Clarithromycin is a macrolide antibiotic that inhibits bacterial protein synthesis by binding to the 50S ribosomal subunit. It is widely used in Helicobacter pylori eradication regimens because of its high gastric stability and activity against the organism. When combined with a proton pump inhibitor (PPI) and another antibacterial agent, it forms the backbone of the classic triple therapy for gastritis and peptic ulcer disease. This article walks you through the science, dosing, pitfalls and alternatives, letting both clinicians and patients make informed choices.
Why Helicobacter pylori is the Target
Helicobacter pylori is a gram‑negative, spiral‑shaped bacterium that colonises the stomach lining. Its urease activity neutralises gastric acid, allowing it to survive the hostile environment. Chronic infection triggers inflammation (gastritis) and can erode the mucosal barrier, culminating in peptic ulcers.
Eradicating H. pylori not only heals existing lesions but also reduces the risk of gastric cancer. Studies from European gastroenterology societies (e.g., Maastricht V/Florence Consensus Report 2022) consistently recommend antibiotic‑based therapy as the first‑line approach.
Mechanism: How Clarithromycin Disrupts H. pylori
Clarithromycin binds to the 23S rRNA of the bacterial ribosome, halting peptide chain elongation. This action is bacteriostatic at standard gastric concentrations but becomes bactericidal when paired with an acid‑suppressing PPI that raises stomach pH, facilitating drug penetration.
Importantly, clarithromycin is metabolised by the liver enzyme CYP3A4. Co‑administration with CYP3A4 inhibitors (e.g., certain antifungals) can raise plasma levels, increasing the chance of side‑effects.
Standard Triple Therapy Regimen
The classic regimen, endorsed by most national guidelines, includes:
- Clarithromycin 500mg twice daily
- Amoxicillin 1g twice daily (or metronidazole 500mg twice daily if amoxicillin cannot be used)
- A proton pump inhibitor (e.g., omeprazole 20mg) twice daily
Therapy lasts 14days for most adults. Cure rates exceed 85% in regions with low clarithromycin resistance.
When to Choose Clarithromycin‑Based Therapy
Indications for the clarithromycin triple include:
- Confirmed H. pylori infection via urea breath test, stool antigen, or biopsy.
- No known macrolide allergy.
- Local clarithromycin resistance rates < 15% (data from regional surveillance programs).
If resistance is higher, clinicians often pivot to a bismuth quadruple or levofloxacin‑based regimen.

Antibiotic Resistance: The Growing Challenge
Resistance emerges primarily through point mutations in the 23S rRNA gene, reducing clarithromycin binding. In many parts of Asia and South America, resistance now exceeds 30%.
Routine susceptibility testing is rarely available, so clinicians rely on epidemiological data. When resistance is suspected, the following alternatives are considered.
| Regimen | Key Drugs | Duration | Typical Success Rate* | Major Contra‑indications |
|---|---|---|---|---|
| Clarithromycin Triple | Clarithromycin + Amoxicillin + PPI | 14days | 85‑90% (low resistance areas) | Macrolide allergy, high resistance |
| Levofloxacin Triple | Levofloxacin + Amoxicillin + PPI | 10‑14days | 80‑85% (moderate resistance) | Fluoroquinolone allergy, tendon disorders |
| Bismuth Quadruple | Metronidazole + Tetracycline + Bismuth + PPI | 10‑14days | 90‑95% (high resistance settings) | Pregnancy (tetracycline), severe renal impairment |
*Success rates are average figures from large‑scale meta‑analyses published in 2023.
Dosage Details and Practical Tips
For adults, the standard clarithromycin dose is 500mg taken with food to improve absorption. Children over 12kg may receive 7.5mg/kg twice daily, although pediatric formulations are less common.
Key practical points:
- Take the PPI 30minutes before breakfast and dinner to maximise acid suppression.
- Adhere strictly to the 14‑day schedule - premature stopping is the most common cause of failure.
- Monitor for gastrointestinal side‑effects (nausea, diarrhoea) and hepatotoxicity (elevated liver enzymes).
Side‑Effects and Drug Interactions
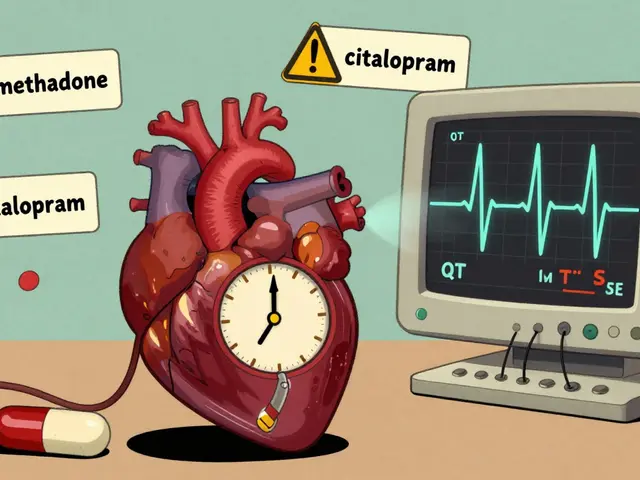
Clarithromycin’s most frequent adverse events are mild: taste disturbances, abdominal discomfort, and occasional rash. Severe reactions, such as QT‑prolongation or hepatotoxicity, are rare but warrant caution, especially in patients on other QT‑prolonging agents (e.g., certain antiarrhythmics).
Because clarithromycin inhibits CYP3A4, it can raise plasma concentrations of statins, some benzodiazepines, and immunosuppressants. Adjust doses or choose alternative antibiotics when these co‑medications are essential.
Related Concepts and Next Steps
Understanding clarithromycin’s role opens doors to broader topics in gastrointestinal pharmacology:
- Proton pump inhibitors - their pharmacodynamics, dosing strategies, and impact on antibiotic efficacy.
- Helicobacter pylori testing - non‑invasive breath tests vs invasive endoscopic biopsies.
- Antibiotic stewardship - how clinicians balance cure rates with the risk of resistance.
- Gastric mucosal healing - the role of mucosal protectants (e.g., sucralfate) after eradication.
Readers interested in the next layer might explore “Bismuth Quadruple Therapy for Resistant H. pylori” or “Managing PPI‑Related Risks in Long‑Term Ulcer Care”.

