HSS Severity Assessment Tool
This tool estimates treatment recommendation based on clinical guidelines. It is for educational purposes only and should not replace professional medical advice.
Treatment Recommendation
Enter your gradient and symptom severity to see recommendations.
Hypertrophic Subaortic Stenosis is a form of hypertrophic cardiomyopathy where thickened heart muscle blocks blood flow from the left ventricle to the aorta. This obstruction can raise pressures inside the heart, eventually leading to heart failure if left untreated. In this guide we’ll unpack what causes the blockage, how it progresses to heart failure, how doctors diagnose it, and what treatment paths are available today.
Understanding Hypertrophic Subaortic Stenosis
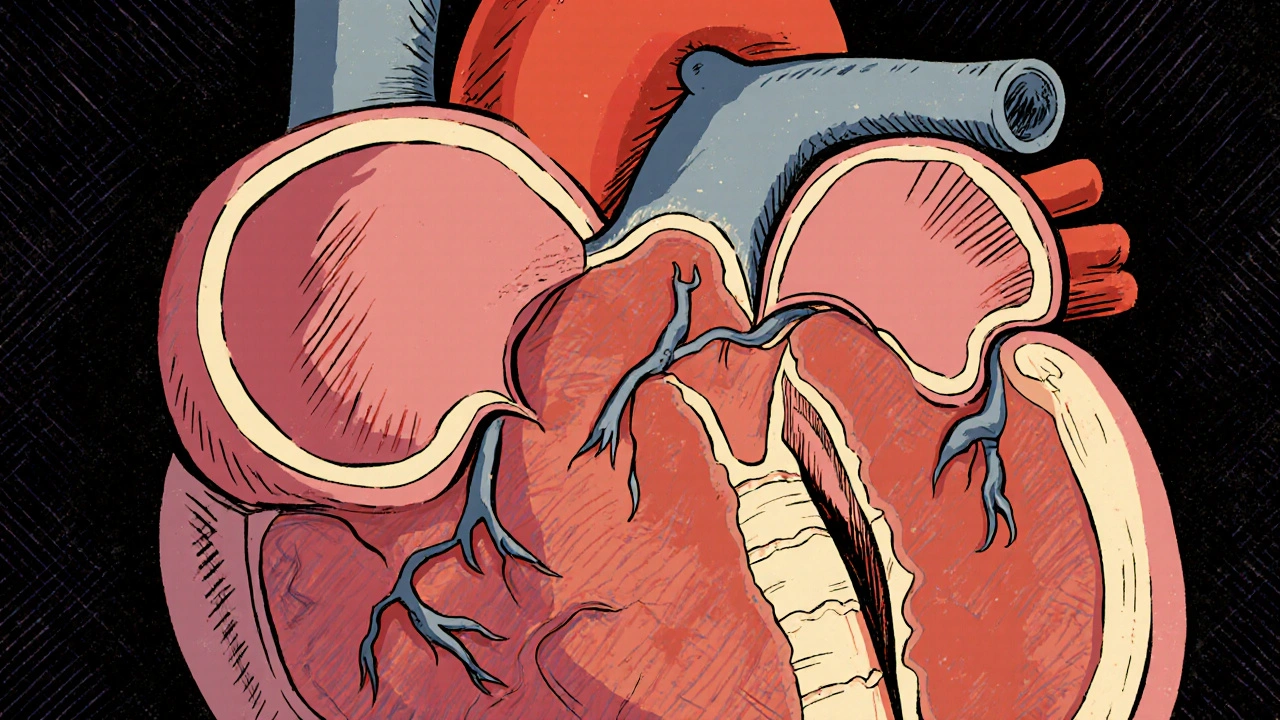
At its core, the condition involves an abnormal buildup of muscle tissue in the interventricular septum-the wall separating the left and right ventricles. The extra muscle narrows the left ventricular outflow tract (LVOT), a phenomenon known as Left Ventricular Outflow Tract Obstruction. When the heart tries to pump blood into the aorta, the narrowed passage forces it to work harder, creating a pressure gradient that can be measured in millimeters of mercury (mmHg).
