Anticholinergic Burden Calculator
What is Anticholinergic Burden?
Anticholinergic burden measures the total impact of medications that block acetylcholine, a brain chemical crucial for memory and heart function. Higher scores increase risk of cognitive decline and cardiac issues.
ACB Scale: 0 = No effect, 1 = Low, 2 = Moderate, 3 = High (highest risk)
Your Current Risk
When you take a tricyclic antidepressant like amitriptyline or nortriptyline for depression or chronic pain, you might not realize you’re also loading your body with a hidden risk-one that can slowly blur your memory, slow your thoughts, and even mess with your heart rhythm. These drugs were once the go-to treatment for depression, but today, they come with a warning label most people never see: anticholinergic burden. And for people over 50, especially those taking multiple medications, that burden can be dangerous-even irreversible.
What Is Anticholinergic Burden?
Anticholinergic burden isn’t a single drug side effect. It’s the total impact of all the medicines in your system that block acetylcholine, a key brain chemical needed for memory, attention, muscle control, and heart regulation. Tricyclic antidepressants (TCAs) are among the strongest offenders. They were designed to boost serotonin and norepinephrine, but along the way, they also slam shut muscarinic receptors in the brain and body. That’s why a single dose of amitriptyline gets the highest possible score-3-on the Anticholinergic Cognitive Burden (ACB) Scale. That’s the same level as some bladder meds and old-school allergy pills. When you stack TCAs with other anticholinergic drugs, the effect multiplies.Why Your Memory Might Be Fading
If you or a loved one has started forgetting names, struggling to follow conversations, or feeling foggy after starting a TCA, it’s not just aging. Research from JAMA Internal Medicine tracked over 3,400 adults over 65 for seven years and found those taking high-anticholinergic drugs had a 54% higher chance of developing dementia. And it’s not just correlation-stopping the drug doesn’t always bring memory back. In some cases, the damage sticks around for years. Clinicians have seen this play out repeatedly. Patients come in with suspected dementia, but after stopping amitriptyline, their cognition improves within months. One Reddit thread from psychiatrists described multiple cases where elderly patients were wrongly diagnosed with Alzheimer’s-until their TCA was pulled. Their symptoms? Dry mouth, confusion, trouble finding words. Classic anticholinergic effects. Not dementia. Just drug-induced.Cardiac Risks You Can’t Ignore
