Therapeutic Drug Monitoring – What It Is and Why You Should Care
Ever taken a medication and wondered if the dose is just right? Therapeutic drug monitoring (TDM) answers that question by measuring the amount of a drug in your blood. It helps doctors keep drugs in the sweet spot – high enough to work, low enough to avoid problems. When you hear "TDM" think of a simple blood test that guides safe and effective dosing.
What is Therapeutic Drug Monitoring?
TDM is a tool that checks drug concentrations at specific times after a dose. Some drugs have narrow therapeutic windows, meaning the gap between a good level and a toxic level is small. Antiepileptics, antibiotics like vancomycin, and immunosuppressants are classic examples. By drawing a blood sample, the lab reports a number that the clinician compares to a target range. If the level is below the range, the dose may be increased; if it’s above, the dose is lowered or the dosing interval is changed.
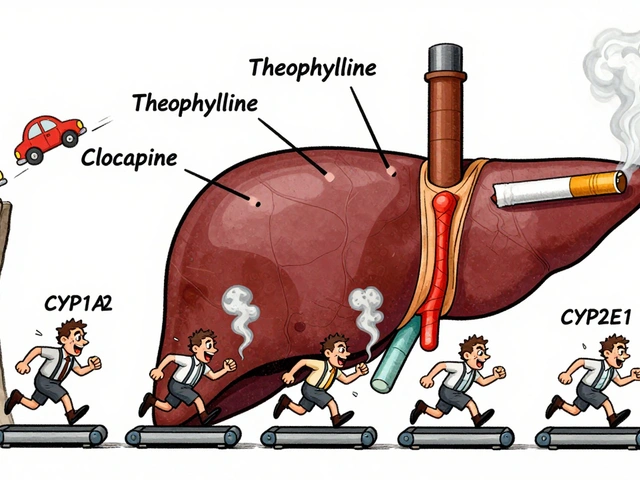
Why not just stick to the label dose? Because many factors shift drug levels – age, kidney function, liver disease, body weight, even genetics. TDM personalizes therapy, turning a one‑size‑fits‑all approach into a patient‑specific plan.
How to Implement TDM in Practice
First, identify drugs that need monitoring. Your clinic’s formulary or a quick check of the drug’s label will tell you if TDM is recommended. Next, schedule the blood draw at the right time. For most drugs, you draw a "trough" sample just before the next dose; for others, a "peak" sample a few hours after dosing is needed. The lab will give you a result in ng/mL or µg/L, along with the therapeutic range.
Once you have the number, interpret it in context. Look at the patient’s kidney and liver labs, current dose, and any other meds that might interact. Adjust the dose incrementally – a 10‑20% change is common – and repeat the level after the new dose reaches steady state, usually after 3‑5 half‑lives of the drug.
Communicate the plan clearly to the patient. Explain why the test matters, what the result means, and how the next dose may differ. This transparency improves adherence and reduces anxiety about blood draws.
For clinicians, integrating TDM into electronic health records can streamline ordering and tracking. Alerts for overdue levels or out‑of‑range results keep the process on schedule. Pharmacists often play a key role, reviewing results and suggesting dose tweaks.
Finally, remember that TDM isn’t a stand‑alone cure. It works best alongside clinical assessment – watch for symptom changes, side‑effects, and lab trends. If a patient feels better and the level sits in the target range, you’ve hit the mark. If not, reassess the dosing schedule, potential drug interactions, or underlying organ function.
Therapeutic drug monitoring may sound technical, but at its core it’s about getting the right amount of medicine to the right person. By using simple blood tests, clear ranges, and step‑by‑step dose tweaks, you can boost treatment success and cut down on adverse events. Give it a try next time you prescribe a drug with a narrow therapeutic window – both you and your patients will thank you.

Divalproex Dosage Guide: How to Find Your Right Dose
- By : Tamsin Riverton
- Date : Aug 11 2025
Learn how to determine the correct Divalproex dosage for epilepsy, bipolar disorder, or migraine, with clear dosing ranges, safety tips, and monitoring guidelines.