When it comes to treating severe osteoporosis, most people think of pills that slow bone loss. But there’s another approach-building new bone. That’s where teriparatide and abaloparatide come in. These aren’t just another drug in a bottle. They’re injectable anabolic agents, designed to stimulate bone formation, not just stop its breakdown. And for people with very low bone density, high fracture risk, or those who haven’t responded to other treatments, they can be life-changing.
What Makes These Drugs Different From Other Osteoporosis Treatments?
Most osteoporosis drugs-like alendronate, risedronate, or denosumab-are antiresorptives. They work by slowing down the cells that break down bone (osteoclasts). That helps preserve what’s left. But teriparatide and abaloparatide do the opposite. They activate the cells that build bone (osteoblasts). Think of it like this: antiresorptives are a brake. These two are an accelerator.
Teriparatide, sold as Forteo, is a synthetic version of the first 34 amino acids of human parathyroid hormone (PTH). It was the first of its kind, approved by the FDA in 2002. Abaloparatide (Tymlos), approved in 2017, is a synthetic analog of a related hormone, PTHrP. While they’re similar in structure, their effects on bone cells aren’t identical. Abaloparatide binds more selectively to a specific shape of the PTH receptor, which researchers believe leads to stronger bone-building signals and less bone breakdown. That small difference has big consequences in real-world outcomes.
Which One Builds Bone Faster?
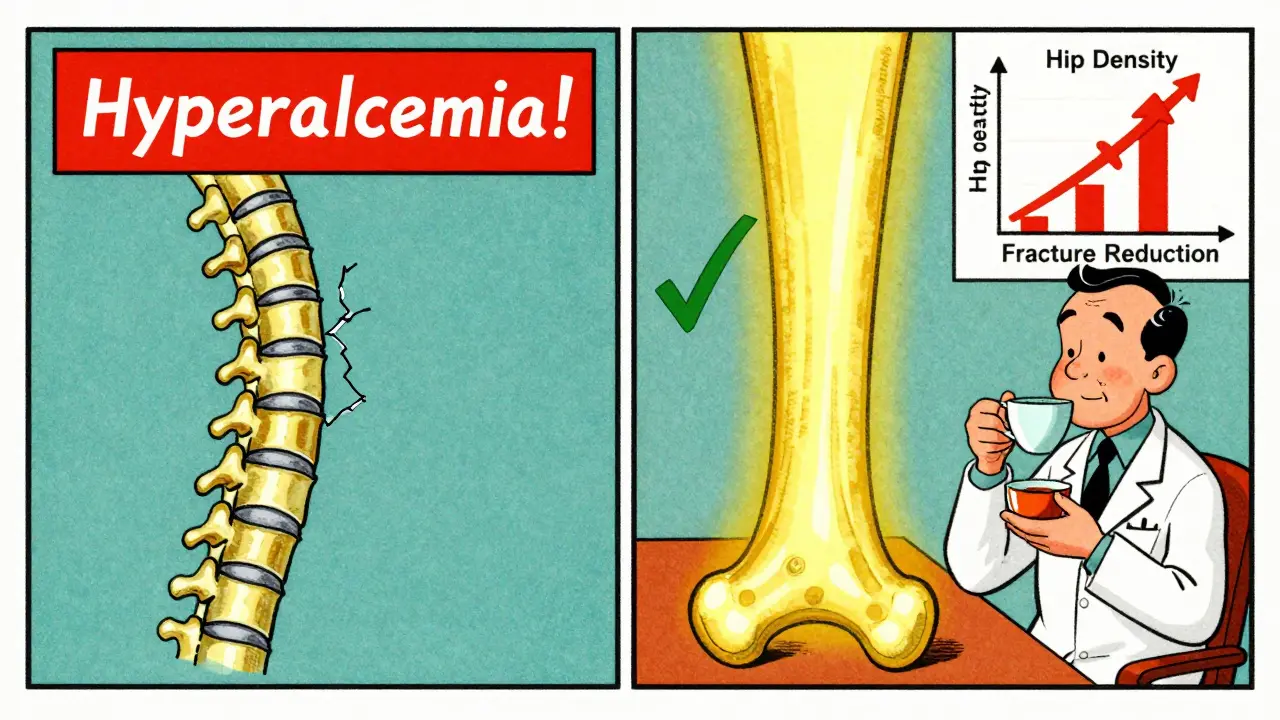
Head-to-head data from the ACTIVE trial, which tracked over 2,400 postmenopausal women over 18 months, gives us the clearest picture. Both drugs improved bone mineral density (BMD), but abaloparatide pulled ahead in key areas.
At the total hip-where fractures are most dangerous-abaloparatide increased BMD by 3.41%, compared to 2.04% with teriparatide. That’s a 1.37% difference. At the femoral neck, the gap was even wider: 2.93% vs 1.49%. Even at the spine, abaloparatide showed faster gains early on, though the difference evened out over time. These aren’t just numbers on a chart. For someone with a hip T-score of -2.7 or lower, these gains mean over a 50% chance of moving out of the osteoporosis range (T-score > -2.5) in just 18 months.
And it’s not just about density. The same trial showed abaloparatide cut new vertebral fractures by 86% compared to placebo, and nonvertebral fractures by 51%. Teriparatide was effective too, but abaloparatide consistently outperformed it in reducing fractures outside the spine.
Why Does Safety Matter More Than You Think?
Both drugs can raise calcium levels in the blood-a side effect called hypercalcemia. It’s usually mild, but it can cause nausea, fatigue, confusion, or even kidney stones. And it’s one of the main reasons people stop treatment.
