Antibiotic Resistance Explained: How It Affects You
Antibiotic resistance is when bacteria stop responding to medicines that used to kill them. It sounds like a lab story, but it shows up in everyday clinics, hospitals, and even at home. When a drug doesn’t work, infections linger longer, treatments get more expensive, and the risk of serious illness grows.
Why Bacteria Become Resistant
Bacteria are tiny, but they learn fast. Every time you take an antibiotic, the drug kills the bacteria it can, but a few may survive. Those survivors copy their resistant traits and pass them on to the next generation. Over time, the whole population can become tough to treat.
Two main habits drive this process. First, using antibiotics for viral infections like colds or flu. Viruses don’t need antibiotics, so the medicine just pressures the bacteria in your body for no good reason. Second, not finishing a prescribed course. Stopping early leaves the strongest bugs alive, giving them a chance to multiply.
Other factors add fuel. In farms, antibiotics are sometimes added to animal feed to keep animals healthy and grow faster. The cheap, low‑dose exposure creates a breeding ground for resistant germs that can jump to people through food or the environment.
How You Can Help Slow It Down
You have a lot of power to keep antibiotics working. If you get a prescription, take the whole dose exactly as your doctor says. Even if you feel better after a few days, finish the pack.
Never ask for antibiotics for a cold, sore throat, or any illness that looks viral. Trust your doctor’s judgment – they know when a drug will actually help.
Practice good hygiene. Wash your hands often, cover coughs, and keep wounds clean. Preventing infections reduces the need for antibiotics in the first place.
If you’re buying animal products, look for labels that say “no antibiotics added” or “raised without antibiotics.” Choosing those options cuts down the spread of resistant bugs from farms.
Stay current on vaccinations. Flu shots, pneumonia vaccines, and other immunizations stop infections before they start, meaning fewer chances to need antibiotics.
Finally, talk to your pharmacist or doctor if you’re unsure about a prescription. Ask what the drug does, how long you need to take it, and what side effects to watch for. That conversation can protect you and the community.
Antibiotic resistance isn’t a problem for scientists only – it’s a everyday issue that we can all help manage. By using medicines wisely, staying clean, and choosing foods thoughtfully, you play a key role in keeping these life‑saving drugs effective for years to come.

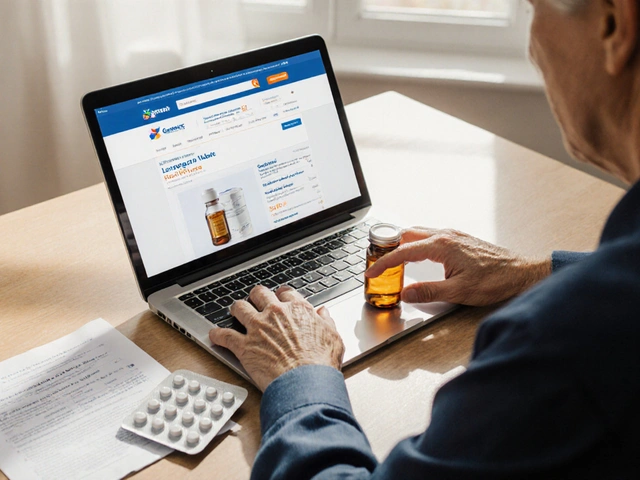
Norfloxacin’s Role in Treating Recurrent Urinary Tract Infections
- By : Tamsin Riverton
- Date : Aug 1 2025
Explore how norfloxacin works, when it’s suitable for recurrent UTIs, dosing tips, resistance concerns, and alternatives for safer long‑term care.