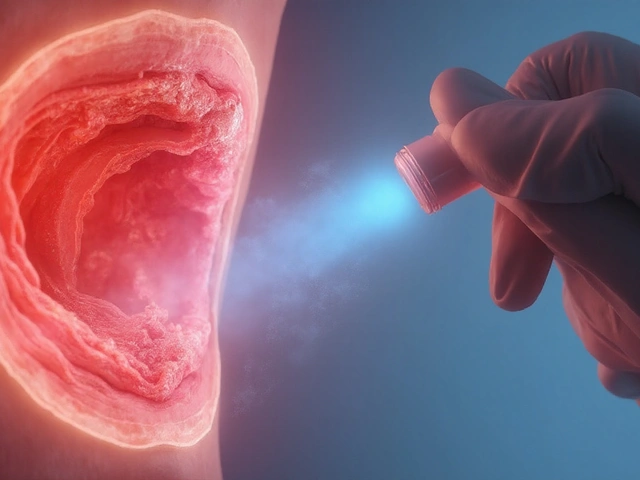
Fluoroquinolones target bacterial DNA by blocking two key enzymes – DNA gyrase and topoisomerase IV. Those enzymes help bacteria copy their genetic material, so when they’re blocked, the bugs can’t multiply and eventually die off. This mechanism makes the drugs effective against a wide range of gram‑negative and some gram‑positive bacteria, which is why doctors often reach for them in tougher infections.
When to use and when to avoid
Typical uses include urinary‑tract infections, certain types of pneumonia, skin infections, and gastrointestinal bugs like traveler's diarrhea. They’re also a go‑to for complicated sinus or ear infections when other antibiotics haven’t worked. However, they’re not first‑line for simple infections because the risk profile is higher. Pregnant women, children, and people with a history of tendon problems should steer clear unless no other option exists.
Side effects can feel minor at first – nausea, headache, or mild dizziness – but the serious ones deserve attention. Tendon rupture, especially in the Achilles, has been linked to fluoroquinolones and can happen weeks after therapy ends. Nerve damage causing tingling or numbness (peripheral neuropathy) is another warning sign that shouldn’t be ignored.
Drug interactions are common. Antacids containing magnesium or aluminum, as well as supplements with calcium or iron, can bind to the antibiotic and cut its effectiveness. If you need those for other reasons, take the fluoroquinolone at least two hours before or six hours after the antacid.
Because the liver processes many fluoroquinolones, people with severe liver disease may need dose adjustments. Kidney function also matters; if your kidneys aren’t working well, the drug can build up and cause more side effects. Your doctor will likely order a blood test to check these organs before starting treatment.
The FDA has issued several safety alerts over the years, urging prescribers to limit use to patients who truly need them and have no safer alternatives. These alerts also recommend a short treatment duration – usually five days or less – to cut down on the chance of serious side effects.
Practical safety tips: stay hydrated, avoid intense physical activity that stresses your tendons while you’re on the medication, and report any sudden joint pain or numbness right away. If you notice vision changes, heart palpitations, or severe diarrhea, seek medical help immediately.
In short, fluoroquinolones can be life‑saving when used correctly, but they require careful monitoring. Always discuss the benefits and risks with your healthcare provider, and don’t hesitate to ask about alternative antibiotics if you have concerns. Knowing the facts helps you and your doctor make the best choice for your health.

Norfloxacin’s Role in Treating Recurrent Urinary Tract Infections
- By : Tamsin Riverton
- Date : Aug 1 2025
Explore how norfloxacin works, when it’s suitable for recurrent UTIs, dosing tips, resistance concerns, and alternatives for safer long‑term care.