Frequently Asked Questions
Can clarithromycin be used if I’m allergic to penicillin?
Yes. Clarithromycin itself is a macrolide, not a beta‑lactam, so penicillin allergy does not contraindicate its use. However, if amoxicillin is part of the triple regimen, the doctor may replace it with metronidazole.
How do I know if my H. pylori strain is resistant to clarithromycin?
Direct susceptibility testing is rare in routine practice. Instead, clinicians rely on regional resistance surveillance data. If you live in an area where resistance exceeds 15%, your doctor may choose a different regimen from the start.
Is it safe to take clarithromycin while on a statin?
Clarithromycin can raise statin levels, increasing the risk of muscle injury. If you need both drugs, your physician may switch you to a statin less affected by CYP3A4 (e.g., pravastatin) or temporarily pause the statin during the 14‑day course.
What should I do if I miss a dose?
Take the missed dose as soon as you remember, unless it’s close to the next scheduled dose. In that case, skip the missed pill and continue with the regular schedule. Never double‑dose.
Can I drink alcohol while on clarithromycin therapy?
Alcohol does not directly interact with clarithromycin, but both can irritate the stomach lining. To minimise discomfort and support healing, it’s best to limit alcohol until treatment is complete.




7 Comments
Clarithromycin resistance in India is hitting 40% in some urban centers. I’ve seen patients fail triple therapy three times before we switched to bismuth quadruple. The real issue isn’t the drug-it’s the overuse in respiratory infections. We’re breeding superbugs in primary care clinics and wondering why ulcers won’t heal.
Look, I get that resistance is a problem, but let’s not throw the baby out with the bathwater. Clarithromycin triple is still the gold standard in low-resistance zones like the Midwest US, and for good reason-it’s simple, cheap, and works when you’re not fighting MRSA-level resistance. The real tragedy is how many patients quit after day 7 because they ‘feel better.’ No, you don’t. You’re just letting the tough bugs survive to fight another day. Stick to the full 14 days. Your stomach will thank you. And if you’re on a statin? Talk to your doc. Pravastatin or rosuvastatin are your friends here. Don’t just wing it.
I appreciate how clearly this was laid out. My dad just finished treatment and was terrified of side effects, but the breakdown of alternatives really helped us understand why his doctor chose this path. It’s reassuring to know there are options if it doesn’t work the first time. I hope more people get access to this kind of clarity.
So clarithromycin is effective huh? Interesting how the pharmaceutical industry loves to push these regimens without mentioning that the real cure is diet and stress management. Oh wait they don’t because you can’t patent kale. Also why is everyone assuming H. pylori is always bad? Maybe it’s just trying to balance your microbiome. I’ve heard of people with ulcers who got better after ditching proton pump inhibitors entirely. Just saying.
I’ve been reading up on this since my GI doc recommended the triple therapy last month. I was skeptical at first, especially because I’ve had bad reactions to antibiotics before, but the way this breaks down the alternatives really helped me feel less anxious. I’m on day 10 now-nausea is annoying but manageable, and I’ve been taking the PPI 30 minutes before meals like they said. The table comparing regimens was a game changer. I wish all medical articles were this practical.
Clarithromycin? More like clarithromycin™-the FDA’s little pet project to keep Big Pharma rich. Did you know the 85% success rate only applies in places where they haven’t been dosing chickens with it since 1998? And don’t get me started on CYP3A4-your liver’s screaming for mercy while your statin’s doing a backflip. This isn’t medicine, it’s a controlled experiment with your organs as the test subjects. They’ll tell you to ‘trust the science’ while the resistance rates climb. Wake up. The real cure? Avoid hospitals. Eat fermented foods. And pray.
While the article provides a clinically sound overview, it fails to address the ethical implications of empirical antibiotic prescribing in the absence of susceptibility testing. In resource-constrained settings, the deployment of clarithromycin-based regimens without confirmatory diagnostics constitutes a form of therapeutic nihilism. The Maastricht guidelines are predicated on infrastructure that does not exist in 70% of the world. Without acknowledging this, the recommendation appears not as evidence-based, but as culturally imperialistic.
Write a comment