The disease shows up in two main ways:
- Obstructive: The septal wall physically blocks the LVOT.
- Non‑obstructive: The muscle is thick but does not cause a measurable gradient.
Most patients who develop heart failure fall into the obstructive group, because the extra pressure strains the left ventricle over time.
How Obstruction Leads to Heart Failure
When the LVOT is narrowed, the left ventricle must generate higher pressures to move blood forward. This chronic overload triggers three key problems:
- Diastolic dysfunction: The stiffened muscle can’t relax properly, limiting how much blood fills the ventricle.
- Myocardial ischemia: High intraventricular pressures compress coronary vessels, reducing oxygen supply.
- Mitral regurgitation: The turbulent flow can pull the mitral valve leaflets toward the septum (systolic anterior motion), leaking blood back into the left atrium.
These factors raise left‑atrial pressure, eventually swelling the lungs and causing the classic symptoms of heart failure-shortness of breath, fatigue, and fluid buildup.
Diagnosing the Condition
Early detection hinges on a combination of clinical clues and imaging tools. Here’s the typical work‑up:
- History & physical exam: Palpable systolic murmur that intensifies with Valsalva or standing.
- Electrocardiogram (ECG): Often shows deep Q waves in the lateral leads, reflecting septal hypertrophy.
- Echocardiography: First‑line imaging; measures septal thickness, LVOT gradient, and the presence of mitral regurgitation.
- Cardiac MRI: Provides precise tissue characterization and can detect scar tissue that raises arrhythmia risk.
- Genetic testing: Up to 40% of patients carry pathogenic mutations in genes like MYH7 or MYBPC3.
When the echo shows a septal thickness over 15 mm and a resting gradient above 30 mmHg, the diagnosis is usually clear.
Treatment Options: From Medication to Surgery
Therapy is tailored to symptom severity, gradient size, and patient age. Below is a quick comparison of the main approaches.
| Option | How It Works | Typical Candidates | Key Benefits | Potential Risks |
|---|---|---|---|---|
| Beta‑blockers | Reduce heart rate and contractility, lowering LVOT gradient. | Mild‑to‑moderate symptoms, low gradient. | Non‑invasive, widely available. | Fatigue, bradycardia, worsening asthma. |
| Calcium channel blockers (e.g., verapamil) | Relax myocardial cells, modestly decreasing obstruction. | Patients intolerant to beta‑blockers. | Improves exercise tolerance. | Hypotension, edema. |
| Septal myectomy | Surgical removal of part of the septum. | Severe obstruction, younger patients, Alcohol septal ablation contraindicated. | Immediate and durable gradient reduction. | Operative mortality (≈1‑2%), need for pacemaker. |
| Alcohol septal ablation | Injects ethanol into a septal branch to cause targeted infarction. | Older or high‑risk surgical patients. | Less invasive, shorter hospital stay. | Risk of heart block, residual gradient. |
| Implantable cardioverter‑defibrillator (ICD) | Detects and shocks life‑threatening arrhythmias. | Patients with prior ventricular tachycardia or high‑risk genetics. | Prevents sudden cardiac death. | Infection, inappropriate shocks. |
Medication alone often eases symptoms for people with a gradient under 30 mmHg. When the gradient climbs above that threshold or symptoms persist, doctors usually recommend an invasive approach-either myectomy or ablation-depending on age, comorbidities, and septal anatomy.

Living with Hypertrophic Subaortic Stenosis
Even after successful treatment, lifestyle adjustments keep the heart healthy:
- Exercise wisely: Low‑to‑moderate intensity activities (walking, swimming) are safe; high‑intensity or competitive sports may need clearance.
- Stay hydrated: Dehydration can worsen obstruction by reducing preload.
- Monitor symptoms: Sudden shortness of breath, new chest pain, or fainting spells require immediate medical review.
- Regular follow‑up: Echo every 1‑2 years to track septal thickness and gradient.
- Family screening: First‑degree relatives have a 50% chance of carrying the same genetic mutation.