It’s not just your brain. TCAs also mess with your heart. They act like Class 1A antiarrhythmics-drugs meant to treat irregular heartbeats-but without the safety controls. Amitriptyline can stretch out your heart’s QT interval, the time between beats. A prolonged QT can lead to torsades de pointes, a life-threatening arrhythmia. At therapeutic doses, QRS duration can increase by 10-25%. In overdose, it jumps to 50% or more. That’s why ER doctors treat TCA overdoses as medical emergencies. Compare that to SSRIs like sertraline or escitalopram. They have near-zero anticholinergic scores and don’t stretch the QT interval the same way. Studies show amitriptyline carries 2.8 times the risk of QT prolongation compared to sertraline. For someone with existing heart disease, high blood pressure, or a family history of sudden cardiac events, that’s not a small difference. It’s a red flag.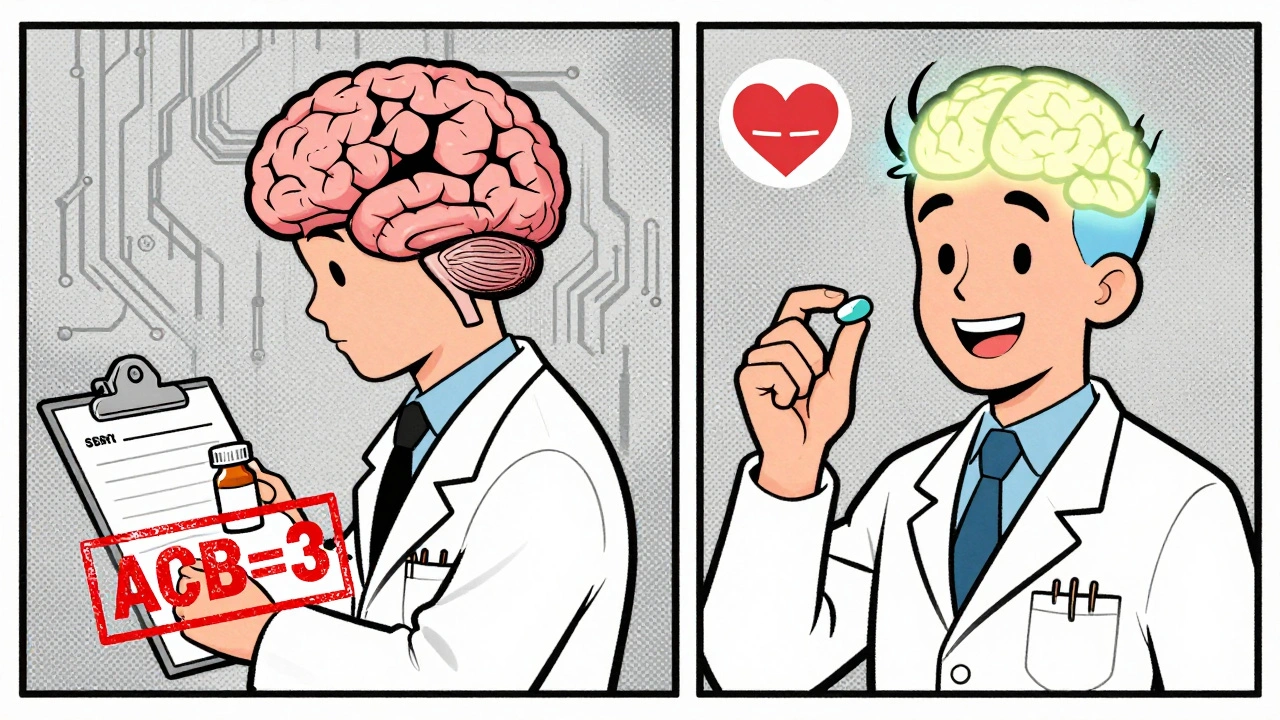
Who’s Most at Risk?
It’s not just the elderly. Anyone over 50, especially those on multiple medications, is vulnerable. A 2022 survey by the National Council on Aging found that 68% of adults over 65 taking TCAs had at least two anticholinergic side effects. Dry mouth? Common. Constipation? Routine. Blurred vision? Expected. But cognitive decline? That’s the silent killer. And it’s often missed because doctors focus on the depression, not the side effects. Even over-the-counter meds add up. If you’re taking diphenhydramine (Nytol®) for sleep or chlorphenamine (Piriton®) for allergies, you’re adding to the burden. One patient in an AARP forum described needing nightly artificial saliva and daily laxatives just to manage side effects from nortriptyline. That’s not normal aging. That’s drug toxicity.Alternatives That Work Better-and Safer
You don’t have to suffer through side effects to treat depression or neuropathic pain. Serotonin-norepinephrine reuptake inhibitors (SNRIs) like duloxetine and venlafaxine have ACB scores of 0 or 1. They’re just as effective for pain and depression, with far fewer brain and heart risks. SSRIs like escitalopram and citalopram are even cleaner. Cognitive behavioral therapy (CBT) has strong evidence for both depression and chronic pain, with no side effects at all. For treatment-resistant depression-where TCAs once ruled-there are now options like ketamine nasal spray, transcranial magnetic stimulation (TMS), and newer agents like vortioxetine. None carry the same anticholinergic weight.What Should You Do?
If you’re on a TCA, don’t stop cold turkey. Withdrawal can cause dizziness, nausea, and mood crashes. But you can work with your doctor to safely taper off. Nortriptyline is slightly less potent than amitriptyline, so switching might help-but the goal should be to move to a safer alternative. Ask for an ACB score calculation. Most UK electronic health systems now have tools built in that auto-calculate your total anticholinergic load. If your score is 3 or higher, it’s time to have a real conversation. Ask: “Is this drug still necessary? What are the alternatives? Could my memory issues be from this?” NICE guidelines now say: minimize anticholinergic drugs during dementia assessments. That’s not just advice-it’s a standard of care. If your doctor hasn’t mentioned this, it’s your right to ask.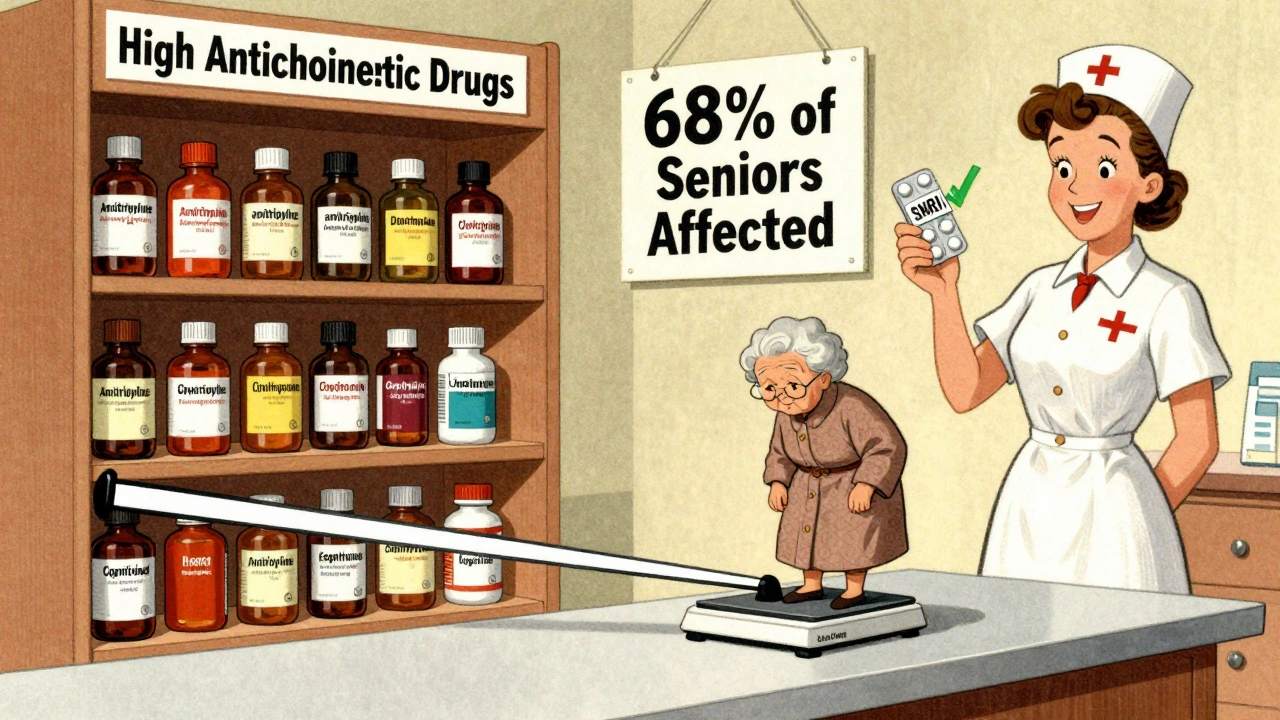
