Hepatitis C Drug Resistance: Key Facts and What to Do
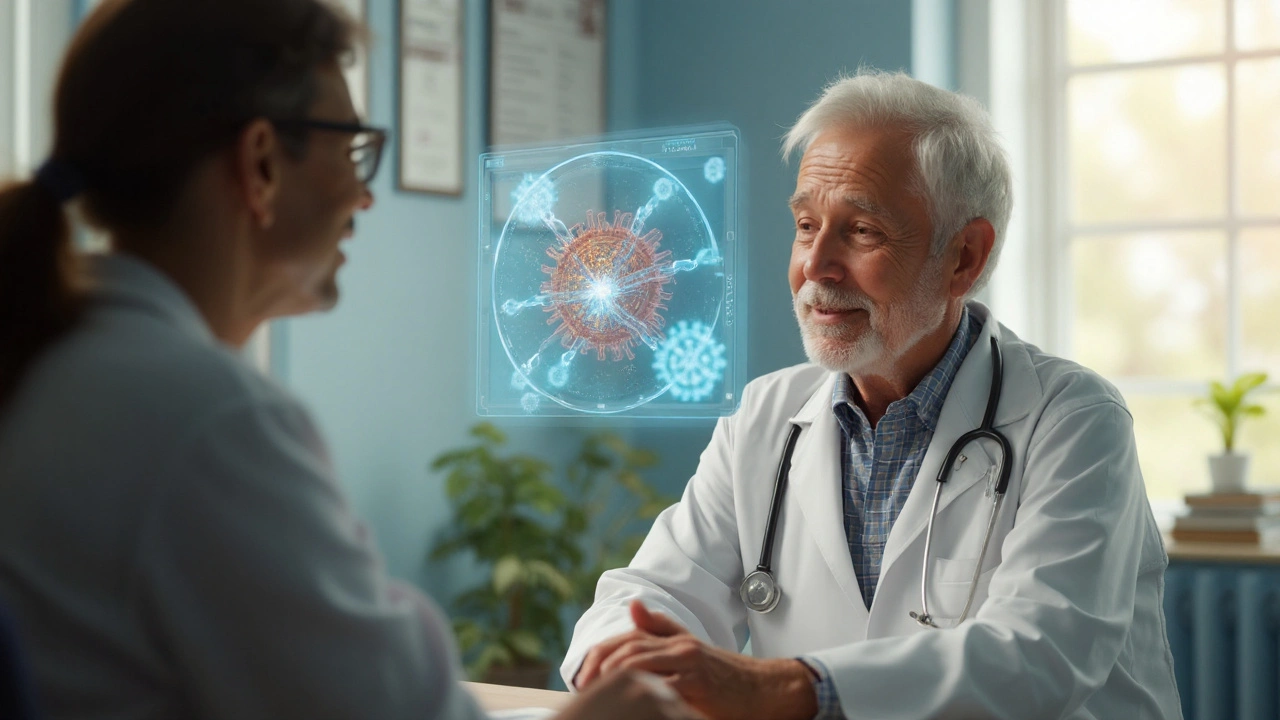
Modern antivirals cure most hepatitis C cases, but a small group of patients hit a wall when the virus stops responding. That’s drug resistance, and it can feel like a setback. The good news? Knowing why it happens and how to tackle it makes the odds swing back in your favor.
Why resistance occurs
Hepatitis C is a fast‑changing virus. Every time it copies itself, it makes tiny mistakes—mutations. Most mutations are harmless, but a few give the virus an edge against a specific drug. When you take a direct‑acting antiviral (DAA), the drug puts pressure on the virus. The few mutated viruses that can survive start to dominate, leading to resistance.
The most common culprits are changes in three viral proteins: NS5A, NS5B, and the NS3/4A protease. A single change in the NS5A region, for example, can make a drug like ledipasvir lose much of its power. That’s why doctors keep an eye on these spots, especially in patients who have already been treated before.
How doctors manage resistant HCV
First step is testing. Before starting therapy, many clinicians order a baseline resistance‑associated substitution (RAS) test. If a patient has already failed a regimen, a repeat RAS test helps pick the next drugs that the virus is still sensitive to.
Once resistance is confirmed, the treatment plan shifts. Doctors may add a second DAA from a different class, extend the treatment length, or throw ribavirin into the mix. For instance, a patient with NS5A resistance might get a protease inhibitor plus sofosbuvir for 24 weeks instead of the usual 12.
Newer DAAs are in late‑stage trials and promise activity against even the toughest RAS patterns. Guidelines from the American Association for the Study of Liver Diseases (AASLD) are updated regularly, giving clinicians a roadmap for retreatment.
For patients, the most practical advice is simple: take every dose on schedule, avoid missed pills, and keep the doctor in the loop about any side effects. If you’re on a DAA and feel unusually sick, call your provider right away—early tweaks can prevent resistance from taking hold.
Another tip is to stay on top of follow‑up labs. After therapy, a viral load test at 12 weeks tells you if the virus is truly gone. A detectable load at that point signals a possible resistant strain, and further testing can guide the next steps.
In short, hepatitis C drug resistance isn’t a dead end. With the right testing, a tailored drug combo, and strict adherence, most patients still achieve a cure. Keep the conversation open with your healthcare team, and don’t hesitate to ask about the latest retreatment options if you hit a snag.
Daclatasvir and Hepatitis C: Patient Guide to Overcoming Drug Resistance
- By : Tamsin Riverton
- Date : Sep 6 2025
A clear, patient‑focused guide explaining how Daclatasvir works, why resistance occurs, and what treatment options exist for Hepatitis C patients facing drug‑resistant virus.