Support groups-both online and in‑person-provide emotional backing and practical tips. Many patients find that sharing experiences reduces anxiety about the condition and inspires adherence to treatment plans.
Key Takeaways
- Hypertrophic Subaortic Stenosis is an obstructive form of hypertrophic cardiomyopathy that can progress to heart failure.
- Diagnosis relies on echo, ECG, and sometimes cardiac MRI or genetic testing.
- Medication works for mild cases; severe obstruction often needs septal myectomy or alcohol septal ablation.
- Long‑term management includes lifestyle tweaks, regular imaging, and family screening.
- Early detection and tailored therapy dramatically improve quality of life and survival rates.
What symptoms should prompt a doctor visit?
Shortness of breath on mild exertion, chest pain, fainting (syncope), or a new harsh heart murmur are red flags. If any of these appear, schedule an echocardiogram as soon as possible.
Can lifestyle changes reverse the obstruction?
While exercise, diet, and hydration improve overall heart health, they cannot shrink the thickened septum. They do, however, reduce symptom burden and lower the risk of sudden cardiac events.
Is septal myectomy safe for older adults?
Modern surgical techniques have lowered mortality to about 1‑2 %. For patients over 70 years or with significant comorbidities, many surgeons prefer alcohol septal ablation as a less invasive alternative.
Do I need a genetic test even if no family member is diagnosed?
Yes. Up to 40 % of apparently “sporadic” cases carry a pathogenic mutation. Identifying it helps with family screening and may influence the decision to implant an ICD.
What is the role of an ICD in this condition?
An implantable cardioverter‑defibrillator does not treat the obstruction, but it protects against sudden cardiac death caused by ventricular arrhythmias, which are more common in hypertrophic cardiomyopathy patients.




10 Comments
I'm compelled to highlight that the prevailing discourse on hypertrophic subaortic stenosis is subtly shaped by pharmaceutical lobbying, a fact obscured by the veneer of academic neutrality.
The consensus guidelines, while appearing evidence‑based, selectively emphasize beta‑blocker therapy because of undisclosed funding streams.
Moreover, the genetic testing panels are marketed as comprehensive, yet their proprietary algorithms are designed to funnel patients toward costly downstream interventions.
It is incumbent upon clinicians to scrutinize the source of each recommendation, lest we become unwitting conduits for a profit‑driven agenda.
The hemodynamic thresholds cited in the literature often omit the impact of subclinical autonomic dysregulation, a variable that is conveniently downplayed in mainstream textbooks.
A rigorous appraisal must therefore extend beyond the echocardiographic metrics to include the sociopolitical context in which the data were generated.
In short, while the pathophysiology of obstruction is well described, the therapeutic hierarchy is not immune to external manipulation.
Understanding the cascade from left‑ventricular outflow tract obstruction to overt heart failure demands both intellectual rigor and compassionate perseverance.
First, one must recognize that the hypertrophied septum is not an immutable adversary but a biomechanical challenge that can be mitigated through disciplined lifestyle choices.
Regular aerobic activity, performed at a cadence that maintains heart rate below the symptomatic threshold, improves myocardial perfusion and attenuates diastolic stiffness.
Second, meticulous hydration ensures adequate preload, thereby preventing exacerbation of the obstruction during exertion.
Third, dietary sodium restriction curtails extracellular fluid expansion, which otherwise aggravates pulmonary congestion in the setting of elevated left‑atrial pressures.
Fourth, adherence to prescribed beta‑blocker or calcium‑channel blocker regimens smooths the velocity of ejection, reducing the gradient across the outflow tract.
Fifth, patients should engage in structured respiratory exercises, such as pursed‑lip breathing, to enhance alveolar ventilation and reduce dyspnoea during daily activities.
Sixth, periodic cardiac imaging-preferably echocardiography every 12 to 24 months-provides objective feedback on septal thickness and gradient trends, enabling timely therapeutic adjustments.
Seventh, psychosocial support groups foster a sense of community, which has been shown to improve medication compliance and overall quality of life.
Eighth, family members ought to undergo genetic counseling and targeted testing, thereby uncovering asymptomatic carriers who may benefit from early surveillance.