Deprescribing Works
In NHS Somerset, a structured program helped reduce anticholinergic burden in 78% of older patients. Six months after stopping TCAs, 63% showed measurable cognitive improvement. Their MMSE scores went up. Their confusion lifted. Their dry mouth eased. One woman, 72, said: “I started remembering where I put my keys again. I didn’t realize I’d forgotten how to do that.” The trend is clear. In the U.S., TCA prescriptions for depression dropped from 15% in 2000 to under 5% in 2020. New antidepressants approved since 2010 are almost all low-anticholinergic. The Beers Criteria, used by doctors to avoid unsafe meds in older adults, now lists TCAs as “potentially inappropriate” unless no other option exists.It’s Not About Fear-It’s About Choice
TCAs aren’t evil. They helped people before safer drugs existed. For a small group-those with treatment-resistant depression or severe neuropathic pain who’ve tried everything else-they still have a place. But for most, the risks far outweigh the benefits. Your brain and heart aren’t interchangeable parts. Once damage sets in, it doesn’t always reverse. The real question isn’t whether TCAs work. It’s whether you need to pay that price.Can tricyclic antidepressants cause dementia?
Yes. Long-term use of high-anticholinergic drugs like amitriptyline and nortriptyline has been linked to a 54% increased risk of dementia over seven years, according to a major study in JAMA Internal Medicine. These drugs interfere with acetylcholine, a brain chemical critical for memory. In some cases, cognitive decline improves after stopping the drug, but not always-damage can be permanent.
Do all antidepressants have anticholinergic effects?
No. Tricyclic antidepressants (TCAs) are among the worst offenders, with a score of 3 on the ACB scale. Most modern antidepressants like SSRIs (e.g., sertraline, escitalopram) and SNRIs (e.g., duloxetine) have scores of 0 or 1, meaning minimal to no anticholinergic activity. Even some older drugs like mirtazapine have lower scores than TCAs.
How do I know if I’m taking a high-anticholinergic drug?
Check your medication list against the Anticholinergic Cognitive Burden (ACB) Scale. Amitriptyline and nortriptyline are both ACB=3. Common over-the-counter drugs like diphenhydramine (Nytol®) and chlorphenamine (Piriton®) are also ACB=2 or 3. Ask your pharmacist or GP to calculate your total ACB score. If it’s 3 or higher, you’re at increased risk.
Can I stop taking a TCA on my own?
No. Stopping abruptly can cause withdrawal symptoms like dizziness, nausea, anxiety, and even rebound depression. Always work with your doctor to taper slowly-usually over 4 to 8 weeks. Your doctor can help you switch to a safer alternative like an SSRI or SNRI while managing your original condition.
Are there any safe alternatives to TCAs for chronic pain?