Here, abaloparatide has a clear edge. In the ACTIVE trial, only 3.4% of abaloparatide users had hypercalcemia, compared to 6.4% on teriparatide. That’s nearly double the risk. Real-world data backs this up. A 2024 claims study of over 43,000 women found that abaloparatide users had 17% fewer cases of high calcium than those on teriparatide. Patient forums echo this: users switching from teriparatide to abaloparatide often report their calcium levels returning to normal within months.
There’s another safety factor: dizziness. About 41% of teriparatide users report feeling lightheaded after injection, especially when standing up too fast. With abaloparatide, that number drops to 29%. It’s not just discomfort-it’s a fall risk. For older adults, even one fall can mean a hip fracture.
Which One Lowers Fracture Risk More?
Bone density is important, but the real goal is preventing fractures. And here, the data is even more telling.
A 2024 retrospective analysis of over 43,000 women found that those on abaloparatide had a 17% lower risk of hip fracture and an 12% lower risk of nonvertebral fractures compared to teriparatide users. That might sound small, but for someone with a history of prior fractures or a T-score below -3.0, every percentage point counts.
What’s more, the ACTIVE-EXTEND follow-up study showed that patients who switched to alendronate after 18 months of abaloparatide maintained those gains. At 3.5 years, 68% still had hip T-scores above -2.5. That’s a powerful combo: build bone fast, then lock it in.
Teriparatide works too, but it doesn’t match abaloparatide’s consistency in reducing nonvertebral fractures. Experts like Dr. Felicia Cosman point out that abaloparatide’s advantage makes it especially valuable for patients who’ve already broken a bone elsewhere-like the wrist or ribs-because those people are at much higher risk for the next one.
Cost and Access: The Hidden Battle
Let’s be honest: cost matters. A lot.
Before 2024, abaloparatide cost around $5,750 per month. Teriparatide? About $4,200. That gap narrowed dramatically in January 2024 when generic teriparatide hit the market. Today, the generic version can cost as little as $2,500 per month. Insurance coverage reflects this: 44% of abaloparatide users report prior authorization denials or high copays, compared to 28% for teriparatide.
For many, the price difference is a dealbreaker. Even if abaloparatide is clinically superior, if your insurance won’t cover it-or your out-of-pocket cost is $1,000 a month-you’re left with few options. That’s why the American Association of Clinical Endocrinologists still recommends teriparatide as first-line for most patients, especially when cost is a factor.
But here’s the twist: if you’re over 65, have a hip T-score below -3.0, or have had a nonvertebral fracture, the clinical benefit of abaloparatide often outweighs the cost. Some patients who switched after hypercalcemia or dizziness with teriparatide say the higher price was worth it.
What About Side Effects and Daily Life?
Both drugs are injected daily under the skin, using pre-filled pens. That’s not easy. Some people struggle with needle anxiety. Others forget. A 2024 survey found that 32% of teriparatide users stopped treatment within a year-mostly because of side effects. For abaloparatide, the discontinuation rate was 24%.
Injection site reactions are common with both. About 68% of teriparatide users report redness or irritation, compared to 52% with abaloparatide. Both require refrigeration (between 2°C and 8°C). If you travel often, that’s a hassle. Both can cause transient low blood pressure when you stand up too fast after injection. The advice is simple: sit or lie down for 30 minutes after each shot.
There’s also a learning curve. The National Osteoporosis Foundation says most patients need 6 to 12 months to get comfortable with the routine. That’s why pharmacies now offer coaching: calling patients to check technique, refill timing, and side effects. It’s not just about the drug-it’s about support.
Who Gets Which Drug?
There’s no one-size-fits-all. But here’s how most specialists decide:
- Choose abaloparatide if: You’ve had a nonvertebral fracture, your hip T-score is -3.0 or lower, you’ve had hypercalcemia on teriparatide, or you’re willing to pay more for better safety and fracture reduction.
- Choose teriparatide if: You’re on a tight budget, your main concern is spine fractures, you haven’t had prior fractures outside the spine, or your insurance won’t cover abaloparatide.
One thing both drugs have in common: they’re not meant to be used forever. The FDA limits both to 18-24 months total lifetime use. After that, you switch to an antiresorptive-usually alendronate or denosumab-to hold onto the bone you built. Studies show this “sequential therapy” works better than using either drug alone.
The Future: What’s Coming Next?
Right now, daily injections are a barrier. But that’s changing. Radius Health is testing a weekly version of abaloparatide. Phase 3 trials finished in late 2023, with results expected in mid-2025. If approved, it could double adherence rates.
Also, the FDA is encouraging research into longer-term anabolic use. The current 2-year limit is based on old rodent studies showing a rare risk of bone cancer. But newer human data shows no increased risk. Experts believe the limit may be lifted in the next few years.
And with the global population aging, demand is rising. By 2030, over 22% of Americans will be over 65. Osteoporosis affects over 10 million in the U.S. alone. Anabolic agents are no longer niche-they’re becoming essential.
Final Thoughts: It’s Not Just About the Drug
Teriparatide and abaloparatide aren’t just medications. They’re tools to rebuild what’s been lost. The choice between them isn’t just clinical-it’s personal. It’s about your fracture history, your finances, your tolerance for side effects, and your willingness to stick with daily shots.
If you’re at high risk for hip fractures, abaloparatide’s data is hard to ignore. But if cost or access is a barrier, teriparatide still delivers real results. Talk to your doctor. Get your bone density tested. Ask about insurance coverage. And don’t assume one is better for everyone. The best choice is the one that fits your life-and keeps you standing.