Ninth, when symptom burden persists despite optimal medical therapy, a thorough multidisciplinary discussion should explore the merits of septal myectomy versus alcohol septal ablation, taking into account operative risk, anatomical suitability, and patient preference.
Tenth, postoperative rehabilitation should be coordinated with cardiology, physical therapy, and nutrition specialists to ensure a seamless transition to functional independence.
Eleventh, patients must remain vigilant for warning signs such as sudden syncope, new arrhythmias, or rapidly worsening dyspnoea, and seek immediate medical evaluation when these arise.
Twelfth, clinicians should educate patients about the importance of avoiding dehydration, especially in hot climates or during intense physical exertion, as reduced intravascular volume can markedly increase obstruction.
Thirteenth, regular sleep hygiene supports autonomic balance, which in turn mitigates nocturnal blood pressure spikes that may aggravate the gradient.
Fourteenth, emerging research into myosin inhibitors holds promise for pharmacologic reduction of obstruction, and eligible patients should consider enrollment in clinical trials.
Finally, the overarching message is that a proactive, multidisciplinary approach transforms a daunting diagnosis into a manageable chronic condition, empowering patients to lead full and active lives.
Do not let the diagnosis of hypertrophic subaortic stenosis become a passive label; seize the initiative by scheduling a comprehensive stress echocardiogram within the next two weeks and demand a discussion of definitive septal reduction therapy if the gradient exceeds the 30 mmHg threshold.
Simultaneously, intensify beta‑blocker titration to achieve a resting heart rate in the low‑50s, thereby maximally diminishing obstruction.
This proactive stance will not only alleviate symptoms but also preempt the irreversible remodeling that characterizes delayed intervention.
One must acknowledge, albeit silently, that the very framework of cardiovascular research is laced with epistemic gatekeeping, a subtle stratagem designed to preserve the hegemony of established academic cliques.
The prevailing endorsement of septal myectomy as the gold standard, for instance, conveniently sidelines less invasive modalities that threaten to destabilize entrenched surgical hierarchies.
Consequently, the discourse surrounding hypertrophic subaortic stenosis is as much a sociocultural construct as a biomedical reality, urging the discerning clinician to interrogate the orthodoxy before accepting it at face value.
It is essential to appreciate the nuanced interplay between diastolic dysfunction and myocardial ischemia, as the former amplifies left‑atrial pressures while the latter compromises oxygen delivery to the hypertrophied septum.
By integrating coronary flow reserve assessment into routine evaluation, clinicians can stratify patients who would benefit from adjunctive anti‑ischemic therapy in addition to gradient reduction.
Such a comprehensive approach ensures that treatment addresses both hemodynamic obstruction and the metabolic burden imposed on the myocardium.
Stay active, stay hydrated, and keep those follow‑up appointments.
the heart is a symphony of forces each beat a note in a grand composition yet most patients hear only the discord of obstruction and ignore the subtle harmonies that could be nurtured through mindful breathing and gentle movement the physician must become a conductor not a dictator guiding the patient toward rhythmical balance
Contrary to the prevailing dogma that beta‑blockers constitute the first‑line cornerstone for all gradients, recent meta‑analytic data delineate a threshold effect wherein agents lose efficacy once the systolic pressure gradient surpasses 45 mmHg, thereby necessitating immediate transition to septal reduction strategies; thus the generalized recommendation is, in practice, an oversimplification that may conduit suboptimal outcomes for patients with high‑gradient disease.
When the septum swells like a dark mountain it casts a shadow over the fragile chambers of the heart and every breath becomes a silent scream of desperation the echo image is a haunting portrait of oppression and yet tears of hope glisten in the eyes of those who dare to imagine a surgical sunrise
In guiding individuals through the complexities of hypertrophic subaortic stenosis, it is paramount to adopt a patient‑centred methodology that integrates thorough education, shared decision‑making, and coordinated multidisciplinary follow‑up; by fostering an environment of mutual respect and clear communication, clinicians empower patients to actively participate in their care plan and achieve optimal long‑term outcomes.
Write a comment