Yes. Duloxetine and venlafaxine (SNRIs) are effective for neuropathic pain and have minimal anticholinergic effects. Non-drug options like cognitive behavioral therapy (CBT), physical therapy, and mindfulness-based stress reduction also have strong evidence. For some, gabapentin or pregabalin may be appropriate, though they carry their own risks. Always discuss alternatives with your doctor before switching.
Next Steps If You’re on a TCA
- Write down every medication you take-including vitamins, sleep aids, and allergy pills.
- Ask your GP or pharmacist to calculate your total ACB score.
- If your score is 3 or higher, ask: “Is this drug still necessary? What are the safer alternatives?”
- Don’t stop suddenly. Work with your doctor on a tapering plan.
- Monitor for changes in memory, balance, or heart rhythm. Report them immediately.




13 Comments
I had no idea my nightly Benadryl was adding to the brain fog 🤯 My grandma kept forgetting where she put her glasses and we thought it was Alzheimer’s - turns out it was the amitriptyline + sleep aid combo. Stopped both, she’s back to telling stories from the 70s like it was yesterday.
this is so real i was on nortriptyline for back pain and started forgettin names of my own kids 😭 my doc never mentioned any of this. switched to duloxetine and my brain feels like it woke up from a 5 year nap
We treat depression like it’s a broken pipe you fix with one wrench but the brain isn’t plumbing it’s a symphony and every drug you throw in changes the harmony. TCAs were the brass section blasting at full volume - effective yes but deafening. Now we have violins and flutes that still play the melody without shattering the windows. We’re not abandoning the old, we’re evolving the orchestra.
People think doctors are just handing out pills like candy but if you’re over 50 and on 6 meds including that sleepy-time diphenhydramine you’re basically running a pharmacological experiment on yourself and then blaming aging when your memory goes. Stop being passive and start asking for your ACB score. It’s not hard.
It is imperative to recognize that the accumulation of anticholinergic agents within the geriatric pharmacological regimen constitutes a significant and underappreciated iatrogenic risk factor for neurocognitive decline. The reduction of such burden through deprescribing protocols, as demonstrated in NHS Somerset, yields statistically significant improvements in MMSE scores and functional autonomy, thereby affirming the necessity of systematic review in polypharmacy management.
America is soft. You guys take one pill and suddenly your brain is melting. In my day we took whatever the doctor gave us and didn’t complain. Now everyone’s checking ACB scores like it’s a Yelp review. Just suck it up and get back to work
The ACB scale is a game changer. I’m a geriatric pharmacist and I’ve seen patients go from ‘I can’t remember my grandkids’ names’ to ‘I finally remembered my wedding anniversary’ after tapering off TCAs. It’s not magic - it’s neurochemistry. And the cardiac risks? Same story. QT prolongation isn’t theoretical - I’ve seen the EKGs. SSRIs and SNRIs aren’t just safer, they’re smarter. Why risk a stroke when you can get relief without the collateral damage?
my mom was on amitriptyline for 12 years and never told me she was so confused. when we switched her to venlafaxine she started cooking again and remembered how to use the microwave. i wish i’d known about this sooner. if you’re on a TCA talk to your doc. dont wait til its too late
I’m so glad this is getting attention. I work with seniors and so many of them are on these meds because it’s what their doctor prescribed decades ago and no one ever checked. We had a woman who thought she had dementia - turned out her ACB score was 5. After switching and cutting out the OTC sleep aid? She started gardening again. That’s not recovery. That’s resurrection.
The clinical evidence is compelling, and the epidemiological data from longitudinal cohorts such as the one published in JAMA Internal Medicine cannot be dismissed. The pharmacodynamic profile of TCAs, particularly their affinity for muscarinic receptors, directly correlates with the observed cognitive trajectory. The notion that these effects are reversible in all cases is misleading; neuroplasticity has limits, and prolonged cholinergic suppression may induce structural changes. Deprescribing is not merely prudent - it is ethically incumbent.
Ugh. Another article making people paranoid about their meds. My doctor knows what he’s doing. I’m not going to stop something that helps my depression just because some blog says it’s ‘dangerous’. You people are so scared of everything now. Just let people live.
You’re not alone. I was on nortriptyline for 8 years and felt like I was walking through fog. I thought it was just me getting older. Then I talked to my doctor and switched. Now I remember my kids’ birthdays. I remember where I put my keys. I remember who I am. Don’t wait until you’re lost. Ask. Talk. Change. You deserve to feel like yourself again 💪❤️
It’s funny how we treat the body like a machine you can upgrade with new software when the truth is we’re still figuring out what the operating system even is. We replaced TCAs not because we knew better but because we had shiny new toys. But maybe the old drugs weren’t wrong - maybe we just didn’t understand the cost. And now we’re pretending the cost doesn’t exist because it’s easier than admitting we made a mistake. The brain doesn’t forgive easily. And neither should we.
Write a comment